-
PDF
- Split View
-
Views
-
Cite
Cite
P Mhandu, S Chaubey, H Khan, R Deshpande, Unusual presentation of a chondrosarcoma as an anterior mediastinal mass, Journal of Surgical Case Reports, Volume 2012, Issue 4, April 2012, Page 1, https://doi.org/10.1093/jscr/2012.4.1
Close - Share Icon Share
Abstract
Chest wall chondrosarcomas are a rare cause for an anterior mediastinal mass. Commonly patients present with a painless palpable mass with a third of patients describing diffuse chest pain. We present a patient with an anterior mediastinal chest wall chondrosarcoma presenting with neurological symptoms and flushing. As more of these cases are seen and reported this rare entity is more likely to be considered in the differential diagnosis under appropriate circumstances.
INTRODUCTION
Chest wall chondrosarcomas are a rare cause for an anterior mediastinal mass. We present the interesting case of a young male patient who presented with neurological symptoms from the mass. Although chondrosarcoma is considered the most common primary malignancy of the chest wall and sternum, it is a rare lesion with an incidence of 0.5 chest wall chondrosarcomas per million people per year. Approximately 75% of chest wall chondrosarcomas arise from the costochondral junction of the ribs and sternum.
CASE REPORT
A 26 year old male presented with sudden onset of severe shortness of breath and headache, more intense on the right side while swimming. This was associated with tunnel vision in his left eye, facial flushing and numbness on the left side of his face and down his left arm. On clinical examination he was found to have a murmur and investigation with a chest X-ray (CXR) (Fig 1A) revealed a large mediastinal mass which was causing significant displacement of the trachea to the right. A subsequent computed tomography (CT) (Fig 1B) scan demonstrated a large superior mediastinal mass, which was extending down into the anterior mediastinum and compressing the right ventricular outflow tract (RVOT) of the heart. A Doppler study with transthoracic echocardiogram showed the RVOT to have a systolic gradient of 60 mmHg and was the most probable source of the murmur. After discussion at the multidisciplinary meeting it was decided to proceed with surgery.
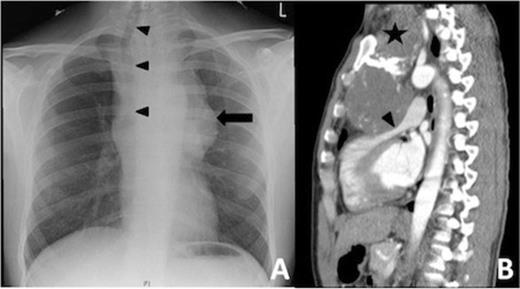
Patient CXR (Figure 1A) with a large shadow (black arrow) of the mass in the superior mediastinum. Due to its size the trachea was displaced far to the right (black arrow head). Sagital views of the CT scan (Figure 1B) showed the mass (black star) in the superior mediastium extending inferiorly into the anterior mediastinum causing obstruction of the right ventricular outflow (black arrow head). The aortic arch was also pushed posteriorly.
In theatre before the skin incision was made the patient desaturated probably due to the complete obstruction of the RVOT by the mass. An urgent sternotomy was performed with immediate relief of the RVOT compression, achieving complete stability in the patient’s clinical status. Initial inspection of the mass showed that it was stuck to the posterior of the sternum and the left sternoclavicular joint. Vessels stalks originating from the subclavian artery and directly from the aorta were supplying the mass. These were ligated and the entire mass was removed. There were no evidence of cervical or mediastinal lymphadenopathy. Following the successful debulking of the mass the patient made good postoperative recovery with no neurological deficit.
Histological examination (Fig 2) showed the mass to be a chondrosarcoma (grade 1). It appeared to be arising from the posterior aspect of the sternum and the left sterno-clavicular joint. However the tumour was seen to be extending to the excision margins. Hence despite the tumour having been successfully debulked the positive excision margins made it necessary to keep the patient under careful vigilance with initial six monthly imaging. At the 3 monthly follow up the patient was doing well and was devoid of any symptoms he had described before his operation.
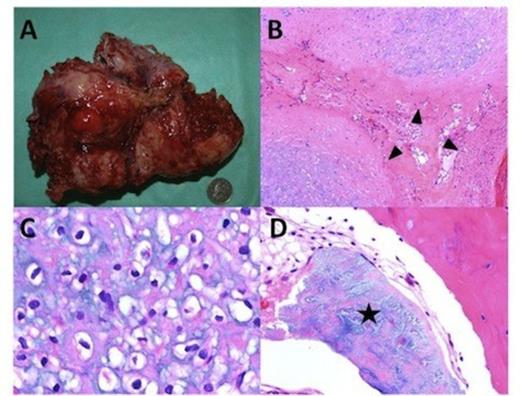
A 170x120x70 mm mass weighing 675 grams was removed. (Figure 2A) The mass was lobulated (Figure 2B) with the lobules separated by thick collagenous bundles (black arrow head). The tumour cells comprised of mature chondrocytes (Figure 2C) which showed minimal atypia. No necrosis or mitoses was seen. However metaplastic bone formation (Figure 2D) was observed (black star). These findings were consistent with those of a well differentiated chondrosarcoma.
DISCUSSION
Although chondrosarcomas are considered the most common primary malignancy of the chest wall and sternum, it is nevertheless a rare lesion as reported in the literature. They are more common in men within there fifth and sixth decade of life (1,2,3)
Patients with chest chondrosarcoma can present with a variety of symptoms depending on tumour size and location. 75% of chest wall chondrosarcomas arise from the costochondral junction between the ribs and sternum as was observed in our case. Sternal chondrosarcoma can present as a slowly growing mass, as in the presented case, producing dyspnoea. Lesions can invade within the medullary bone resulting in the destruction of the anterior and posterior cortical margins. These features were not observed in our case with only a mild abnormality observed along its posterior cortical surface of the sternum. A review of 106 patients with chest wall chondrosarcoma by Windhe et al (3) found that the most common presentation was with a painless palpable mass. Thirty two per cent of patients reported diffuse chest pain while in thirteen per cent of patients the chondrosarcoma was an incidental finding. None of the patients reported periods of fever, pain at night, weight loss or general illness. The case presented here first came to medical attention due to neurological symptoms. Though it is not possible to explain all the patient’s symptoms with the presence of the sternal chondrosarcoma the patient remains symptom free at his 3 month follow-up, suggesting the mass was the direct or indirect cause of his symptoms.
Given the patient’s young age the other possible differential diagnosis considered by the authors was that of a germ cell tumour which produce 10% to 15% of anterior mediastinal tumours in young adults. Sixty to seventy percent of these tumours comprise of mature teratomas. Other differential diagnosis of an anterior mediastinal mass, which one could consider include a thymoma, thymic carcinoma, lymphoma especially the nodular sclerosing subtype of Hodgkin’s disease which has a predilection for the anterior mediastinum and Castleman disease which is an uncommon entity in which giant lymph node hyperplasia involves the thorax in 70% of patients.
Our case highlights the importance of considering a chondrosarcoma in the differential diagnosis of an anterior mediastinal mass despite a nonconforming clinical presentation.
The keys to successful treatment are early recognition and radical excision with adequate margins, as chondrosarcoma is relatively resistant to radiotherapy and conventional cytotoxic chemotherapy (4). Complete resection of the tumour has shown 100% survival after 5 years compared to 75 % with incomplete resection. Wide surgical resection was attempted as local recurrence is common with incomplete excision usually after 3-years (3,5). The patient has now been referred to a specialist sarcoma centre for further surveillance and treatment.
Our case highlights the unusual presentation of a rare tumour. The case emphasises the importance of considering it in the differential diagnosis of chest wall tumours. The greater awareness of this possibility will hopefully shorten the time to diagnosis and allow for more planned treatment.



