-
PDF
- Split View
-
Views
-
Cite
Cite
Zainab Alammar, Jawad S Alnajjar, Mohammed A Almarzooq, Manal Alquaimi, Idiopathic cocoon syndrome presenting as small bowel obstruction with asymptomatic postoperative intra-abdominal collection: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 8, August 2025, rjaf595, https://doi.org/10.1093/jscr/rjaf595
Close - Share Icon Share
Abstract
Abdominal cocoon syndrome (ACS) is a rare cause of small bowel obstruction (SBO). Its nonspecific presentation frequently mimics more common obstructive pathologies, delaying diagnosis. A 56-year-old male presented with abdominal pain, obstipation, and vomiting. CT showed clustered ileal loops. Exploratory laparotomy revealed a thick fibrocollagenous peritoneal membrane encapsulating ischemic bowel loops. Resection of non-viable bowel and enteroenterostomy were performed. Postoperative recovery was complicated with an asymptomatic intra-abdominal collection managed with vacuum-assisted dressing. ACS poses diagnostic and therapeutic challenges. Early recognition and surgical intervention are essential to avoid complications. Clinician awareness is crucial for timely diagnosis and management.
Introduction
Small intestinal obstruction (SBO) is a common surgical emergency [1]. Abdominal cocoon (AC), or sclerosing encapsulating peritonitis, is a rare and often underrecognized cause of SBO [2]. It is classified into idiopathic and secondary types, with the idiopathic variant typically affecting young females [3]. This report a male patient diagnosed with ACS, highlighting the atypical presentation and the diagnostic challenges and post operative course.
Case presentation
A 56-year-old male patient presented to the emergency department with generalized abdominal pain, obstipation, and vomiting for six days. On examination, there was diffuse generalized abdominal tenderness and a palpable mass in the hypogastric region. Contrast enhanced abdominal computed tomography (CT) revealed clustered ileal loops in the pelvis with multiple transitional zones and dilated proximal small bowel loops (Fig. 1).
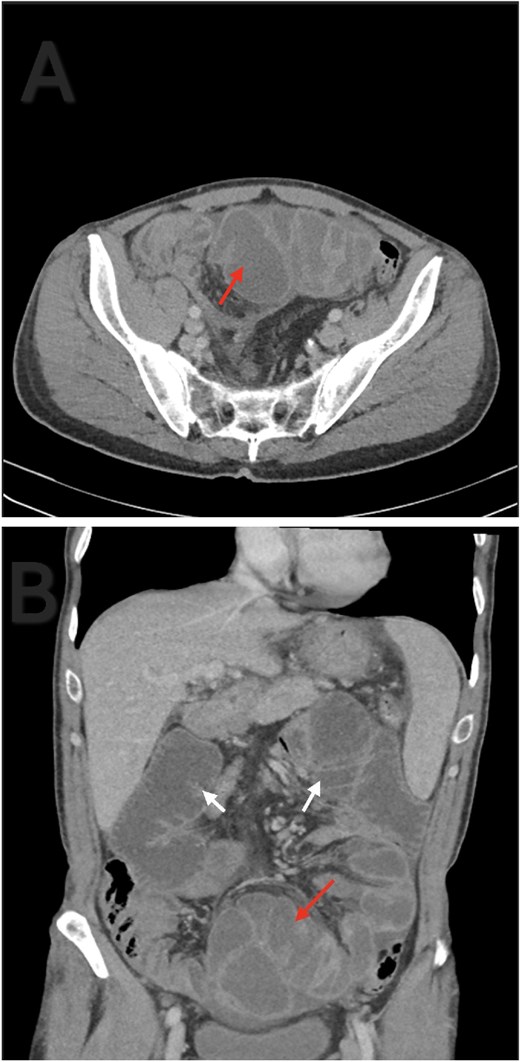
Axial (A) and coronal (B) contrast enhanced abdominal CT. Ileal loops congregated at the pelvis (red arrow). Small bowel loops dilation (white arrow).
Exploratory laparotomy was performed for complete small bowel obstruction. Intraoperatively, a thick, pale peritoneum and whitish turbid fluid were found. The small bowel was encapsulated by dense adhesions. Adhesiolysis was performed, and an ischemic, dilated terminal ileum segment was resected, followed by side-to-side enteroenterostomy (Fig. 2).
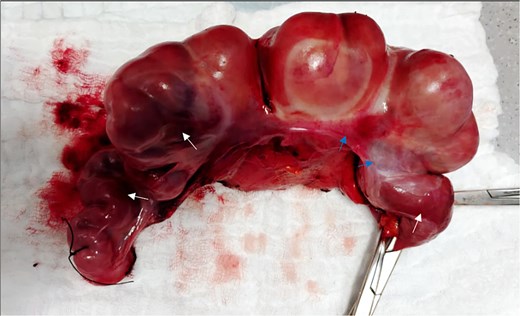
The resected segment of the terminal ilium. Ischemic bowel (white arrows). Thick peritoneum (blue arrows).
The patient initially had an uneventful recovery and was discharged on postoperative day seven. A week later, he returned with asymptomatic pus discharge from the wound. CT revealed a 15 × 8 × 6 cm encapsulated intra-abdominal collection and small fascial dehiscence without signs of anastomotic leak (Fig. 3). After failed radiological drainage, a vacuum-assisted dressing was applied for 8 days. Follow-up ultrasound confirmed resolution of the collection and closure of the defect. The patient was discharged in stable condition and showed complete wound healing at follow-up.
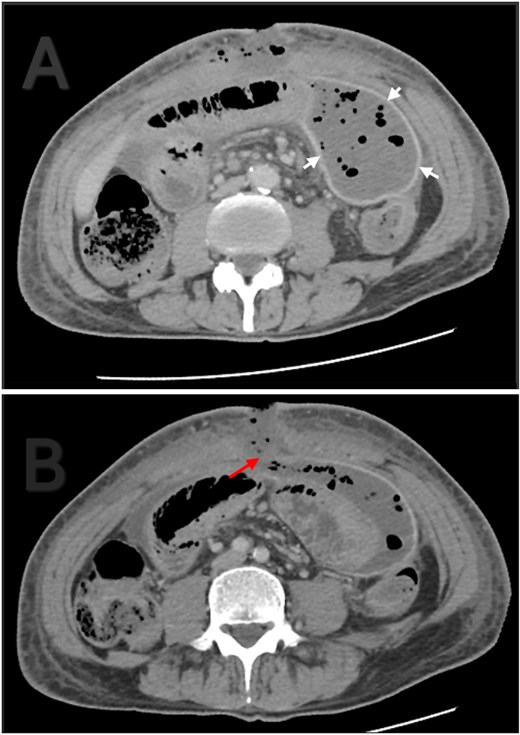
Contrast enhanced abdominal CT. (A) Thick and well localized capsule surrounding the collection (white arrows). (B) The collection is communicating with the atmosphere through a fascial dehiscence (red arrow).
Discussion
Sclerosing encapsulating peritonitis (SEP) first described in 1907 as ‘peritonitis chronica fibrosa incapsulata’ by Owtschinnikow [4] and later termed abdominal cocoon syndrome (ACS) by Foo in 1978 [2]. It is a chronic inflammatory condition where the small intestines are enclosed within a dense fibrocollagenous membrane. ‘Sclerosing’ refers to collagen deposition, ‘encapsulating’ to fibrous sheath formation, and ‘peritonitis’ to the underlying inflammation [3]. The pathogenesis is linked to recurrent subclinical peritonitis, leading to fibrosis and cocoon formation [2, 5, 6]. Our patient had no risk factors, aligning with idiopathic cases reported in previous series [7].
Clinically, ACS presents variably as acute, subacute, or chronic gastrointestinal obstruction, which may be partial or complete. Common symptoms include nausea, vomiting, anorexia, weight loss, and malnutrition, though some patients remain asymptomatic. Rarely, a soft abdominal mass may be palpated [3]. In our case, the patient had a relatively short symptom duration and acute onset, which is atypical compared to reported median durations of several years [8]. ACS is classified into three types: Type 1 involves part of the small intestine, Type 2 involves the entire small intestine, and Type 3 extends to other abdominal organs [9].
CT is the imaging modality of choice, with typical findings including clustered or ‘cauliflower-like’ bowel loops and peritoneal thickening. In our patient, CT revealed clustered ileal loops and transitional zones, raising suspicion for mechanical obstruction. Histopathology, though seldom needed, can support SEP diagnosis by revealing fibroconnective tissue growth, inflammation, and dilated lymphatics. Absence of granulomas, giant cells, or birefringent material helps to rule out tuberculosis [9].
Management of abdominal cocoon syndrome depends on disease severity. Surgery is the mainstay, involving adhesiolysis and membrane excision to restore bowel function. Severe cases may require decompression or bowel resection if ischemia is present, as in our case. Conservative treatment may be adequate for mild symptoms. Incidental appendectomy is often advised [2, 9]. In this case, an ischemic ileal segment was resected followed by side-to-side anastomosis. Studies show preoperative nutritional support reduces complications, while intestinal stenting improves postoperative satisfaction [8].
Conclusion
Abdominal Cocoon Syndrome is a rare challenging and often underdiagnosed cause of small bowel obstruction due to its nonspecific symptoms. Early recognition is essential to prevent complications such as bowel ischemia. Surgery remains the cornerstone of treatment but may be technically difficult due to extensive adhesions. More research and greater clinical awareness are needed to improve diagnosis and outcomes.
Conflict of interest statement
The authors declare no conflicts of interest related to this manuscript.
Funding
None declared.
References
- gastrointestinal tract vascular insufficiency
- abdominal pain
- small bowel obstruction
- bandages
- intestines
- tissue membrane
- surgical procedures, operative
- vomiting
- abdomen
- diagnosis
- ileum
- peritoneum
- obstipation
- dressing of skin or wound
- laparotomy, exploratory
- enteroenterostomy
- emergency surgical procedure
- sclerosing encapsulating peritonitis



