-
PDF
- Split View
-
Views
-
Cite
Cite
Deena S Hadedeya, Badr M Beyari, Aljawharah A Alotaibi, Munirah Y Fetani, Salma H Sait, Appendicular neuroma with an initial presentation of renal colic: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf632, https://doi.org/10.1093/jscr/rjaf632
Close - Share Icon Share
Abstract
Appendicular neuroma is rarely diagnosed based solely on histopathological specimens. It mimics acute appendicitis upon presentation and is managed surgically. We present a 46-year-old woman with a final presentation of acute appendicitis. A laparoscopic appendectomy was performed, and the specimen revealed a neuroma of the appendix based on histopathological reports.
Introduction
An acute abdomen is a common complaint in emergency settings. Identifying the underlying pathology is crucial for managing acute abdomen to avoid life-threatening events. Acute appendicitis is a well-known type of appendicitis. However, reports of acute appendicitis due to an incidental neuroma of the appendix are rare [1, 2]. Appendicular neuroma is a benign growth or hyperplasia of neural tissue arising from the vermiform of the appendix [3]. In this case report, we present a patient who initially presented with renal colic pain but was diagnosed with appendicitis based on contrast tomography (CT) scan of the abdomen and was treated surgically. Appendicular neuroma was identified postoperatively based on histopathology.
Case report
A 46-year-old female with a known cerebrovascular accident and renal stone presented at the emergency department with worsening right-sided flank pain, a frank hematuria, and shivering for the past 2 days. There was no history of fever, nausea, vomiting, or diarrhea. The patient had undergone sleeve gastrectomy and laparoscopic cholecystectomy prior to her emergency visit.
On examination, the patient was alert, conscious, and oriented. She was vitally stable, but mildly dehydrated. Tenderness was observed in the right lower quadrant, with a positive Murphy’s sign and round tenderness. There was no guarding, rigidity, Rovsing’s sign, or mass.
Investigations revealed the following: white blood cells, 6.16; hemoglobin, 13.2; platelet count, 259; neutrophils #, 3.22; and C-reactive protein, 1.6. Urine was yellow to clear with a red blood cell count of 66.4.
Unenhanced CT of the abdomen and pelvis using the standard kidney, ureter, and bladder concluded that a 5 × 6 × 3 mm stone was in the right renal pelvis with proximal mild back pressure; the appendix measured 12.5 mm, showing a thick wall and surrounding fat stranding, as seen in Fig. 1.
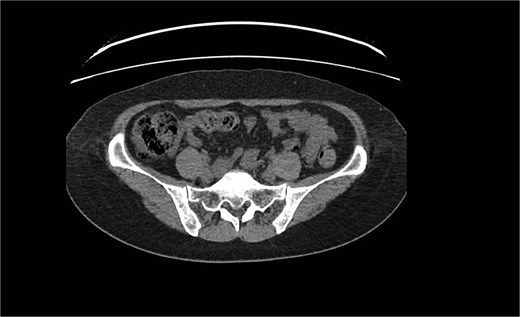
Dilated tubular structure with signs of fat stranding suggesting appendicitis.
Based on her clinical picture and radiological findings, the patient was admitted with appendicitis and underwent laparoscopic appendectomy with a possible open approach. An urologist was consulted regarding the right renal pelvic stone, and they conservative management was recommended. Intraoperative abdominal exploration identified the cecum and revealed an inflamed appendix (not gangrenous or perforated). Appendectomy was performed uneventfully in a classical manner, and the appendix was sent for histopathological examination. The patient spent 1 day in the hospital and was discharged the next day in a stable condition. Upon visiting the clinic, her overall well-being improved, and physical examination revealed a soft and lax abdomen with healed scars at the surgical sites. Histopathology results showed fibrous obliteration of the appendicular lumen/neuroma without any signs of acute appendicitis or malignancy (Fig. 2).
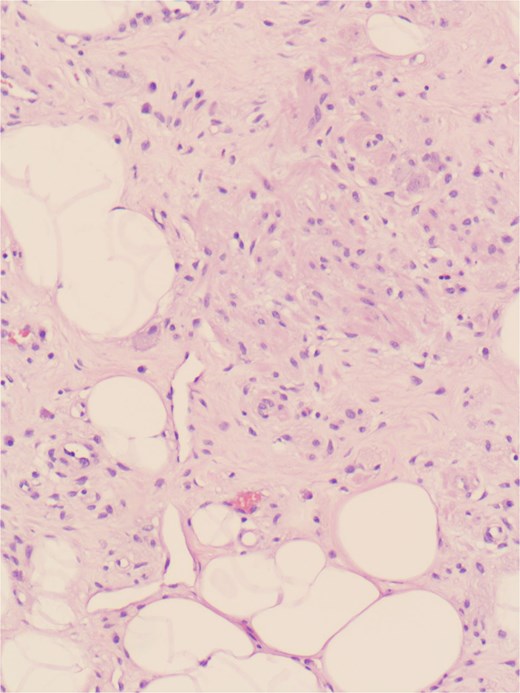
Nerve-like spindle cells and fibrous obliterations suggesting features of an appendicular neuroma.
Discussion
An appendiceal neuroma is a neural tissue proliferation in the appendicular lumen that leads to obliteration of the lumen, as described in the late 1920s by Masson [4].
The pathology of the disease appears as a loose proliferation of positive S-100 protein and neuron-specific enolase spindle cells in a myxoid background, entrapped by connective tissue and fat cells with eosinophil infiltration, as demonstrated by the Stanley [3] report of 20 cases of appendicular neuromas.
The condition is considered a rare and incidental pathology, as demonstrated by a retrospective study by Chan and Fu [5], who found one appendicular neuroma in 11 443 appendicular histological specimens. Moreover, a retrospective study by Elfaedy et al. [6] revealed 10 cases of appendicular neuromas in 4012 species between 2009 and 2017. Therefore, appendicular neuromas is a rare entity indistinguishable from the classic presentation of acute appendicitis. The only method for identifying the nature of the disease is routine histopathology, which is performed postoperatively.
Hussein et al. [7] found that 70% of patients with appendicular neuromas are >26 years old, with a male-to-female ratio of 2:3. As in our case, Al-Janabi et al. reported a female patient, while Molina et al. and Jagtap et al. reported male patients [1, 2, 8]. Although our patient initially presented with renal colic, almost all the aforementioned cases presented with acute appendicitis. All shared the same algorithm for investigation and management. Appendectomy was performed as standard surgical management for all patients. Histopathology was key to identifying appendicular lesions and ruling out other potential malignancies in all cases. No further management was reported in these cases.
In summary, appendicular neuroma is similar to acute appendicitis, with the same management.
Histopathology is crucial as it is a definitive guide for identifying appendicular neuromas.
Conflict of interest statement
None declared.
Funding
None declared.



