-
PDF
- Split View
-
Views
-
Cite
Cite
A Pereira, M Massada, R Sousa, R Lemos, Metastatic carcinoma as an unusual cause of failure in total hip arthroplasty, Journal of Surgical Case Reports, Volume 2012, Issue 3, March 2012, Page 9, https://doi.org/10.1093/jscr/2012.3.9
Close - Share Icon Share
Abstract
Evaluation of osteolysis after total hip arthroplasty remains a challenge. It may reflect a myriad of problems: from wear-debris induced lesions to infection, metabolic bone disease or even malignant infiltration. We present the clinical, radiographic and pathological features of a 64-year-old woman in whom loosening and failure of total hip arthroplasty occurred secondary to a periacetabular metastasis from a previously undiagnosed lung carcinoma.
INTRODUCTION
Periprosthetic osteolysis is the most common complication after total hip arthroplasty and is seen with increasing frequency due to the growing number of arthroplasties and lifetime of the implants(1). Most of the time the bone loss is due to wear-mediated inflammation that ultimately can lead to aseptic loosening of cemented and uncemented devices, but may reflect a late change of an infectious process and more rarely an infiltration of a primary or metastatic tumor (2,–,4).
We present a case of a patient whose acetabular component loosening was secondary to a neoplastic process and not to a benign condition as it would be expected and thought. The purpose of this report is to highlight the potential for malignancy to mimic septic and aseptic loosening and to include it in the differential diagnosis in the failing hip arthroplasty in order to avoid caveat revision arthroplasty (5,6).
CASE REPORT
A 64-year-old woman presented with right hip pain of mixed characteristics with few months of evolution. She has had a fracture of the neck of the femur (Garden IV) after a fall nine years before, and undergone total hip arthroplasty with a cementless device (ART stem and ALIZE cup from Biomet, Warsaw, Indiana, USA). The patient followed our standard protocol for evaluation of pain after total hip arthroplasty, with plain radiographs and inflammatory markers (C-reactive protein and erythrocyte sedimentation rate). The inflammatory markers were within the normal range and comparing past and present radiographs there were signs of cup instability with osteolysis lines larger than 2 mm in zones I and II of De Lee and Charnley (Fig 1).
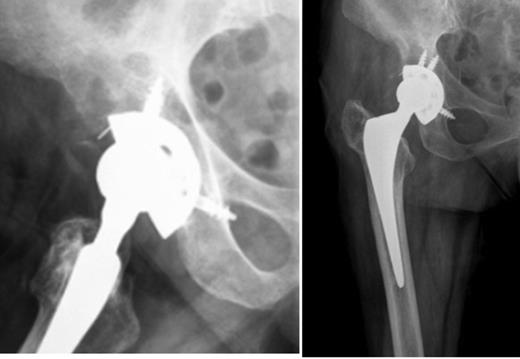
Right hip radiographs (lateral and AP) at the initial evaluation with osteolysis in zones I and II of De Lee and Charnley suggestive of cup loosening
Given these findings, it was interpreted as aseptic loosening of the acetabular component and the patient was proposed for revision surgery. Two months later, when the patient was admitted for surgery, there was onset of right hip pain out of proportion associated with inability to walk, weight loss and respiratory symptoms. We asked for new pelvic and hip radiographs that showed an extensive osteolytic lesion with neoplastic appearance (Fig. 2).
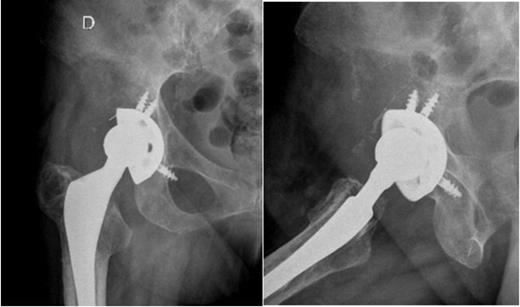
Right hip radiographs (AP and lateral) at the admission, two months later, with an extensive osteolytic lesion in the right iliac wing
The patient was then studied to investigate the location of the primary tumor, and thoracic radiographs and CT scan revealed a central nodular lesion in the left lung that biopsy, subsequently, confirmed to be a non-small cell carcinoma. The tumor was staged as a T2N3M1b in the TNM classification after the staging exams. Of course there was a change in terms of prognosis and guiding therapy and the patient was referred for palliative radiotherapy for pain control. The patient died 7 months after the histological diagnosis.
DISCUSSION
Although very rare, tumors have been reported in literature in relation to total joint prosthesis. They are generally primary, mostly sarcomas, and are more common in the proximal femur (7–8). To date, there are few reports documenting the occurrence of metastatic infiltration as cause of failure of total hip arthroplasty, and only one report of cup loosening secondary to metastatic carcinoma (5,–,9). Our case of cup loosening from metastatic infiltration but from a primary tumor of unknown aetiology is the first to be reported. In most cases, the diagnosis of malignancy is made by histology after revision surgery to treat presumed septic or aseptic loosening. Similarly, are described in the literature arthroplasties undertaken to treat presumed non-neoplastic disorders, which are later determined to be secondary to extra-articular tumors – caveat arthroplasty (6). In retrospect, all this shows that it is necessary to draw attention to this possibility so that a systematic approach might be helpful. The clinical history and examination must include a scrutiny of atypical symptoms and signs, risk factors and past diseases. Periprosthetic osteolysis must be carefully evaluated in relation to the presence of accompanying symptoms, duration, progression, cortex invasion and number of lesions (10). If pain or progressive osteolysis is noted, septic loosening must be ruled out, and inflammatory markers, hip aspiration and technetium bone and indium leukocyte scans should be performed (10). If there are still suspicious and atypical findings, biopsy must be considered.
Even if osteolysis is a common finding and almost always a benign problem, one must be open to other diagnostic possibilities that are potentially more serious. Therefore, a review of the history, physical examination and imaging must be done, and biopsy must be considered if there are suspicious findings. This is the only way to avoid subduing the patient to an unnecessary revision surgery whose aggressiveness and consequences might be highly painful.



