-
PDF
- Split View
-
Views
-
Cite
Cite
P Mekhail, A Saklani, M Philobos, AG Masoud, Thigh subcutaneous emphysema: is that a clear indication for thigh exploration?, Journal of Surgical Case Reports, Volume 2011, Issue 2, February 2011, Page 1, https://doi.org/10.1093/jscr/2011.2.1
Close - Share Icon Share
Abstract
Thigh subcutaneous emphysema is an usual orthopaedic presentation normally associated with musculoskeletal problems or penetrating wounds. But, sometimes it can be related to abdominal pathology. We present a case of subcutaneous emphysema of the thigh secondary to para-caecal abscess.
INTRODUCTION
Upper thigh subcutaneous emphysema manifested by swelling, crepitus and cellulitis is a common orthopaedic presentation, usually related to underlying musculoskeletal problem or penetrating wound. In a few situations, this can be related to abdominal pathology rather than limb pathology and most of these cases are usually associated with significant morbidities and possible mortality.
We present a case of subcutaneous emphysema of the thigh secondary to para-caecal abscess. This was managed by laparotomy alone for abdominal pathology without the need for surgical debridement or thigh exploration.
CASE REPORT
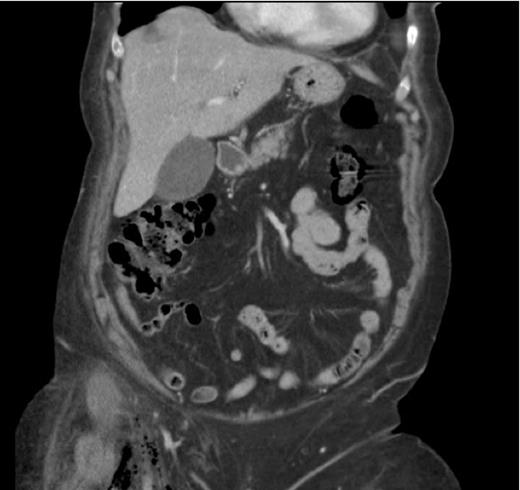
A 75- year old female was admitted as an emergency with right iliac fossa pain. She was afebrile. Bloods on arrival showed leukocytosis of 18.6 and CRP of 235.5. Clinical examination was inconclusive. During her over-night stay, she developed tachycardia and hypotension which responded to fluids. On review, abdominal examination revealed fullness in the right iliac fossa. More importantly she developed swelling and redness of the right thigh. The patient had a CT abdomen, pelvis and upper thigh that showed gas containing fluid collection in the right iliac fossa in keeping with either diverticular or appendicular abscess (Figure 1). It also showed inferior extension of the gas into the right ilio-psoas muscle, groin and upper thigh (perivascular) raising the possibility of necrotising fasciitis (Figure 2).

On laparotomy, an abscess was found in close proximity to a caecal mass. The abscess cavity was entered and a right hemicolectomy was performed. Residual tip of the appendix was found in the abscess cavity. There was no pus tracking retroperitoneally or along the psoas muscle and the muscle looked healthy. A needle aspiration from the swollen upper thigh did not reveal any pus. Most likely cause of the subcutaneous emphysema in thigh was thought to be gas in the abscess cavity tracking along fascial planes. No exploration of the thigh was performed and the plan was to review the thigh swelling the next day. However, this settled down completely following laparotomy alone.
Post operative histology revealed acute perforated appendicitis with peri-appendicular abscess. Post operatively the patient recovered well, no further surgery was done and the patient went home after a slow convalescence.
DISCUSSION
Retroperitoneal and psoas abscesses are possible complications following gastrointestinal perforation. This collection can trickle down by gravity along fascial planes posterior to the inguinal ligament and both of them can lead to subcutaneous emphysema and possibly thigh abscess (2,3,4,5). Perforated appendix is the commonest cause of bowel-related right thigh emphysema, whereas on the left side it is usually caused by diverticular disease or perforated rectal cancer (2,3,4,5). Due to the nature of the disease enteric flora are usually detected but chances of developing gas gangrene is usually remote (4). The subcutaneous emphysema may result from several mechanisms: first many of the colonic flora are gas producing, and perhaps more important passage of intestinal gas from gastrointestinal tract in to tissues as the result of positive gradient between bowel lumen and subcutaneous space (5). The diagnosis like in our case is often delayed or missed due to paucity of localising signs. If no necrotic tissue or dead muscle is found next to primary pathology, provided that primary pathology is treated timely, subcutaneous emphysema of the thigh may herald a benign course. On the other hand if necrotic muscles are found in the abdomen or pus tracks in to the thigh, exploration of thigh is mandatory to ensure complete debridement and to avoid missing necrotising infections of the thigh.
In our case the patient was managed conservatively (without thigh exploration) as once the abdominal pathology has been treated, the thigh subcutaneous emphysema started to improve with antibiotics and with close monitoring of the patient.
Subcutaneous emphysema of the thigh, secondary to abdominal pathology when associated with healthy psoas muscle is a condition that follows a benign course. This can be treated conservatively without exploration of the thigh as long as the abdominal pathology is promptly managed. Good imaging modalities including CT and MRI are strongly recommended when the underlying pathology of the thigh subcutaneous emphysema is not clear.



