-
PDF
- Split View
-
Views
-
Cite
Cite
CR Baker, P Bhagwat, A Wan, Mesenteric paraganglioma with gallbladder paraganglion nest, Journal of Surgical Case Reports, Volume 2012, Issue 3, March 2012, Page 8, https://doi.org/10.1093/jscr/2012.3.8
Close - Share Icon Share
Abstract
We report on an original case of a 64 year old lady diagnosed with an extraadrenal mesenteric paraganglioma associated with an incidental histological finding of a gallbladder paraganglion. Paragangliomas are rare neuroendocrine, neural crest-derived tumours, found in diverse locations and display variable catecholamine secreting behaviour. Malignant potential can be difficult to predict on histology. We review the current literature on these multifarious tumours.
INTRODUCTION
Paragangliomas are rare chromaffin cell tumours that derive from neural crest origin. Intraabdominal paragangliomas are most commonly phaeochromocytomas of the adrenal medulla, while extraadrenal paragangliomas can arise in diverse locations. We present a case of a mesenteric paraganglioma with a subsequent finding of a small paraganglion cell nest within the gallbladder.
CASE REPORT
A 64 year old lady was admitted with a short history of abdominal pain. Her past medical history included an ERCP for choledocholithiasis and hypertension. CT scanning revealed a 3.3cm mass within the small bowel mesentery and a shrunken gallbladder. (Figure 1 a, b). The mass enhanced avidly and heterogeneously, with arterial supply from the superior mesenteric artery.

CT Scan showing 3.3 cm avidly enhancing mass (arrow) in the small bowel mesentery with arterial supply from the superior mesenteric artery (A) horizontal and (B) coronal section
Laparoscopy was performed with conversion to a lower midline laparotomy because of dense adhesions. Following adhesiolysis, a 4×3cm soft vascular mass was found in the terminal ileum mesentery. The mass was removed intact, without need to perform a small bowel resection. The patient made an uncomplicated recovery.
The mesenteric mass was a variegated tan colour, with areas of focal haemorrhage and surrounded by ectatic blood vessels (Figure 2). Microscopically, the tumour was made up of nests of polygonal cells with vesicular non-nucleolated nuclei and strikingly clear cytoplasm (Figure 3). There was scanty mitotic activity and immunohistochemical staining was positive for neuroendocrine markers chromogranin, synaptophysin and CD56. There was close association with delicate capillaries and S100 positive sustentacular cells. Appearances were consistent with an extraadrenal paraganglioma.

Macroscopic appearance of section through mesenteric paraganglioma
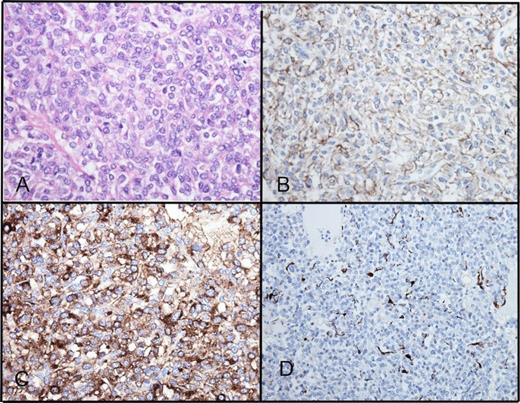
Histology of mesenteric paraganglioma. (A) H&E x400, (B) CD56 immunostaining, (C) chromogranin immunostaining, (D) S100 immunostaining of sustentacular cells
Further investigations included 24-hour urinary catecholamines, which were negative on two occasions. MRI showed no evidence of further disease and six months later, CT scanning showed no evidence of recurrence. As the patient had ongoing right upper quadrant pains, an elective cholecystectomy was performed. Gallbladder histology showed features of chronic cholecystitis. In addition, within the wall was a small (<1mm) nodule of polygonal cells arranged in small nests surrounded by a single layer of thin delicate spindle cells [Figure 4]. Appearances and immunohistochemistry were consistent with a paragangliomatous rest. The patient is well with no evidence of recurrence three years following surgery.
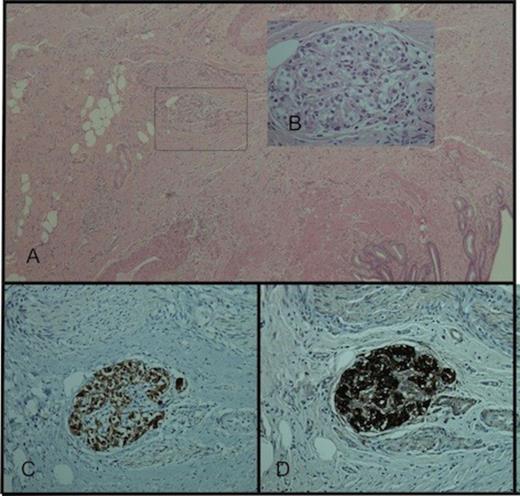
(A) Paraganglion cell rest within the gallbladder wall. H&E staining ×40, (B) H&E staining ×400, (C) synaptophysin immunostaining ×200, (D) chromogranin immunostaining ×200
DISCUSSION
Paraganglioma is the term used to describe tumours originating from neural crest-derived cells that disperse widely to form parasympathetic and sympathetic ganglia of the autonomic nervous system (1). Parasympathetic-associated paragangliomas arise in head and neck, often described by their site of origin e.g. carotid body tumours and rarely secrete catecholamines. Sympathetic paragangliomas have a greater propensity for secretion and are divided into pheochromocytomas of the adrenal medulla and extra-adrenal paragangliomas. The later makeup 5-10% of sympathetic tumours and have been described in diverse locations (2).
The incidence of paragangliomas is 1-2/100,000 (1). Although the majority are sporadic, germline mutations have been identified in up to 30% (3). Hereditary conditions associated include MEN2, von Hippel-Lindau, neurofibromatosis type 1 and familial paraganglioma phaeochromocytoma syndromes with mutations identified in at least six distinct genes (RET, NF1, VHL, SDHB, SDHC and SDHD). In the case of the rare familial paraganglioma/pheochromocytoma syndromes, mutations are found in genes encoding the succinate-dehydrogenase enzyme complex of the mitochondrial electron transport chain. The mechanism of tumourigenesis is unknown, but theories include chronic activation of hypoxia sensing pathways and impairment of apoptosis (4).
Isolated paraganglionic cell collections have been described in diverse locations (5). Sympathetic paragangliomas can be found along the sympathetic chain and sympathetic plexus of the bladder, kidneys, mediastinum and heart. There have been eight reports of paraganglioma arising from the mesentery (6). Seven of these cases were, as in our patient, arising from the small bowel mesentery and one in the mesentery of the descending colon.
There have been seven reports of gallbladder paragangliomas, all asymptomatic, and four cases described in relation to the biliary system (7). This is the first description of paraganglioma tissue described in both gallbladder and mesentery. The small paraganglion rest was found within the gallbladder wall and is unlikely to represent a metastasis from the previously resected tumour.
Most paragangliomas are diagnosed in the 4th or 5th decade and can be an incidental finding, by screening on family history or due to symptoms from either mass effect or catecholamine secretion. One of the largest series is from the Mayo Clinic with most presenting as incidental findings or mass effect and only 20% catecholamines (8).
If suspected, a detailed family history should be obtained and measurement of plasma or urinary metanephrines or catecholamines performed. For imaging, both CT and MRI are sensitive, but there are no pathognomonic features. In general, these tumours appear as heterogeneous masses and, whether functional or nonfunctional, are highly vascularised. Metaiodobenzylguanidine (MIBG) is a catecholamine analogue, taken up by 90% of paragangliomas and is used for localisation (123I-MIBG) and therapy (131I-MIBG) (9). These scans are specific, although sometimes lack sensitivity. 18F-FDG-PET scanning can be used in identification of metastases. Biopsy should not be performed due to the risk of precipitating a hypertensive crisis, bleeding or tumour seeding.
The histological prediction of malignant behaviour is difficult - the presence of metastatic disease being the only diagnostic feature. Malignancy is more likely in extra-adrenal, larger, less differentiated tumours (10). Whereas 10-26% of phaeochromocytomas are malignant, intra-abdominal extra-adrenal paragangliomas have higher malignant potential (up to 50%), with spread possible to lymph nodes, liver and lung.
The treatment for the majority of paragangliomas is surgical resection. If evidence of catecholamine secretion, α and β-blockade should be commenced preoperatively. In the presence of metastasis, 5 year survival is 50% (1). Postoperative follow up if secretory should include plasma or urinary metanephrines, initially after 3-6 months and then yearly. For non-secretory cases, appropriate imaging should be performed.
In summary, preoperative diagnosis of extraadrenal paraganglioma can be difficult due to the variable presentation, location and lack of characteristic findings on imaging. In the presence of a highly vascular lesion, especially along the paravertebral axis, it is prudent to arrange screening for urinary metanephrines. Once resected, the risk of malignancy can be difficult to judge from the histology, often only diagnosed following the development of metastatic disease.



