-
PDF
- Split View
-
Views
-
Cite
Cite
A Mason, J Gahir, S Kadirkamanathan, Oesophageal xanthalasma with Barrett’s Oesophagus and Menetrier’s Disease, Journal of Surgical Case Reports, Volume 2011, Issue 4, April 2011, Page 9, https://doi.org/10.1093/jscr/2011.4.9
Close - Share Icon Share
Abstract
This case report describes three conditions; oesophageal xanthalasma, Menetrier’s disease and Barrett’s oesophagus, none of which have ever been seen together, diagnosed in one patient. Further to the details of the case the endoscopic, radiological and histological findings are discussed. Any links between these three conditions are currently unclear.
INTRODUCTION
This patient was found to have oesophageal xanthalasma and Barrett’s oesophagus on endoscopy, and was then shown to have Ménétrier’s disease on endoscopic ultrasound. There have been no previous cases of a patient with oesophageal xanthalasma and Barrett’s oesophagus, with oesophageal xanthalasma and Ménétrier’s disease or with Ménétrier’s disease and Barrett’s oesophagus.
This case shows three conditions, two of which very rare, none of which have ever been previously reported together.
CASE PRESENTATION
A 63 year old gentleman presented to a colorectal outpatient appointment in July 2009. He presented with a 3 month history of diarrhoea. He was found to have a normocytic anaemia, which had improved after being prescribed ferrous sulphate. He had a past medical history of dyspepsia, which was managed with lansoprazole; diabetes mellitus type 2 and hypercholesterolaemia. There was no significant family history.
On examination the abdomen was soft and non-tender. PR examination and all other examination findings were unremarkable.
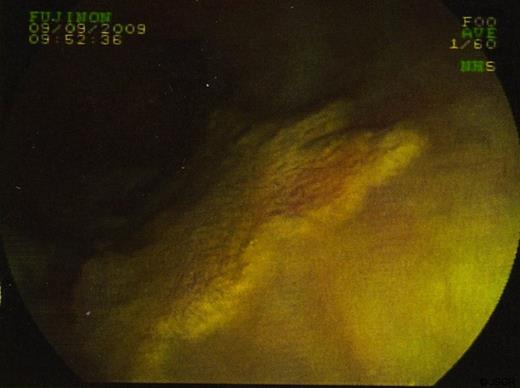
In September 2009 the patient underwent a colonoscopy and oesophagogastroduodenoscopy (OGD). Colonoscopy was unremarkable. However, views of the oesophagus on OGD showed what was thought to be a superficially spreading tumour, 35cm from the incisors and 5 cms in length. Barrett’s oesophagus was also seen. (figure 1 & 2)

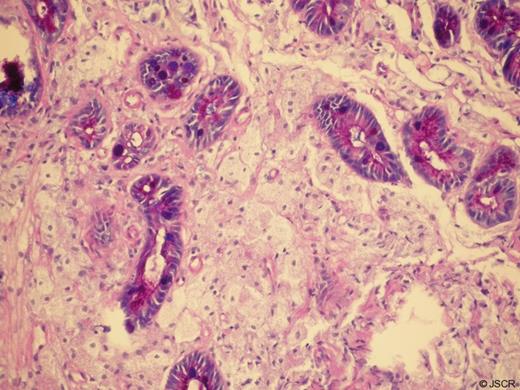
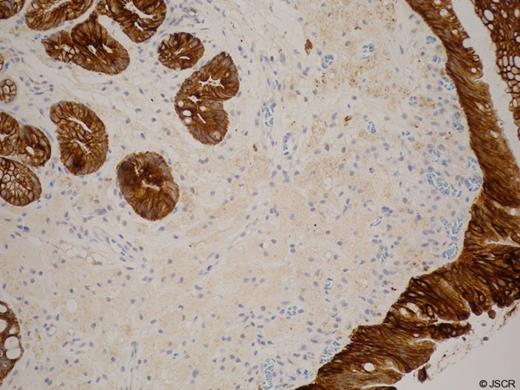
Biopsies were taken and sent to histopathology. In some sections the cells viewed had small bland nuclei with foamy cytoplasm. They were negative for mucin stain and negative for epithelial markers. There was no dysplasia or malignancy. This picture was consistent with xanthalasma. Other biopsies of surrounding tissue showed a picture consistent with Barrett’s oesophagus. (Figure 3 & 4)
Endoscopic ultrasound examination showed an area of xanthalasma proximal to the oesophago-gastric junction in segments of Barrett’s mucosa. There were no enlarged lymph nodes. The gastric mucosa was shown to be diffusely thickened suggestive of Ménétrier’s disease.
The patient had a CT scan of the chest abdomen and pelvis which showed thickening of the gastric body and fundus supporting the diagnosis, with no lymphadanopathy or signs of malignancy.
In the future the patient will be monitored with surveillance endoscopy.
DISCUSSION
Xanthaloma can be found anywhere along the gastrointestinal tract. It is more often found in the stomach and colon and is rare in the oesophagus and small intestine. Only seven cases of oesophageal xanthalasma have previously been reported, the first being described by Remmele and Engelsingin in 1984. (1)
Of the cases reported in the oesophagus, the majority were found to be in the lower third2 a finding that is consistent with this case. Three of the previous cases of reported oesophageal xanthalasmas seen have been solitary lesions (2,3), as is this one. Previous xanthalasma patches have been reported as being between 1 and 10 mm in length, this xanthalasma was seen to be 50 mm on OGD, much larger than those previously reported.
Xanthaloma in the oesophagus is a rare finding on OGD causing it to be misdiagnosed in many cases. In this case endoscopic ultrasound did not add much to the process of diagnosing xanthaloma. The most important diagnostic tool is biopsy and histology.
Ménétrier’s disease is a rare idiopathic precancerous disorder more commonly affecting men and those aged 30 – 60. There is thickening of the gastric folds of the gastric body with mucous gland metaplasia and increased production of mucus. As the disease progresses there is a reduction in parietal cells, actually reducing acid secretion. There has been no proven medical treatment for Ménétrier’s disease although the patient may undergo subtotal gastectomy if the condition is severe. The patient would also require surveillance as there is an associated risk of stomach cancer. (4)
Barrett’s oesophagus is a premalignant condition caused by repeated reflux of gastric contents into the oesophagus. It is found in approximately 1% of the adult population and 3-5% of the population with GORD. (5) The increase risk of developing adenocarcinoma is 35 – 125 times that of the general population. (6) Treatments include medical treatment to reduce acid secretion such as H2 blockers of proton pump inhibitors, or in some cases surgical intervention such as fundoplication or resection may be recommended.
Oesophageal xanthalasma has never before been reported with Barrett’s oesophagus or Ménétrier’s disease, it is likely that in this case they are incidental findings as there is currently no known aetiology linking the conditions together. The increase in mucus production and decrease in acid secretion in Ménétrier’s disease makes the never before reported finding of this disease together with Barrett’s oesophagus surprising.



