-
PDF
- Split View
-
Views
-
Cite
Cite
E Iacovou, A Chrysovergis, P Kontopoulos, J Xenelis, Cochlear implantation following temporal bone fracture, Journal of Surgical Case Reports, Volume 2011, Issue 12, December 2011, Page 4, https://doi.org/10.1093/jscr/2011.12.4
Close - Share Icon Share
Abstract
Patients with bilateral temporal bone fractures frequently suffer profound hearing loss. These patients may benefit from cochlear implantation. Displaced fracture lines and ossification of the cochlea might complicate insertion of the electrode array. In the present paper we present a case of a failed cochlear implantation due to ossification of the cochlea, followed by a successful one on the opposite side in a patient who sustained bilateral temporal bone fractures. Preoperative imaging may identify these factors, help guide the appropriate surgical approach and choose which side to implant. We aim to highlight the necessity of imaging and discuss the reliability of computed tomography (CT) scanning in predicting cochlear patency in cases of temporal bone fracture. Possible management options in the case of complex cochlear implantation are also described.
Introduction
Patients with bilateral temporal bone fractures that run through the otic capsule may lose their hearing. These patients often become good candidates for cochlear implantation. The present paper describes a case of cochlear implantation after a bilateral temporal bone fracture causing bilateral profound hearing loss and ossification of one cochlea. A CT scan prior surgery showed patency of both cochleas. However, attempted surgery on the left ear failed due to ossification of the cochlea. A subsequent postoperative CT scan showed patency of the right cochlea and the patient was successfully implanted on that side at a second stage.
Case report
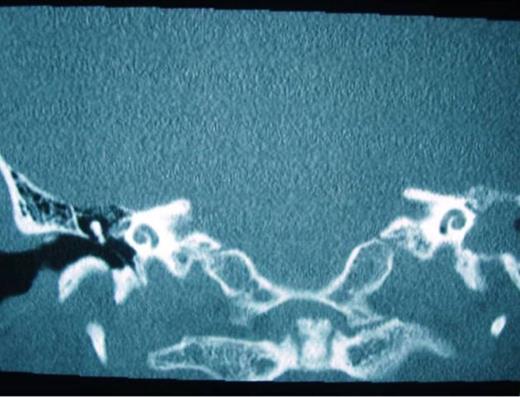
A 52 –year-old male with bilateral deafness and right facial nerve palsy presented to our clinic. The patient who was referred for consideration of cochlear implantation had a history of head injury 8 months before. An initial CT scan 2 months following his injury showed a transverse temporal bone fracture on the right side and a longitudinal one on the left side. Both cochleas appeared to be patent (Fig. 1, 2). The left ear was chosen for implantation as the injury was less severe on that side.
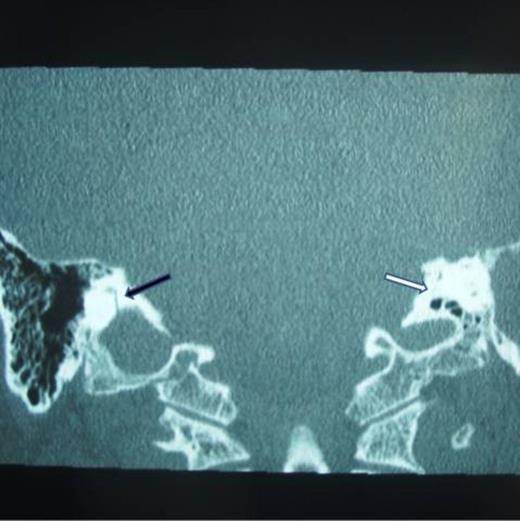
Right transverse fracture (black arrow) and left longitudinal fracture (white arrow)
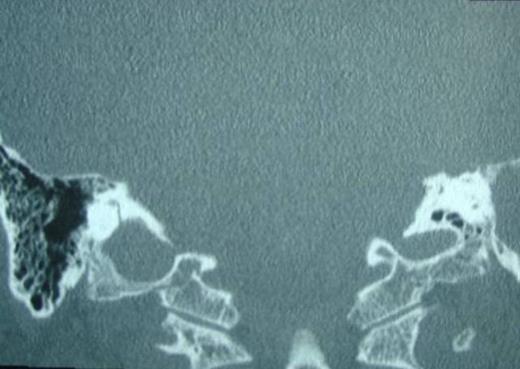
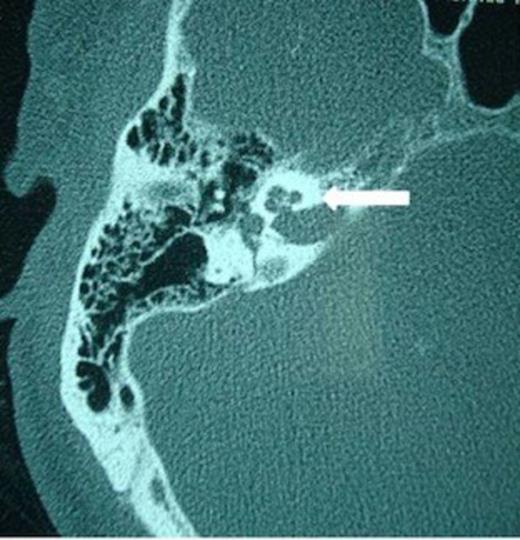
When surgery was attempted, cochleostomy revealed complete obliteration of the scala tympani. Efforts to insert the electrode through the scala vestibuli were also unsuccessful. The procedure was abandoned and a subsequent high resolution CT scan showed complete ossification of the left cochlea and but a patent cochlea on the right (Fig. 3 and 4). Twenty days following the initial attempt, a right cochlear implantation was successfully performed. Following mapping, programming, and aural rehabilitation, the patient was able to understand speech and use the telephone.
Discussion
Temporal bone fractures are divided into two groups: longitudinal and transverse fractures. Longitudinal fractures begin in the squamous part of the temporal bone, extend through the external auditory canal, across the middle ear, and terminate near the carotid canal. Hearing loss in this type of fractures is usually conductive due to ossicular dislocation. Transverse temporal bone fractures extend across the petrous ridge, with the fracture beginning in the posterior fossa and crossing the otic capsule into the middle ear space. Patients might present with hemotympanum and an intact tympanic membrane. Furthermore the fracture might allow communication between the subarachnoid space and the middle ear, increasing the risk of meningitis or involve the internal auditory meatus, causing possible damage to the cochlear nerve.
Patients with bilateral profound hearing loss secondary to fractures become candidates for cochlear implantation. There are few reports in the English literature of successful cochlear implantation in patients with deafness from temporal bone fractures (1-3).
Histopathological studies of temporal bone fractures reveal a variety of injuries such as complete destruction of the organ of Corti and stria vascularis, loss of hair and ganglion cells, hemorrhage into the cochlear duct, and labyrinthitis ossificans (3,4). As reported by Nadol et al (5) a number of ganglion cells may survive in temporal bone fractures. Nadol reports an average survival of only a third of the ganglion cell population after temporal bone fractures. However, there is no strong evidence in literature showing a correlation between ganglion cell counts and auditory function after cochlear implantation. It seems that even poor ganglion cell survival might allow successful electrical stimulation. (6)
Although fractures of the otic capsule usually heal by fibrosis, sometimes they may be complicated by cochlear osteoneogenesis and result in ossification of the cochlea. The most frequent site of ossification is the basal turn of the scala tympani (2,3). In such cases alternative techniques for implant placement have been described. Successful electrode insertion has been achieved by drilling out the obliterated portion of the basal turn (2) or by performing a partial labyrinthectomy to gain access to the round window and allow electrode insertion (7). Furthermore, a scala vestibuli insertion may be attempted (8). Postoperative results in these patients were comparable to those with a conventional scala tympani insertion. In addition, the sooner the implantation was performed, the greater the possibilities for a successful insertion, as there is less time for ossification (1).
The exact time of ossification of the cochlea following a temporal bone fracture is not known. As illustrated in our case, it is best to obtain temporal bone imaging immediately prior to implantation to rule out labyrithitis ossificans or other abnormalities, especially when there has been a long time delay between injury and surgery. In our case the initial CT scan failed to demonstrate ossification of the cochlea, showing patency of both cochleas. According to Siedman et al (9) CT scan may miss up to 22% of cases of cochlear luminal obstruction, subsequently found at surgery. In addition, as reported in literature MRI scan (T2-weighted images) is becoming an increasingly significant imaging modality in investigating cochlear patency. Its role in differentiating between cochlear fluid, fibrosis or bone formation is under evaluation in a number of centers. With T2-weighted image it is possible to assess the cochlea, the semicircular canals, the internal acoustic meatus and the cerebello-pontine angle. As shown by Laszig et al the detection of the absence of fluid seems to be a more sensitive method for determining patency of the cochlea (10).
Temporal bone fractures may lead to ossification of the cochlea and implantation must therefore be performed as soon as possible following injury. Both HRCT and MRI scans are required to assess patency of the cochlea, involvement of the internal auditory meatus or possible communication between the subarachnoid space and the middle ear. In cases of bilateral fractures, implantation is best avoided on the site of transverse fracture, due to the possibility of direct intracranial communication and risk of meningitis.



