-
PDF
- Split View
-
Views
-
Cite
Cite
D Yerrakalva, R Ackroyd, F Lee, Metastatic malignant melanoma causing ileo-ileal intussusception, Journal of Surgical Case Reports, Volume 2011, Issue 12, December 2011, Page 1, https://doi.org/10.1093/jscr/2011.12.1
Close - Share Icon Share
Abstract
We report here a rare case of metastatic malignant melanoma presenting as ileo-ileal intussusception. A 66-year-old man revealed a past medical history of excision of malignant melanoma, followed by axillary lymph node spread treated with block dissection and radiotherapy. He presented with symptoms of small bowel obstruction and subsequent CT revealed a likely nodular intussusception. Resection confirmed the intussusception and histological analysis confirmed the lead point as metastatic malignant melanoma.
It has been reported that up to 5% of those with malignant melanoma will present with bowel metastases before death, yet autopsy studies estimate approximately 60% of those with melanomas have GI metastases. Intussusceptions themselves account for only 1-5% of intestinal obstructions in adults. The magnitude of silent metastases highlights the need to take those with a previous malignant melanoma presenting with GI symptoms seriously as surgery can affect survival.
INTRODUCTION
Though reports of small bowel metastatic malignant melanoma are uncommon, their presentations as intussusception are rare. These metastases can present with almost any gastrointestinal symptom, which makes diagnosis difficult. Further, autopsy reports show much higher incidence of metastases to bowel than reported in life (1).
We discuss here one such case and highlight the need for awareness of this presentation as surgical intervention can alter survival (1,2,3).
CASE REPORT
A 66 year old man with a previously resected cutaneous malignant melanoma was admitted in December 2010 with a one month history of intermittent generalised abdominal pain, vomiting and constipation.
He gave a history of surgical excision of a melanoma in 2005. The melanoma had a Breslow thickness of 1.8mm and he had Clark level III disease. In 2008, he complained of pain in his right axilla. USS-guided biopsy revealed metastases to the right axillary lymph nodes which were treated with block dissection and chemotherapy. Further, a CT scan in August 2010 had shown a non-obstructing nodular intussusception, with the most proximal lesion being at the duodeno-jejunal flexure, but the patient was asymptomatic at this point so was only monitored.

Plain radiograph showing dilated small loops of bowel with a transition point in the right upper quadrant

A repeat CT scan in November 2010 showed evidence of small bowel obstruction and increased nodularity of the previous abnormality. The patient complained of intermittent, generalised abdominal pain over the previous month, with several days of vomiting and incomplete constipation. Examination revealed a soft, distended abdomen with generalised tenderness and tinkling bowel sounds. He was admitted and initially treated with conservative management. His symptoms settled and he was discharged.

Two weeks later, he was readmitted with worsening pain and absolute constipation. Abdominal X-ray showed marked dilatation of the proximal and mid small bowel loops in keeping with high grade small bowel obstruction. CT confirmed this, demonstrating the classic donut sign on coronal reformat; the wall of the intussusception appeared thickened but no definite mass lesion was seen at this point.
Laparotomy confirmed the diagnosis of ileo-ileal intussusception, but it could not be reduced. The apex looked like tumour with seven further tumour deposits seen throughout the small bowel, the largest being proximal to the intussusception with serosal involvement. The intussusception was resected (25cm of small bowel) with creation of an end-to-end anastomosis. A wedge resection of another deposit was also performed.
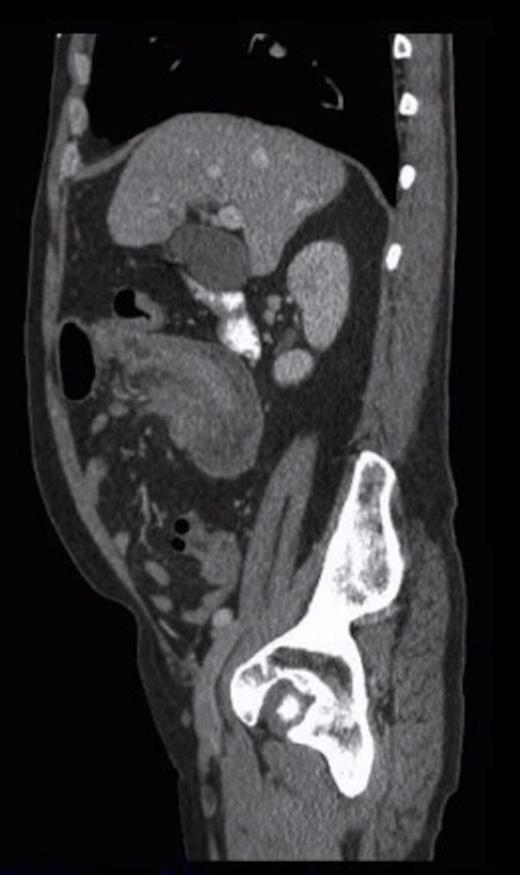
Sagittal CT showing the ‘sausage’ appearance of the intussusception
Histological analysis confirmed the presence of metastatic malignant melanoma. Biopsies contained two distinct tumours with surface ulceration spreading into the muscularis propria but with clear margins. Immunohistochemistry showed the cells to be HMB45 positive. Slides from right axillary block dissection of the metastatic melanoma were reviewed and showed similar morphology.
DISCUSSION
The gastrointestinal (GI) tract is one of the commonest sites for metastases of malignant melanomas. The small bowel is thought to account for 50% of these gastrointestinal metastases (4). 1-3% of all GI malignancies are due to melanomas, and it is the commonest extra-abdominal primary to metastasise to the GI tract1.
Lens et al. (1) report that up to 5% of those with malignant melanoma will present with bowel metastases before death, yet autopsy studies estimate approximately 60% of those with melanomas have GI metastases. The magnitude of silent metastases coupled with the fact that these metastases can present with almost any GI symptom highlights the need for high clinical suspicion in patients with a previous malignant melanoma presenting with GI symptoms.
Small bowel metastatic malignant melanoma is uncommon but its presentation as intussusception is extremely rare. Intussusceptions themselves account for only 1-5% of intestinal obstructions in adults (5). Furthermore, only 30% of small bowel intussusceptions are due to malignant disease.
Surgery is currently the treatment of choice (1,2,3). There is good evidence base for its safety, its symptomatic benefit, but also its effectiveness in prolonging remission. 5-year survival rates of 20-41% have been reported after complete surgical resection with free surgical margins, and long-term survival of up to 10 years (1,2,3).
While the rarity of this presentation is clear, the literature suggests that many of those with malignant melanomas harbour silent small bowel metastases. This means early investigation of patients with gastrointestinal symptoms and past history of malignant melanoma is important as surgical management can make a significant impact on survival.



