-
PDF
- Split View
-
Views
-
Cite
Cite
S Davey, F Alam, S Malik, A delayed presentation of cardiac tamponade after blunt trauma, Journal of Surgical Case Reports, Volume 2011, Issue 9, September 2011, Page 1, https://doi.org/10.1093/jscr/2011.9.1
Close - Share Icon Share
Abstract
Cardiac tamponade is a recognised complication of blunt trauma to the chest. It usually presents at the time of the acute event but there are rare cases of delayed presentations. We present such a case where the tamponade occurred six weeks following the trauma to the chest wall.
INTRODUCTION
We present a case of a patient with cardiac tamponade, who presented with symptoms six weeks after the initial blunt trauma to his chest.
CASE PRESENTATION
A 63-year-old male presented to the Emergency Department, short of breath and feeling generally unwell for 2 days prior to admission. Six weeks prior to admission, he had fallen off a ladder and fractured 2 ribs in the right hemi-thorax.
He was assessed in the emergency department and sent home with analgesia. Four weeks later he was seen by his GP feeling “chesty” and was treated with a short course of antibiotics for a suspected lower respiratory tract infection.
Two days prior to admission, the patient felt increasingly unwell, with the symptoms of being cold and clammy at times. He also had pleuritic chest pain with shortness of breath. He had right lumbar and right upper quadrant pain, with the latter being more dominant.
On admission to the ED, he was hypotensive (70/50), tachycardic (112) but maintaining his oxygen saturations in air (100%) and was afebrile. He was appropriately resuscitated.
Chest and abdominal plain film x-rays demonstrated healing rib fractures, with no consolidation, pneumo-thorax or haemo-thorax.
He remained slightly tender in his right upper abdomen and lumbar regions but looked generally unwell (sweaty, pale and restless). He was still cold and clammy. As a result of his persistent hypotension, tachycardia, partial response to resuscitation and acidosis on the arterial blood gases, a CT scan was arranged.
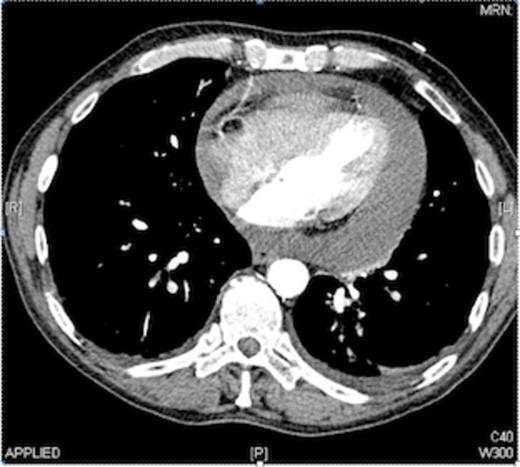
The CT findings were a moderate to severe pericardial effusion, with a fluid rim of approximately 2 cm, around the whole pericardium (as shown in Fig. 1).
The effusion was drained under ultrasound guidance. 900mls of blood stained fluid was aspirated. His blood pressure improved dramatically and stabilised, the patient felt immediately better, his breathing eased, and his shortness of breath settled.
DISCUSSION
This case study appears to be the first report of cardiac tamponade that presented 6 weeks after the initial blunt injury. A search on PubMed (“delayed cardiac tamponade blunt trauma”) gave 28 results, of which only 4 were reports of delayed cardiac tamponade as opposed to other pathologies.
Of these four, one presented 4 weeks after minor trauma to the chest (1). A second case, presenting three weeks (2) after blunt trauma, was believed to have developed secondary the commencement of an anticoagulant treatment. The remaining two cases (3,4) were at 2 weeks and eight days respectively.
It is therefore clear that this presentation at six weeks is rare. In this case, other causes (cancer, uraemia, spontaneous cardiac rupture and recent heart surgery) were excluded.
This case does demonstrate the need to have an index of suspicion of cardiac tamponade in patients presenting with symptoms and signs of being unwell, even if the insult (blunt chest trauma) was sustained a few weeks prior to their presentation.



