-
PDF
- Split View
-
Views
-
Cite
Cite
Reinou Groen, Samuel Sesay, Adam Kushner, Sheiku Dumbuya, Three-stage repair of a giant inguinal hernia in Sierra Leone: A management technique for low-resource settings, Journal of Surgical Case Reports, Volume 2011, Issue 12, December 2011, Page 8, https://doi.org/10.1093/jscr/2011.12.8
Close - Share Icon Share
Abstract
In this report we discuss the clinical management of a giant inguinal hernia (GIH) in Sierra Leone where surgical resources are severely limited. Though possibly not appropriate for more heavily resourced areas, a three-stage repair proved to be effective and safe for the management of this condition.
Careful explanation, good planning and staged operations may be needed for the repair of GIH in low resource settings and we therefore encourage that they be treated by experienced personnel who are able to secure follow up of the patient. The management of GIH is complicated by the potential of abdominal compartment syndrome and respiratory distress if the hernia is reduced suddenly.
INTRODUCTION
Giant inguinal hernias (GIH) are rarely encountered in high income countries; however, in low resource setting such conditions present more frequently often do to a lack of patient knowledge, trust in the health system, or funds to pay for treatment. Additionally, in low income countries, resources may preclude management that is the hallmark of more resourced environments where a pneumoperitoneum is used to increase the capacity of the abdominal cavity and a mesh is used for definitive repair (1,2).
In Sierra Leone, a small West-African country with a population of 6 million and only 10 surgeons (3), the presentation of a GIH is less of a surprise. A noted aphorism is that in Africa there are only two types of hernias: above the knee and below the knee. The reality in clinical practice, however, where there are many cases of incarcerated and sliding hernias, is that true GIH, defined as a sac with a capacity greater than 2000 ml, are fortunately rare. However, when such cases appear, surgeons in these locations are faced with the problems of how to safely treat a patient with their limited resources.
CASE REPORT
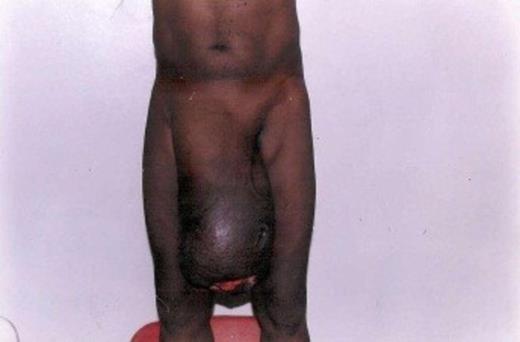
A 55 year old male with a right GIH was referred to a tertiary care hospital in Sierra Leone from a smaller district hospital. The patient was known to have had the hernia since childhood but it had grown large over the years with excoriation of the skin at the apex of the hernia resulting in a painful, foul smelling ulcer measuring 4 x 6 cm. The hernia reached to the patient’s knee while in the upright position and his penis was invaginated into the enlarged scrotal area (figure 1). A smaller left inguinal hernia was also noted.
Economic constraints and fear of surgery led to his delay in seeking treatment. Ultimately family, community and outside financial support allowed him to seek treatment.
Pre-operative counseling was given regarding the planned three stage repair that would be accomplished over a number of months. Stage I, a 2 hour operation under spinal anesthesia, resulted in the excision of the ulcerated skin and partial replacement of the hernia contents into the abdomen as much as possible without compromising the patients’ venous return and breathing (figure 2). Two months later, after the wound had healed, Stage II, a second 2 hours operation under spinal anesthesia, reduced the hernia by an additional 10 cm, again careful not to cause any respiratory compromise or abdominal compartment syndrome and the excessive scrotal skin was removed to maintain the hitched up level of the hernia (figure 3). The patient was advised to rest as much as possible and not to undertake any weight-bearing activities, to allow the abdominal muscles to relax and accommodate well the additional abdominal contents.

Giant inguinal hernia after Stage I: Resection of ulcer and surrounding scrotal skin, partial reduction of hernia sac contents.

Giant inguinal hernia after Stage II: Partial reduction of hernia sac contents and resection of scrotal skin
Five months later, Stage III lasted 7.5 hours and commenced under spinal anesthesia and ended with general anesthesia to fully relax the abdominal musculature. On exploration, the sac contained much of the small intestine and ascending and transverse colon. Bowel loops were adhered together and could not be easily separated from the sac and scrotal skin. The right testis could not be identified.
This final procedure included a lysis of adhesions to separate the small bowel from the ascending colon followed by an en bloc resection of the colon and attached scrotal skin. The specimen included 15 cm of distal ileum and ascending and transverse colon to the splenic flexure. A primary end-to-end anastomosis of the ileum to the descending colon was carried out and a Bassini repair was performed. A scrotal skin reduction allowed ex-vagination of the penis (figure 4). Post-operative recovery was uneventful.

Giant inguinal hernia after Stage III: Bowel resection, ileo-colic anastomosis, hernia repair and resection of scrotal skin)
After discharge from the hospital the patient was followed up four years later in 2009. The operational site looked good, the hernia repair was intact and the patient did not have any complaint. The left inguingal hernia was repaired at that time without complication. The patient returned to his village and was able to ultimately gain employment as a hospital porter.
DISCUSSION
Repair of a GIH needs careful planning as the hernia sac can contain urinary structures, omentum and large and small bowel (4). If the contents of the sac remain unreduced for an extended period of time attempts at sudden reduction can lead to raised intra-abdominal pressure (5). An abdominal compartment syndrome with its consequences of respiratory and circulatory collapse and multi-organ failure can be the results of such an attempt. Furthermore the diaphragm will be displaced into the thoracic cavity, resulting in respiratory difficulty and compromised venous return. The replacement of the intestine in the abdomen may also lead to intestinal obstruction.
Management options can be grouped into either enlarging the abdominal cavity or debulking the abdominal contents. The abdominal cavity can be enlarged by insufflation with CO2 over time causing a pneumoperitoneum (1,2), a phrenectomy, or by use of a large prostetic mesh to repair the defect (5,6). Splenectomy, omentectomy, small or large bowel resections can be optional if debulking of the abdominal contents are necessary. These procedures are often combined and contribute to long operative times and usually necessitate an ICU admission and post-operative ventilation (7).
Insufflation and prostetic mesh were unavailable in our setting. Furthermore neither phrenectomy nor splenectomy is advisable for a patient who must earn a living performing difficult manual labor or where infectious diseases, such as malaria, are common. Long intensive care unit stays and ventilators are also rarely available in a low-resource setting context.
Therefore this case in Sierra Leone was best managed in a multi-stage operation where the abdomen was gradually accustomed to more organs being returned and finally a debulking procedure for organs that could not be safely reduced. For this case a 3-stage procedure was needed, however, earlier experiences (n=21) by the senior author (SSD) show that 2 stage procedures can be undertaken for less complicated GIH. For surgeons working or visiting such a setting, it is important to be aware of the pitfalls of trying to repair such a hernia in a single stage, but also to understand that such cases are not infrequent and that safe techniques are available. Time must also be taken to explain to the patient and family that this is a multi-stage procedure that will be undertaken over a protracted period of time.



