-
PDF
- Split View
-
Views
-
Cite
Cite
S Tatebe, K Oka, S Kuraoka, Intramural bronchogenic cyst of the oesophagus, Journal of Surgical Case Reports, Volume 2012, Issue 10, October 2012, Page 3, https://doi.org/10.1093/jscr/2012.10.3
Close - Share Icon Share
Abstract
Bronchogenic cysts are relatively common mediastinal cysts. Here, we report removal of a rare paraoesophageal-type bronchogenic cyst by video-assisted thoracoscopic surgery in a 52-year-old male patient. The defect of the oesophageal wall was successfully reinforced with an intercostal muscle flap.
INTRODUCTION
Bronchogenic cysts, usually located in the lung or mediastinum, are due to bronchopulmonary foregut malformations and are relatively common congenital cysts in the mediastinum. However, paraoesophageal-type cysts, i.e., those buried completely in the oesophageal wall, are rare. We report successful removal of an intramural bronchogenic cyst in the oesophagus by video-assisted thoracoscopic surgery (VATS).
CASE REPORT
A 52-year-old man was referred due to an abnormal shadow on routine chest X-ray. His medical history included above-the-knee amputation of the left leg due to a traffic accident. He reported mild dysphagia when ingesting solid food. Physical findings were unremarkable. Computerized axial tomography (CAT) scan showed a posterior mediastinal mass compressing the oesophagus, and magnetic resonance imaging (MRI) revealed high signal intensities on both T1 and T2 weighted images suggestive of bronchogenic cyst (Fig. 1).

T1 preoperative magnetic resonance imaging - high intensity signal lesion was found in the posterior mediastinum, suggestive of a bronchogenic cyst

T2 preoperative magnetic resonance imaging - high intensity signal lesion was found in the posterior mediastinum, suggestive of a bronchogenic cyst
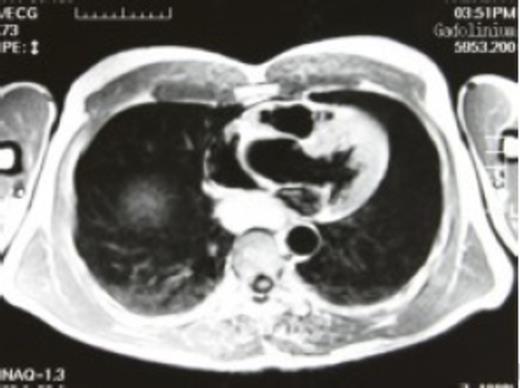
Gadolinium enhanced preoperative magnetic resonance imaging - high intensity signal lesion was found in the posterior mediastinum, suggestive of a bronchogenic cyst
Under general anesthesia in the left lateral position, a thoracoscopic approach was utilised to evaluate and remove the lesion. A cyst was found within the oesophagus wall. The oesophagus wall was carefully dissected, and the cyst was successfully excised. There were no fistulas between the oesophagus and the cyst. Care was taken to avoid breaching the mucosa of the oesophagus, and intraoperative oesophagogastroscopy with a flexible fiberoptic scope confirmed there was no oesophageal injury. Initially, the defect of the oesophageal wall was repaired with sutures, which resulted in mild stenosis of the oesophagus. Some sutures were removed, and a pedicled intercostal muscle flap was prepared to cover the defect completely. All procedures were carried out by VATS with three ports, with a small incision extended to facilitate harvesting the intercostal muscle flap. The cyst measured 30–20–12 mm and had ciliated epithelium, confirming the diagnosis of a bronchogenic cyst. The patient's postoperative course was uneventful, but he felt that ingested food remained in the oesophagus. These symptoms subsided gradually without treatment. Barium swallow tests in the perioperative period showed dilatation of the lower oesophagus, which recovered to almost normal within 4 years (Fig. 2).


DISCUSSION
This case report described successful excision of a paraoesophageal-type bronchogenic cyst by VATS. Management in this case involved a number of issues, including the difficulty in preoperative diagnosis of a paraoesophageal bronchogenic cyst as distinct from an oesophageal cyst (1). Both bronchogenic and oesophageal cysts originate from the foregut, which also makes preoperative diagnosis difficult, and definite diagnosis can be obtained only by pathological examination. CAT scan shows only the cystic nature of the lesion, and the diagnosis remains uncertain in cases in which the mass has high protein and/or calcium contents. MRI has been considered useful in diagnosis of bronchogenic cysts, as shown in the present case, although it provides no information regarding the relation to adjacent organs or tissues. Endosonography has potential for accurate preoperative diagnosis. However, at present no methods are available to obtain a definitive diagnosis of paraoesophageal bronchogenic cyst (2).
Advances in technology and the development of new and better equipment have led to increases in the efficacy of thoracoscopy in diagnosis as well as surgical treatment. VATS has a number of advantages in that it is a less invasive method with better postoperative recovery and shorter hospital stay than conventional surgery.
Complete removal is essential to avoid bronchogenic cyst recurrence, and this is possible by VATS even in para-oesophageal-type lesions as in the present case (3,4). However, in some cases with a fistula between the oesophagus and the cyst, it is necessary to leave a small amount of cyst tissue close the fistula in place. Although there are no specific risks associated with VATS, special care is needed to avoid breaching the mucosa of the oesophagus, which is also required in conventional surgery. Therefore, intraoperative oesophagogastroscopy was performed with a flexible fiberoptic scope in this case to examine the fistula or oesophageal injury. In addition, we reinforced the defect of the oesophageal wall with an intercostal muscle flap. In most cases reported previously, the defect was repaired directly by suturing, and no follow-up was described. Initially we repaired the defect with sutures, but found stenosis of the oesophagus. Some sutures were then removed and a pedicled intercostal muscle flap was applied. Slight dilatation of the oesophagus was noted postoperatively, which was corrected almost completely within several years. Although we do not feel that the muscle flap is absolutely necessary, it is effective in cases with a relatively large oesophageal wall defect or in cases with stenosis by suturing alone. The port incision was extended in this case to harvest the intercostal muscle, which may have been unnecessary.



