-
PDF
- Split View
-
Views
-
Cite
Cite
Alaa A Alanbagi, Ali N Aldarawsha, Asdah Alawad, Sora A Hasan, Murtadah R Kareem, Aula Ahmed, Muntadher Y H Al Gehadi, Zaryab Bacha, Sajjad G Al-Badri, A rare presentation of recurrent undifferentiated embryonal sarcoma of the liver with peritoneal and splenic metastases: case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf680, https://doi.org/10.1093/jscr/rjaf680
Close - Share Icon Share
Abstract
Undifferentiated embryonal sarcoma of the liver (UESL) is a rare, aggressive pediatric malignancy with a high recurrence rate. We present a case of a 16-year-old male with recurrent UESL and rare peritoneal and splenic metastases. Despite initial complete surgical resection, the tumor recurred, necessitating further surgeries and chemotherapy. PET-CT imaging played a crucial role in monitoring disease progression. This case highlights the importance of a multimodal approach, integrating surgery and systemic therapy, in managing recurrent UESL and underscores the need for long-term surveillance to improve patient outcomes.
Introduction
Undifferentiated embryonal sarcoma of the liver (UESL) is a rare, highly aggressive malignant tumor of mesenchymal origin that accounts for ⁓9%–13% of all pediatric liver malignancies [1]. First described by Stocker and Ishak in 1978 [1], UESL typically presents in children between 6 and 10 years of age, with no significant gender predilection. Clinical symptoms are often nonspecific—most commonly abdominal pain and a palpable mass—making early diagnosis difficult. Imaging frequently reveals a large, cystic hepatic mass with solid and necrotic components, often mimicking benign liver lesions. Management has advanced to include multimodal strategies, with complete surgical resection and chemotherapy—commonly involving ifosfamide and doxorubicin—being central to improved outcomes [2, 3]. In selected cases, liver transplantation may be considered. Although historically associated with poor prognosis, recent treatment advances have raised survival rates to over 80%. This report describes a rare case of recurrent UESL with peritoneal and splenic metastases, highlighting unique management challenges.
Case presentation
A 16-year-old male with no significant past medical history presented with abdominal pain and generalized weakness. Initial imaging with ultrasound revealed a large, encapsulated, thick-walled complex mass measuring 180 × 150 mm, located anteriorly and overlapping the left hepatic lobe without signs of infiltration. The lesion demonstrated solid hyperechoic components with scattered vascularity, internal trabeculations, cystic changes filled with semi-turbid fluid, and scattered calcifications. The liver was normal in size and texture, with no abnormalities in the gallbladder, biliary tree, or spleen. A subsequent computed tomography (CT) scan described the lesion as a cystic mass in the left hepatic lobe, measuring 18 × 14 cm, abutting the pancreas and causing pressure on the stomach. The lesion had internal septa-like soft tissue components with continuous contrast filling, suggestive of a giant hemangioma with cystic changes or less likely a cystic neoplasm.
The patient underwent left lateral hepatectomy and cholecystectomy following diagnosis. Histopathology confirmed undifferentiated embryonal sarcoma (UES) of the liver with a 1 mm clear margin (Fig. 1); immunohistochemistry supported the diagnosis. The gallbladder showed chronic cholecystitis, and the lymph nodes were tumor-free. Postoperative imaging after two months revealed a recurrent mass near the stomach (Fig. 2), confirmed as recurrent UES by biopsy. Re-excision showed extensive necrosis and peritoneal infiltration. Positron emission tomography – computed tomography (PET-CT) later identified peritoneal and mesenteric metastases (Fig. 3). Follow-up PET-CT also revealed multiple small hypermetabolic hepatic nodules in addition to peritoneal and mesenteric lesions, indicating intrahepatic disease recurrence. Six cycles of chemotherapy resulted in near-complete resolution of metabolic lesions, with minimal residual activity. Follow-up imaging showed near-complete resolution of hepatic nodules, with only one residual, non-suspicious tiny nodule. After additional chemotherapy and targeted therapy cycles, PET-CT revealed new focal hypermetabolic activity near the splenic flexure, anterior to the spleen, raising concern for recurrence (Fig. 4). The patient underwent omentectomy and splenectomy. Histopathology confirmed metastatic UES in a 2.5 cm splenic lesion with hemorrhage and necrosis, and a 0.4 cm omental nodule, both completely excised. A total of 15 chemotherapy cycles were completed. Post-treatment imaging showed a mixed-density lesion in the splenic bed with FDG uptake, possibly post-surgical, and a new hypermetabolic mesenteric nodule (Fig. 5). Magnetic resonance imaging showed a cystic post-surgical collection without enhancing lesions. Subsequent imaging revealed regression of the splenic bed lesion and resolution of the mesenteric nodule; however, a new hypermetabolic mesenteric density emerged (Fig. 6). The lesion was placed under active surveillance, with additional chemotherapy administered and repeat imaging scheduled to assess response. Bilateral axillary lymph nodes showed reactive hypermetabolism. The patient, having undergone hepatectomy, splenectomy, and multimodal therapy, remains under close surveillance with encouraging treatment response.

Gross appearance of the resected hepatic mass showing a large, multilobulated tumor with irregular contours. The cut surface reveals heterogeneous areas of hemorrhage, necrosis, cystic degeneration, and solid tumor tissue, features characteristic of UESL. The overall morphology reflects the high-grade and aggressive nature of the neoplasm.

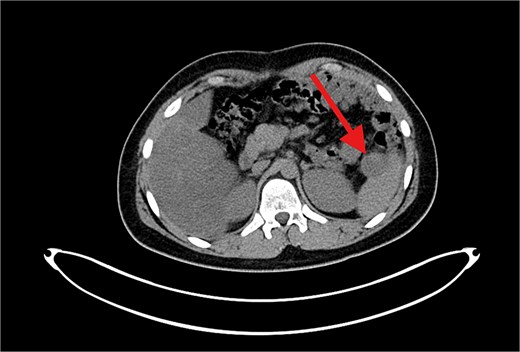
Contrast-enhanced axial CT image showing a large, heterogeneously enhancing soft tissue mass measuring ⁓11 × 5.5 × 8.3 cm in the left subphrenic region, abutting, and indenting the greater curvature of the stomach. The lesion demonstrates internal cystic and necrotic components, consistent with a recurrent undifferentiated embryonal sarcoma.
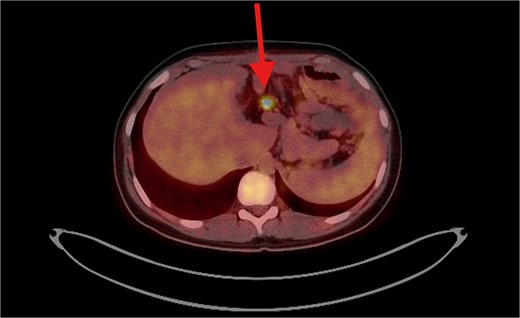
PET/CT scan shows a clear surgical site (left subphrenic area) with no residual/recurrent mass, but there are multiple peritoneal and mesenteric nodules which appear to be hypermetabolic on PET scan, suggesting secondary metastasis.
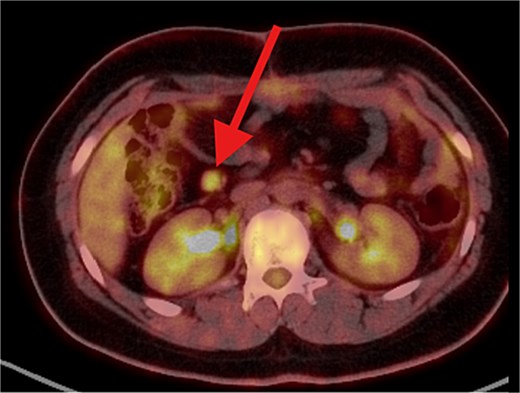
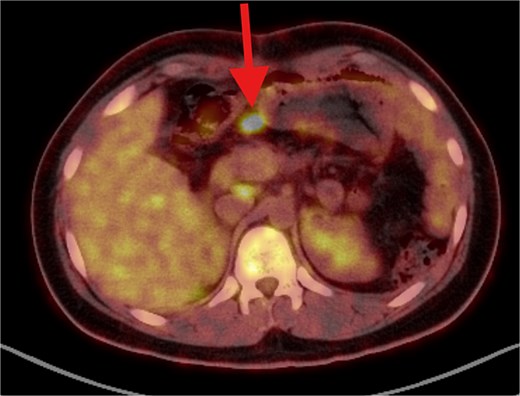
PET/CT scan showing a clear surgical bed. Almost complete metabolic resolution of the previous hypermetabolic abdominal deposits. Development of focal hypermetabolic activity just anterior and abutting the lower spleen pole, at the projection of splenic flexure of the descending colon, this lesion is nonspecific.
PET/CT scan showing a clear surgical bed. There is heterogeneous mostly cystic lesion at splenic surgical bed with moderate FDG uptake at its peripheral soft tissue component, mostly post-surgical sequel. Interval development of right abdominal para median soft tissue / mesenteric nodule with moderate hypermetabolic activity. Suspicious for metastatic process.
PET/CT scan demonstrating the following findings: (1) Clear splenic surgical bed with regression in size and metabolic activity of the previously noted lesion, consistent with resolved post-surgical sequelae. (2) Complete metabolic resolution of the previously identified hypermetabolic right para-median/mesenteric nodule. (3) Development of a new hypermetabolic mid-abdominal mesenteric nodule measuring ⁓2 × 1.5 cm, raising concern for potential disease recurrence.
Discussion
UESL is a rare, aggressive malignant tumor in children and adolescents, accounting for 9%–13% of pediatric liver cancers. Its nonspecific presentation, often mimicking liver abscesses, poses diagnostic challenges [4]. This case is noteworthy for the unusual occurrence of peritoneal and splenic metastases, highlighting the disease’s atypical progression and the complexity of management.
The clinical features of UES often include nonspecific symptoms such as abdominal pain and a palpable mass, as observed in this case. Imaging typically reveals a large, encapsulated cystic hepatic lesion with solid components, findings that align with previous reports describing UES as resembling benign liver lesions like hemangiomas or cystic neoplasms [5]. However, the recurrent and metastatic characteristics of UES in this case are unusual, with limited documentation of peritoneal and splenic involvement. Undifferentiated pleomorphic sarcoma (UPS) of the spleen, a related entity, has been reported to present with symptoms such as abdominal pain and splenic rupture, often leading to diagnostic challenges and mimicking the presentation as in the case of liver involvement. There has also been a case where UESL was misdiagnosed as fallopian tube carcinoma metastasis, underscoring the importance of considering primary liver tumors in differential diagnoses [6].
Research highlights the significance of surgical excision with negative margins as the primary treatment approach. In this case, an initial hepatectomy achieved complete resection, yet recurrence illustrated the aggressive biological behavior of UES. Treatment typically involves a multidisciplinary approach integrating surgical resection and chemotherapy, which has improved patient outcomes significantly. Complete surgical removal remains essential, particularly in pediatric cases where prognosis tends to be more favorable, with reported 3-year overall survival rates reaching 100% in certain studies [7]. In adults, the management of UESL is more challenging due to delayed diagnosis and varied presentations, necessitating a comprehensive approach that includes chemotherapy and, in some cases, radiation therapy to improve survival [8]. The integration of surgical and adjuvant therapies remains fundamental to effectively treating UESL [9].
UESL is recognized as a malignant mesenchymal tumor, indicating its origin from mesenchymal progenitor cells [10]. Histologically, it is characterized by stellate-shaped spindle cells in a myxoid background, features typical of mesenchymal tissue [11]. UESL may arise from hepatic mesenchymal hamartoma, a benign lesion, due to shared chromosomal abnormalities (19q13.4), supporting the hypothesis of a mesenchymal origin [12]. The tumor is known for rapid growth and invasive behavior, often leading to local infiltration and metastasis. In adults, the median time to relapse is ⁓12 months, with a significant proportion experiencing both local and distant recurrences [13]. While metastatic involvement of the peritoneum and spleen is uncommon, it suggests the potential for hematogenous and peritoneal dissemination. The presence of extensive necrosis and hemorrhage in recurrent lesions reflects the tumor’s aggressive nature and response to treatment.
The treatment strategy for UESL underscores the importance of a multimodal approach, combining surgical resection, chemotherapy, and targeted therapy. Complete surgical excision, particularly R0 resection, is essential for improving survival outcomes. While initial resection with negative margins adhered to standard protocols, recurrence necessitated additional procedures like splenectomy and omentectomy. Chemotherapy proved critical in disease control, with positive metabolic responses on follow-up imaging. Despite recurrences, the patient’s favorable response to chemotherapy highlights the evolving role of systemic therapy in advanced UESL, with Doxorubicin and Ifosfamide as standard regimens [14].
This case underscores key aspects of UESL management: its potential to mimic benign lesions, the value of aggressive multimodal therapy, and the role of PET-CT in disease monitoring. Long-term surveillance is crucial due to late recurrences. Although limited by a lack of molecular profiling, this case contributes to the rare literature on splenic and peritoneal metastases and highlights the need for further studies on targeted therapies [15].
Conclusion
This case underscores the aggressive and recurrent nature of UESL, particularly with rare metastatic sites such as the peritoneum and spleen. Despite initial complete resection, disease recurrence necessitated multiple surgeries and systemic therapies. The patient’s favorable response to chemotherapy highlights the importance of a multimodal approach. Long-term surveillance remains essential due to the high risk of recurrence. This report contributes to the limited literature on metastatic UESL and emphasizes the need for continued research into novel therapeutic strategies.
Conflict of interest statement
The authors declare no conflict of interest in preparing this article.
Funding
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics
Ethical permission was applied according to Health Research Ethics guidelines of the Iraqi Ministry of Health.
Consent
Written consent was obtained from the patient.
References
Mocellin S. Hepatic embryonal sarcoma. In: Soft Tissue Tumors. Cham: Springer. 2021.
Thong PM, Luu VD, Lanh NS, et al. . Undifferentiated embryonal sarcoma of liver. J Pediatr Surg Case Rep 2021;64:101746.
Setty BA, Jinesh GG, Arnold M, et al. The genomic landscape of undifferentiated embryonal sarcoma of the liver is typified by C19MC structural rearrangement and overexpression combined with TP53 mutation or loss.
- chemotherapy regimen
- combined modality therapy
- neoplasm metastasis
- sarcoma
- surgical procedures, operative
- liver
- neoplasms
- peritoneum
- liver cancer
- systemic therapy
- childhood cancer
- computed tomography/positron emission tomography imaging
- surveillance, medical
- secondary malignant neoplasm of spleen
- excision
- recurrence risk
- patient-focused outcomes



