-
PDF
- Split View
-
Views
-
Cite
Cite
David Comer, Amit Bedi, Peter Kennedy, Kieran McManus, Werner McIlwaine, Successful Endobronchial stenting for bronchial compression from a massive thoracic aortic aneurysm, Journal of Surgical Case Reports, Volume 2010, Issue 4, June 2010, Page 2, https://doi.org/10.1093/jscr/2010.4.2
Close - Share Icon Share
Abstract
A case of bronchial occlusion caused by a thoracic aortic aneurysm and the relief of this obstruction by the implantation of expandable metallic stents is described. Stent deployment provided an immediate improvement in lung ventilation and chest radiograph appearances. Stent insertion was uncomplicated, but weaning from mechanical ventilation was unsuccessful and the patient died from a ventilator-associated pneumonia, unrelated to the procedure. Endobronchial stenting should be considered as a non-invasive therapy for the treatment of bronchial obstruction, with respiratory compromise, caused by a thoracic aortic aneurysm when vascular surgery is not an option. The medium to long term survival of this patient group is poor. This can be attributed to complications related to the stent and also to the poor performance status of these patients.
INTRODUCTION
We report a case of 77 year old woman who was found to have a bronchial occlusion caused by a thoracic aortic aneurysm and the relief of this obstruction by the implantation of expandable metallic stents is described.
CASE REPORT
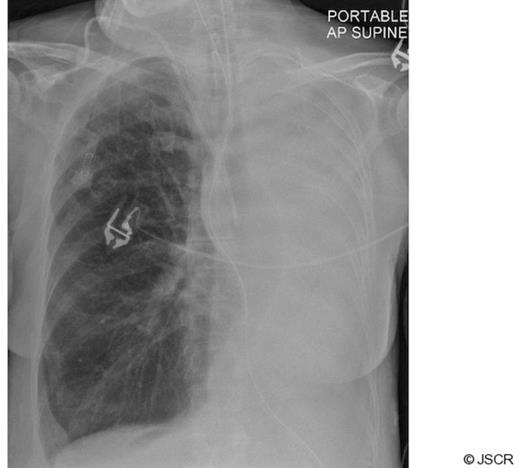
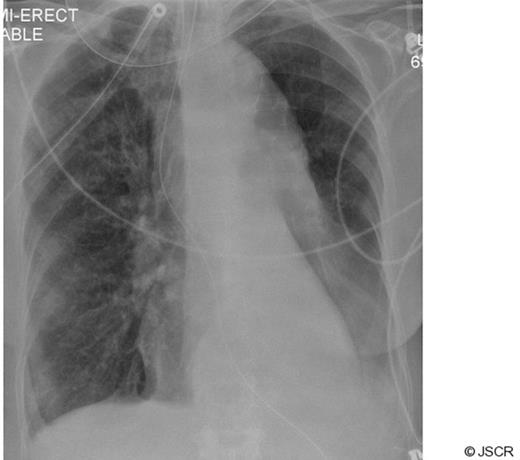
A 77 year old lady presented after an episode of chest pain and dyspnoea. Clinical examination was unremarkable apart from a low grade temperature of 37.8 oC and breath sounds were equal bilaterally. There was no evidence of cardiac ischaemia on an electrocardiogram. Inflammatory markers (white cell count and C-reactive protein) were raised. The cardiac enzyme levels were within normal limits. Empirical antibiotic therapy was instituted for a clinical diagnosis of lower respiratory tract infection. After admission the patient's condition deteriorated with increasing dyspnoea and a worsening PaO2 / FiO2 ratio. Her chest radiograph showed a complete “white-out” of her left lung field (Fig 1). Her trachea was intubated and her lungs mechanically ventilated.
CT scanning revealed a large descending thoracic aortic aneurysm measuring 8 cm in maximum diameter (Fig 2). The left main bronchus was compressed between the aneurysm and the aortic trunk (Fig 3). The patient was regarded as unfit for an open replacement of the aneurysm. The neck of the aneurysm was markedly conical immediately distal to the left subclavian artery, so proximal stent graft placement would have necessitated left common carotid artery and left subclavian artery bypass grafting to provide a parallel proximal landing zone. The distal neck was also markedly conical with a diameter of 42 mm at the coeliac axis, with extensive mural thrombus. These features rendered a successful endovascular repair unlikely, and therefore endovascular interventional was discounted.


CT chest showing complete compression of left main bronchus by large aortic aneurysm
Flexible bronchoscopy with fluoroscopic guidance under general anaethesia was used to deploy two uncovered expandable metallic stents (Ultraflex; Boston Scientific, Ballybrit Business Park, Galway, Ireland). One stent was placed into her left main bronchus (proximal release, length, 4 cm; diameter, 10 mm) and the second into her right main bronchus (proximal release, length, 4 cm; diameter, 12 mm). Prior computed tomography in this case proved useful in order to provide detailed anatomical information of the occluded airway and thus allowing an effective, uncomplicated, stent insertion. A chest drain was inserted after the procedure for a right sided pneumothorax which had developed while on mechanical ventilation.
Arterial oxygenation improved quickly afterwards, allowing the inspired fraction of oxygen to be reduced to 0.3, and there were no complications from the procedure. A subsequent radiograph confirmed re-inflation of the left lung field (Fig 4).
A multidisciplinary team meeting including vascular surgeons, radiologists and intensivists to discuss this complex case proved pivotal in guiding further treatment options. Definitive treatment of the aneurysm was unanimously deemed to be extremely difficult and so after discussion with the patient's family it was agreed that the risk of the procedure and the burden of care required afterwards would not be in this patient's best interests. Despite what initially appeared to be a successful stent insertion, the patient's condition deteriorated, and she died 23 days later from a ventilator-associated pneumonia. This was unrelated to the stent itself which remained patent.
DISCUSSION
The use of endobronchial stenting as a means to relieve extrinsic bronchial compression caused by a thoracic aortic aneurysm is rare, with only seven cases reported in the medical literature. Six of these patients, akin to our patient, had an expandable metallic stent deployed in either the left main bronchus, the left lower lobe bronchus or bilateral endobronchial stent insertions when surgical treatment was not feasible. (1-6) The remaining patient, after an initially uneventful tracheal and left lower lobe bronchus stent insertion, required a repeat procedure after 2 days due to significant extrinsic compression which had deformed the original stainless-steel balloon-expandable Palmaz stent (Johnston & Johnston Interventional Systems, Warren, NJ). A metallic Wallstent (Schneider, Minneapolis, MN) was used at this second intervention in the same sites, with additional stenting in the right main stem bronchus, bronchus intermedius and right lower lobe bronchus.(6) The Palmaz stent, easily compressed by an external force, has since become unpopular.(7) In this series of cases, two patients had a fatal massive haemoptysis, caused by erosion of the stent transbroncially resulting in an aorto-bronchial fistula. These complications occurred 18 months after the insertion of a Gianturco-Z stent (Cook Europe, Bjaerverskov, Denmark) and 20 days from an Ultraflex stent respectively.(1,2) The remaining patients had no complications related to the stent itself. Of these, one died of bronchopneumonia 8 days after stent insertion, another died after one year from a myocardial infarction and another after 14 days from presumed rupture of the aneurysm.(3,4,6) A further patient was discharged after 9 days with no complications reported, and the remaining patient was alive after 23.5 months.(5,6)
Expandable metallic stents placement offers both a rapid and effective approach to restoring airway patency, improving ventilatory function and serving to address symptoms. Despite the recognised complications such as airway inflammation, stent migration, airway erosion and perforation, stent fracture and collapse, our patient had no feasible alternative intervention to address her respiratory compromise.(8) In view of the fact that vascular stenting was contraindicated, bronchial stenting was in this case a palliative procedure in order to facilitate weaning from mechanical ventilation. Metallic stents can be categorized into two types: balloon expandable and self-expanding stents. Balloon-expandable stents depend on balloon-mediated deployment in order to expand the stent adequately and do not exert continuous radial pressure after placement. On the other hand, self-expanding metallic stents assume the shape of the required configuration once released. Ultraflex stents used in this case are either bare or covered, with either proximal or distal release systems. These are popular because of ease of insertion, their flexibility, and dynamic expansiveness. Disadvantages include difficulty in removing the stent and repositioning. The Gianturco-Z stent is associated with higher rates of serious complications. (9)
Tracheobronchial stenting is an established and safe method for the palliative treatment of mechanical central airways obstruction. It provides immediate symptomatic relief in patients with a contra-indication to open surgery. (7) Although permanent application of a self-expanding stent to relieve extrinsic compression of a left main bronchus by an aortic aneurysm in this context is a high risk procedure, it can have a role in certain patients. The poor outcome for these patients is usually unrelated to the stent per se. The long term outcome is not known for the Ultraflex stents when used in this context.
In addition to highlighting the uncertainties of Ultraflex stenting in certain non-malignant conditions, this case illustrates the benefits of a multidisciplinary approach to complex surgical cases. The diverse experience of the multidisciplinary team meeting facilitated a considered and balanced approach to ongoing treatment. While initial treatment was instituted in a particularly effective manner, a limit was agreed upon using the recommendations of the multidisciplinary team. Most importantly, family members were involved and were comforted in the knowledge that treatment was guided by experienced surgeons, anaesthetists and radiologists.



