-
PDF
- Split View
-
Views
-
Cite
Cite
VSR Rao, R Watkins, AZ Kaleem, J Cooke, K Wedgwood, Leukaemic infiltration of gall bladder – unusual presentation of occult chronic lymphocytic leukaemia, Journal of Surgical Case Reports, Volume 2011, Issue 1, January 2011, Page 7, https://doi.org/10.1093/jscr/2011.1.7
Close - Share Icon Share
Abstract
Extramedullary involvement in early stage chronic lymphocytic leukaemia (CLL) is rare. We report the first case of an incidental finding of gall bladder infiltration in a patient who underwent a cholecystectomy for gallstone pancreatitis with no preceding history of CLL. This case reiterates the importance of subjecting even routine cholecystectomy specimens for histopathology examination in the context of this unusual presentation.
INTRODUCTION
Chronic lymphocytic leukaemia (CLL), the commonest type of leukaemia, is a generalised malignancy of lymphoid tissue originating in the bone marrow. It is characterised by an accumulation of monoclonal lymphocytes, usually of B cell type. The malignant lymphocytes spread from the bone marrow to blood, lymph nodes and other organs. CLL is regarded as small lymphocytic lymphoma when lymph nodes are involved but the blood film and, in particular, the white blood cell count is normal. CLL is typically indolent with affected individuals living for many years without treatment. We report a case of a 71-year-old man who had CLL discovered incidentally in the gall bladder wall following laparoscopic cholecystectomy with no history of CLL prior to surgery.
CASE PRESENTATION
A 71-year-old man underwent elective laparoscopic cholecystectomy following an episode of gallstone pancreatitis. Postoperative recovery was uneventful. His medical history included ischaemic heart disease and radical radiotherapy for Ca prostate.
The gall bladder was received opened with an empty lumen, the presence of gallstones having been noted at the time of surgery. The mucosa was its usual green, velvety appearance and the serosal surface showed shaggy adhesions. The gall bladder wall was thickened at 0.4 cm but was otherwise unremarkable. The gall bladder was sampled in the standard way, namely with sections from the neck, fundus and head. The sections from the neck and fundus showed acute-on-chronic mucosal inflammation with focal mucosal erosion. Histology of the section from the head of the gall bladder showed an acute-on-chronic inflammatory infiltrate within the mucosa along with a dense lymphoid infiltrate in the gall bladder wall (Figure 1).
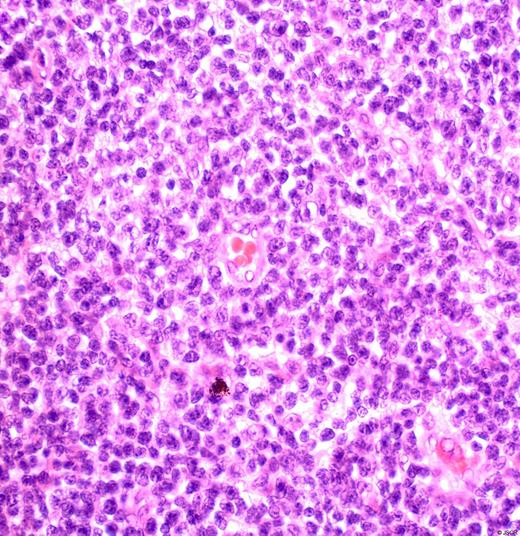
High power photomicrograph of the lymphoid infiltrate within the gall bladder wall. The population is monomorphous and comprised of small lymphocytes with a bland cytological appearance.
Only occasional germinal centres were present. The lymphocytes were small and, other than the monomorphous appearance, were cytologically unremarkable. Initial immunohistochemical staining showed that the infiltrate was predominantly B-cell in nature (CD20 and bcl-2 positive with the T-cell marker CD3 decorating a much smaller population of T-cells dispersed within the infiltrate), confirmed on immunohistochemical staining with the B-cell marker CD20 (Figure 2). Further analysis by the regional Haematological Malignancy Diagnostic Service confirmed the CLL phenotype (CD10 negative, bcl-l negative, bcl-2 positive, CD5 positive, CD20 positive, CD23 positive, CD79 positive, bcl-6 equivocal, CD27 equivocal). The Mib-1 labelling index was 5%.
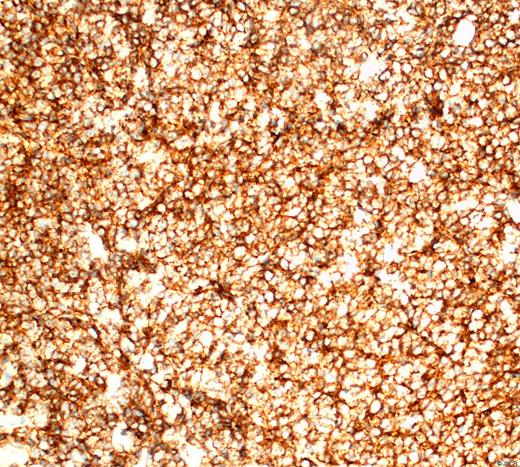
High power photomicrograph of an immunohistochemical stain for the CD20 antigen decorating small B-lymphocytes.
Following the incidental finding of CLL in the gall bladder wall, the patient underwent further clinical evaluation, which ruled out lymphadenopathy and hepatosplenomegaly. A peripheral blood smear revealed a normal myeloid lineage with small to medium size lymphocytes. Computed tomography of the chest, abdomen and pelvis was essentially normal, showing no evidence of hepatosplenomegaly or mediastinal, abdominal and pelvic lymphadenopathy. A bone marrow biopsy was not performed in view of the normal peripheral blood smear and imaging.
At haematological review one year later, the patient developed thrombocytopenia. A bone marrow biopsy confirmed marrow infiltration by B-cell chronic lymphocytic leukaemia. In the absence of B symptoms, it was decided to place the patient on routine follow up.
DISCUSSION
CLL primarily affects adults in later life and is characterised by a proliferation of B-lymphocytes associated with suppression of the immune system, failure of the bone marrow and infiltration of malignant cells into organs. CLL originates in the bone marrow and can spread to the blood and organs of the haemopoietic system. In end-stage disease, CLL can spread to non-haemopoietic structures such as the liver, lungs, gastrointestinal tract, skin, central nervous system, bone, heart, adrenal glands and kidneys (1). Common sites of extramedullary involvement include the lymph nodes and spleen. Unusual cases of early stage CLL with infiltration into prostate, pituitary, myocardium, thyroid, lung, and orbit have been reported (2,3,4,5).
Extramedullary involvement is more frequently seen in patients with acute lymphoblastic leukaemia where common sites of infiltration include the central nervous system, spleen, liver, lymph nodes, ovaries and testes. Skin involvement (leukaemia cutis) and gingival infiltration are seen in approximately 10% of patients with acute myeloid leukaemia (6). Extramedullary involvement of the gastrointestinal tract is relatively rare and the reported autopsy incidence ranges from 5.7% to 13% and is as high as 20% in cases of acute lymphoblastic leukaemia (7). In one of the largest autopsy series, Cornes and colleagues evaluated almost 15,000 consecutive autopsies and identified 264 cases of leukaemia. The most frequently involved sites were the stomach, ileum, and proximal colon, whereas the duodenum and distal colon were less frequently affected (8).
The only case of gall bladder involvement by CLL that has been published to date in the reviewed literature, concerned a 62 year old woman who underwent an emergency cholecystectomy for acute cholecystitis. She had a history of Rai stage IV B-cell chronic lymphocytic leukaemia and was in partial remission, having been treated with prednisolone and chlorambucil. Histology revealed transmural infiltration of the gall bladder with small lymphoid cells, which on immunohistochemistry were positive for CD20 with aberrant expression of CD5 (9). The case we report here recapitulated this immunophenotype.
This is the first reported case of gall bladder involvement by CLL without a previous diagnosis of CLL. All previously reported cases with extramedullary involvement had a history of CLL. This patient was subsequently confirmed to have leukaemic marrow infiltration with CLL and remains stable with no B symptoms. This case reinforces the necessity of subjecting all gall bladder specimens for histopathological examination following routine cholecystectomy contrary to recent suggestions by some studies that this is not necessary if the gall bladder is marcoscopically normal (10).



