-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammad Kheir Chahine, Amira Hamou, Dima E Hajj, Layan Ghraizi, Ribal Houmani, Ghassan Nabbout, Raja Wakim, Multinodular cystic pancreatic acinar cell carcinoma presenting as a splenic hilum cyst with peritoneal carcinomatosis: a case report, Journal of Surgical Case Reports, Volume 2026, Issue 1, January 2026, rjag027, https://doi.org/10.1093/jscr/rjag027
Close - Share Icon Share
Abstract
Pancreatic acinar cell carcinoma (PACC) is a rare malignancy accounting for 0.2%–4.3% of pancreatic tumours, typically affecting older men. Cystic variants are exceptionally uncommon and often mimic benign pancreatic lesions, posing diagnostic challenges. We report a 37-year-old woman who was incidentally found to have a large multiseptated lesion involving the pancreas, spleen, and retroperitoneal structures. Surgical exploration demonstrated multiple peritoneal and hepatic nodules. Distal pancreatectomy, splenectomy, omentectomy, and resection of hepatic lesions were performed. Histopathology confirmed poorly differentiated pancreatic acinar cell carcinoma with extensive peritoneal metastases. Postoperative recovery was uneventful. This case highlights a rare cystic presentation of PACC in an atypical demographic. Clinicians should maintain a high index of suspicion for rare pancreatic malignancies in the differential diagnosis of complex cystic abdominal lesions.
Introduction
Pancreatic acinar cell carcinoma (PACC) is an exceedingly rare pancreatic malignancy, accounting for only 0.2%–4.3% of all pancreatic carcinomas and predominantly affecting males in their sixth decade of life [1]. Despite its rarity, PACC incidence has increased by ~73% over the past decade, likely reflecting enhanced diagnostic modalities and the increased use of cross-sectional imaging [2].
The clinical presentation of PACC is often nonspecific. Many cases are detected incidentally on routine imaging, particularly in younger patients who may remain entirely asymptomatic despite harboring advanced disease [1]. Unlike the typical solid architecture that characterizes most pancreatic malignancies, PACC can rarely present as multiseptated cystic lesions, causing significant diagnostic challenges that mimic benign pancreatic neoplasms such as mucinous cystic neoplasms, serous cystadenomas, or pancreatic neuroendocrine tumours [3, 4].
Cystic PACC is extremely uncommon, with <10 cases reported in the literature [5]. Furthermore, PACC overwhelmingly affects older men, making diagnosis in young women particularly unusual [1, 5].
We present a rare case of cystic PACC in a 37-year-old woman with incidentally discovered multiseptated abdominal masses and extensive peritoneal carcinomatosis.
Case report
A 37-year-old woman was referred for further evaluation after incidental discovery of splenic and hepatic masses during an infertility workup. She was asymptomatic, denying abdominal pain, weight loss, fever, fatigue, or gastrointestinal complaints.
Her medical history included only a caesarian section 7 years earlier. She took no medications, had no relevant family history apart from diabetes mellitus, and denied smoking, alcohol, or drug use.
Imaging
Magnetic resonance imaging (MRI) of the abdomen showed a right para-capsular hepatic lesion (28 × 20 mm) with high T2 and low T1 signal and progressive nodular peripheral enhancement. A second multiseptated lesion measuring 10 × 7.8 × 7.2 cm was identified between the spleen, kidney, and pancreas. The mass had thick enhancing walls, irregular septations up to 6 mm, and mass effect on the splenic hilum and pancreatic tail, raising suspicion for malignancy.
Given interval growth and radiologic concern, surgical excision was planned.
Operative findings
A left extended subcostal incision revealed multiple suspicious nodules on the omentum and colonic mesentery. Omentectomy was performed. A large left-sided mass was found abutting the spleen and pancreatic tail (Fig. 1); thus, distal pancreatectomy and splenectomy were performed. Multiple hepatic nodules were also excised (Fig. 2).
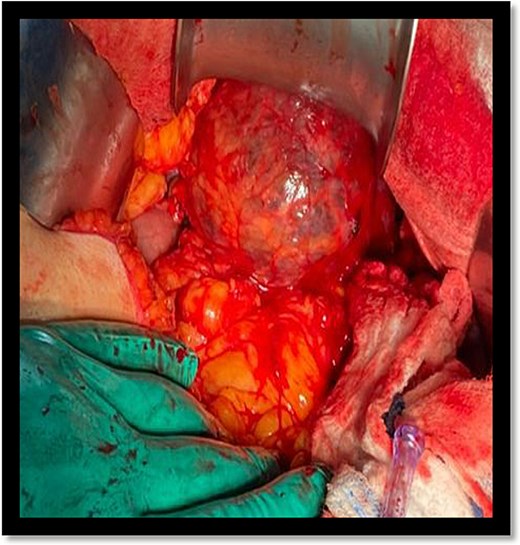
Multiseptated cystic lesion abutting the spleen and distal aspect of the pancreas.
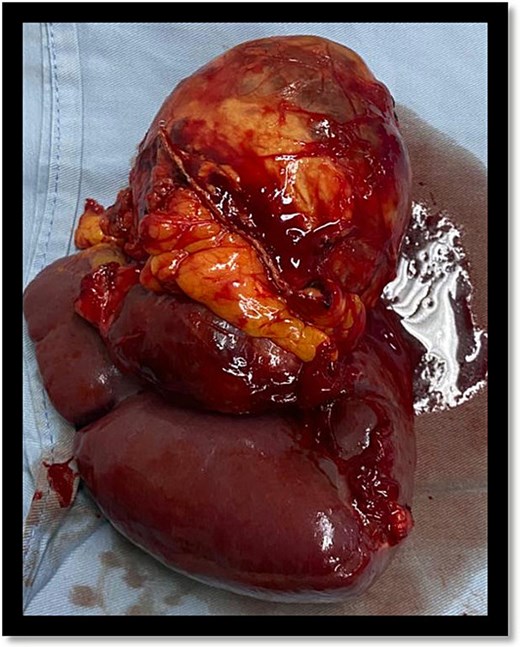
Resected spleen with multinodular cystic mass at the splenic hilum.
Histopathology
Microscopy revealed a poorly differentiated neoplasm with acinar differentiation arising from the pancreas. Metastases involved the omentum, transverse mesocolon, and right diaphragmatic surface. Immunohistochemistry confirmed acinar cell carcinoma.
Postoperative course
The patient recovered without complications and was discharged on postoperative Day 3with appropriate vaccinations and scheduled oncologic follow-up.
Discussion
PACC is a rare pancreatic malignancy, representing a small fraction of exocrine tumours and typically affecting older males [6]. Tumours are often large at diagnosis, with liver metastases occurring in approximately one-third of patients and elevated serum lipase in up to half [7]. Five-year survival ranges between 19% and 22% [7].
Unlike pancreatic ductal adenocarcinoma, PACC frequently presents with vague or absent symptoms, leading to incidental detection. The cystic appearance noted in our case is particularly rare; most PACCs are solid masses in the pancreatic head [1, 3]. Metastatic disease is common at presentation (up to 71%), with the liver, peritoneum, and lymph nodes being frequent sites [8].
The absence of symptoms in our patient, despite extensive metastatic spread, reflects the heterogeneity of PACC. Previous reports describe variability ranging from jaundice and markedly elevated tumour markers to completely normal laboratory studies [9, 10].
Molecular profiling differentiates PACC from ductal adenocarcinoma. While KRAS, TP53, and CDKN2A mutations are uncommon in PACC, BRCA1/2 and ATM alterations are more frequent, suggesting potential benefit from platinum agents and PARP inhibitors [9].
Surgical resection remains the cornerstone of management offering the best chance for a prolonged survival [11]. Chemotherapy, particularly multi-agent regimens such as FOLFIRINOX, has shown benefit in metastatic or node-positive disease [11, 12].
PACC generally carries a better prognosis than ductal adenocarcinoma; resected cases show 5-year survival rates between 36% and 72% [11, 13]. Multimodal approaches combining surgery and chemoradiation may further improve outcomes [7].
Our case demonstrates the need for early surgical intervention when imaging suggests malignancy, even in the absence of definitive preoperative tissue diagnosis. Limitations include lack of preoperative biopsy and unavailability of long-term follow-up data.
This case highlights several important clinical lessons, including that PACC should be considered even in young, asymptomatic women presenting with cystic pancreatic lesions, that early surgical intervention may be warranted in the presence of interval growth and radiologic suspicion for malignancy, and that close collaboration between radiology, surgery, oncology, and pathology teams is essential to optimize outcomes in such rare entities.
Conclusion
Pancreatic acinar cell carcinoma is a rare malignancy that may present with atypical demographics and cystic imaging features, leading to diagnostic uncertainty [14]. This case highlights the need to consider PACC even in young, asymptomatic patients with suspicious or enlarging cystic pancreatic lesions. Early surgical intervention [15] and a multidisciplinary approach are essential to achieve timely diagnosis and optimize outcomes in this uncommon entity [16].
Author contributions
R.H. wrote the Introduction. L.G. wrote the case presentation. D.E.H. and A.H. wrote the discussion. M.K.C. wrote the abstract and the conclusion. G.N. revised and edited the manuscript. All authors approved the final manuscript.
Conflicts of interest
The authors declare no conflicts of interest.
Funding
No funding was received for this study.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and informed consent
This study was approved by the ethics committee of mount-Lebanon hospital. Written informed consent was obtained from the patient.
References
Ikezawa K, Urabe M, Kai Y et al. Comprehensive review of pancreatic acinar cell carcinoma: epidemiology, diagnosis, molecular features and treatment. Jpn J Clin Oncol 2024;54:271–81.
Zhou W, Han X, Fang Y et al. Clinical analysis of acinar cell carcinoma of the pancreas: a single-center experience of 45 consecutive cases. Cancer Control 2020;



