-
PDF
- Split View
-
Views
-
Cite
Cite
Syed Ali Raza Rizvi, Veena Maheshwari, Advanced Upper Eyelid Sebaceous Gland Carcinoma with Deep Orbital Extension, Journal of Surgical Case Reports, Volume 2010, Issue 1, March 2010, Page 5, https://doi.org/10.1093/jscr/2010.1.5
Close - Share Icon Share
Abstract
Sebaceous gland carcinomas (SGC) are highly malignant lid tumors which originate from meibomian glands and rarely from the gland of Zeis, sebaceous gland of caruncle, eyebrows and periocular skin. In many cases correct diagnosis of SGC is delayed because of its ability to masquerade as a variety of other ocular conditions.
A forty year old male presented with a left upper eyelid swelling with an ulcerated wound on its nasal aspect. A differential diagnosis of sebaceous gland carcinoma or preseptal cellulitis was made. Contrast enhanced computed tomography showed an ill defined soft tissue density mass in the left orbit encasing the whole of the optic nerve. A total exentration was performed. A diagnosis of meibomian gland carcinoma was confirmed on histopathology.
This is a report of an advanced sebaceous gland carcinoma with deep orbital extension. An early diagnosis and appropriate treatment may decrease the long term morbidity and extend the survival rate of such patients.
INTRODUCTION
Sebaceous gland carcinoma (SGC) is a highly malignant and potentially lethal tumor that arises from meibomian glands of the tarsal plate, from glands of Zeis or from sebaceous glands of the caruncle, eye brow or facial skin (1). SGC arises from sebaceous material secreting glands and are known to be occasionally multicentric. These tumors are reported to behave aggressively with the tendency to metastasize early with higher mortality rates especially if there is a delay in the diagnosis. In many cases correct diagnosis of SGC of the eyelid is delayed because of its ability to masquerade as a variety of other ocular conditions such as chalazion, chronic blepharoconjunctivitis, basal cell carcinoma or other eyelid tumors.
We describe an advanced case of sebaceous gland carcinoma of the upper eyelid with deep orbital extension.
CASE REPORT
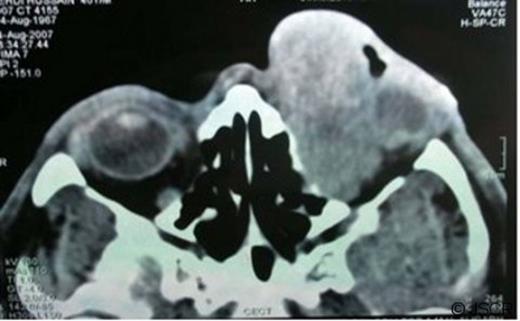
A forty year old male presented to us with loss of vision, pain, swelling and bleeding of the left upper eye lid for the past three months. There was a 1 year history of a small swelling on the left upper eyelid. On ocular examination no light perception was present. A left upper eye lid swelling of 4.0 cm×2.5cm with an ulcerated wound on the nasal aspect of lid margin was seen (Fig 1a). On general examination no lymphadenopathy or organomegaly was detected. A differential diagnosis of sebaceous gland carcinoma, squamous cell carcinoma, or preseptal cellulitis was made. Contrast enhanced computed tomography (CECT) showed an ill defined heterogeneous soft tissue density mass (6.0cm×3.0cm×3.6cm) in the left orbit involving both extraconal and intraconal space. In the intraconal space, the mass was extending deep in the orbit encasing the whole of the optic nerve. There was also a displacement and deformation of the globe laterally (Fig 1b).

left upper eyelid swelling with an ulcerated wound on its nasal aspect.
An incisional biopsy confirmed the diagnosis of Meibomian gland carcinoma. A total exentration of the left eye was carried out. Histopathology showed anaplastic tumor cells arranged in irregular, lobular formation with central necrosis giving it a comedo pattern. The tumor cells were polyhedral with central atypical nuclei, vacuolated eosinophilic cytoplasm and abnormal mitosis (Fig 2). The lateral margins of excision were found to be free from tumor invasion. Based on history, clinical and histopathological findings a diagnosis of Meibomian gland carcinoma of upper lid was made.
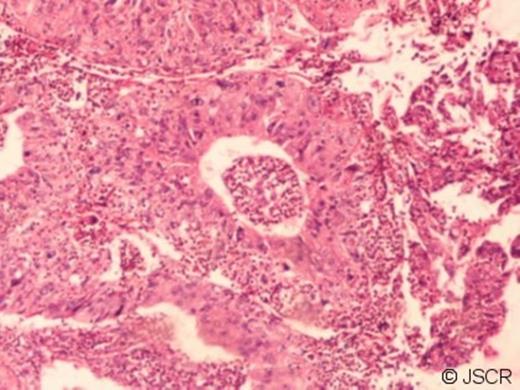
Photomicrograph showing (a) Tumor cells arranged in irregular, lobular formation with central necrosis ( H & E, 125x ) (b)Polyhedral tumor cells with central atypical nuclei, vacuolated eosinophilic cytoplasm and abnormal mitosis ( H & E, 250x ).
The patient remained asymptomatic at one year. Unfortunately he was then found to have developed metastasis to preauricular and submandibular lymph nodes. This was further treated by radical neck dissection and adjuvant radiation therapy of the left orbit. After a further year of follow-ups, no further recurrence or metastasis were found.
DISCUSSION
Meibomian gland carcinoma was described more than a century ago by Fuchs. SGC needs special attention not only because of its masquerading tendency but also because of its much higher prevalence in the Indian subcontinent in contrast to the Western world (2). Prognosis is still regarded as being poor compared with most other malignant eye lid tumors with a mortality second only to malignant melanomas (3).
Numerous factors have been reported to influence the prognosis. Tumors in excess of 10 mm are associated with a poor outcome.4 Tumors of the upper eye lid have been associated with an adverse outcome relative to those affecting the lower lid. The various other clinico-pathologic features that indicate a worse prognosis are vascular, lymphatic and orbital invasion, poor differentiation, multicentric origin, duration of symptoms greater than 6 months, a highly infiltrative pattern and pagetoid invasion of the overlying epithelia of the eye lids (4). The case described has most of the features for a poor prognosis.
A similar case of giant SGC was also reported in an article but without adequate treatment, the patient passed away. The article described the natural course of the disease including metastasis and the importance of adequate early treatment (5).
The majority of recurrences in SGC appear within the first 4 years of treatment. In our case distant metastasis was seen after one year but was treated successfully by radical neck dissection combined with adjuvant radiotherapy.
Patients with SGC must be followed up at short intervals post-operatively as the tumor has a fast growth potential. Adequate follow-up includes meticulous inspection of the local site. Palpation of the pre auricular, submandibular and other neck lymph node chains is mandatory. The approximate guidelines are 3 monthly interval during the first year, 6 monthly during the second year and then on a yearly basis for life (3).
Early diagnosis and treatment may decrease the long term morbidity and extend the survival rate of such patients.



