-
PDF
- Split View
-
Views
-
Cite
Cite
Yudai Yokota, Tomofumi Nishino, Tomohiro Yoshizawa, Ryunosuke Watanabe, Hiroshi Noguchi, Hajime Mishima, Successful reduction of an obturator hip dislocation using flexion, abduction, and external rotation: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 6, June 2025, rjaf438, https://doi.org/10.1093/jscr/rjaf438
Close - Share Icon Share
Abstract
Obturator dislocation of the hip is an extremely rare injury. Urgent closed reduction is critical to prevent complications such as avascular necrosis. We report a rare case of a 52-year-old woman who sustained an obturator dislocation following a motor vehicle collision. Manual reduction was successfully performed under fluoroscopic guidance with the hip positioned in flexion, abduction, and external rotation within 3 h post-injury. The patient followed a staged rehabilitation protocol and recovered well with only mild residual discomfort at 6 months. This case highlights the importance of early diagnosis, prompt reduction, and the utility of alternative reduction strategies when standard techniques fail. Long-term monitoring is advised due to the risk of femoral head collapse and subsequent osteoarthritis.
Introduction
Traumatic hip dislocations are typically classified into two main types based on the direction of femoral head displacement relative to the acetabulum: anterior and posterior. Posterior dislocations are significantly more common, whereas anterior dislocations comprise only ~10% of all cases [1]. Anterior dislocations can be further subcategorized into pubic and obturator types, with the obturator subtype being notably rare [2]. Due to the potential for avascular necrosis of the femoral head, prompt closed reduction is regarded as the cornerstone of initial management [1]. Early diagnosis and timely intervention are crucial in preventing long-term complications and optimizing functional outcomes.
Case presentation
A 52-year-old woman was involved in a frontal motor vehicle collision while seated in the rear seat. At the time of impact, she was in a position of hip flexion, mild abduction, and external rotation (Fig. 1), a posture known to predispose to anterior dislocation. She presented to the emergency department with acute, severe left hip pain, and an inability to actively extend the affected limb. Plain radiographs and computed tomography (CT) scans revealed an obturator-type anterior hip dislocation without any accompanying fractures. Notably, a small depression was detected on the anterolateral articular surface of the femoral head (Fig. 2a–d). Based on the imaging and clinical findings, she was diagnosed with a traumatic obturator dislocation of the hip.
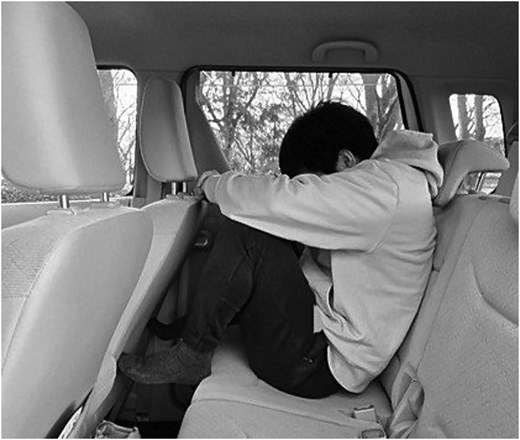
Simulated posture at the time of injury based on patient interview.
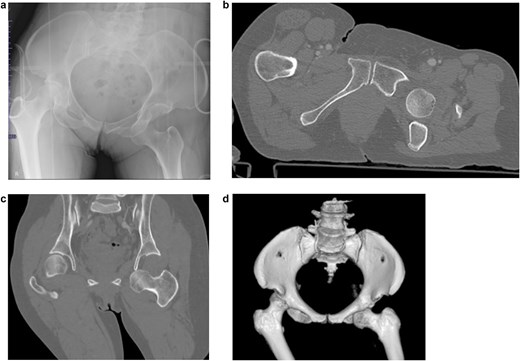
Imaging results at the time of transport. (a) Initial pelvic radiograph showing left femoral head dislocation. (b) Axial CT image showing femoral head displaced into the obturator foramen. (c) Coronal CT image showing inferior and medial displacement of the femoral head. (d) 3D reconstructed CT image showing the femoral head in the obturator foramen.
Manual closed reduction was attempted under intravenous anesthesia using propofol. Initial efforts utilizing flexion, adduction, and internal rotation (Fig. 3a) were unsuccessful. A second attempt using flexion, abduction, and internal rotation (Fig. 3b) also failed to reduce the dislocation. Ultimately, reduction was successfully achieved using a combination of flexion, abduction, and external rotation, along with anteriorly directed pressure applied to the proximal femur (Fig. 3c). The patient tolerated the procedure well, and neurovascular status remained intact post-reduction.

The manual reduction techniques we tried. (a) First reduction attempt: flexion, adduction, and internal rotation (unsuccessful). (b) Second reduction attempt: flexion, abduction, and internal rotation (unsuccessful). (c) Successful reduction with flexion, abduction, and external rotation, with anterior pressure.
Post-reduction CT and magnetic resonance imaging (MRI) demonstrated concentric joint reduction without evidence of femoral head osteonecrosis (Fig. 4a–e). The patient was maintained non-weight-bearing for 4 weeks, followed by partial weight-bearing, and progressed to full weight-bearing by 10 weeks. At the 6-month follow-up, the patient reported only mild residual groin discomfort without any significant restriction in range of motion. Follow-up MRI revealed resolution of initial signal changes in the femoral head, and there were no new findings suggestive of osteonecrosis or cartilage degeneration.
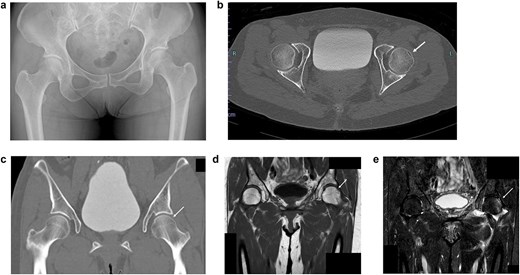
Imaging results immediately after manual reduction. (a) Post-reduction pelvic radiograph confirming reduction. (b) Post-reduction axial CT image confirming reduction. (c) Post-reduction coronal CT image confirming reduction. (d) T1-weighted MRI showing a subchondral band-like low signal area. (e) STIR MRI showing diffuse high signal intensity beneath the subchondral lesion.
Discussion
Anterior hip dislocations, particularly the obturator type, are much less frequent than posterior dislocations, a disparity primarily attributed to the biomechanical strength of the iliofemoral ligament [1–3]. DePalma described two principal mechanisms leading to obturator dislocation. In both mechanisms, forced abduction, external rotation, and flexion of the hip create impingement between the femoral neck and acetabulum, and between the femoral trochanter and ilium [3]. Under such conditions, a posteriorly directed force to the distal thigh or an anterior force at the level of the knee can propel the femoral head inferiorly and anteriorly into the obturator foramen.
Clinically, patients with obturator dislocation typically present with the affected limb in a position of hip flexion, abduction, and external rotation. This case mirrored those findings, supporting the proposed mechanism of injury. The initial posture of the patient during the vehicular accident likely predisposed her to this injury pattern.
The DePalma technique is a well-recognized method for the reduction of anterior hip dislocations and is best performed under general anesthesia with adequate muscle relaxation. The first maneuver involves the assistant applying vertical downward force to the anterior superior iliac spine to stabilize the pelvis while the surgeon performs hip flexion and internal rotation, followed by vertical traction in line with the Allis technique. If reduction is not achieved, a second maneuver is employed, wherein the hip is maintained in abduction and elevated vertically. Subsequently, posterior pressure is applied to the femoral head to achieve upward displacement and internal rotation for reduction [3]. Alternative techniques have also been described, including simple traction with adduction and internal rotation [1, 4, 5], leveraging the same biomechanical principles that cause the dislocation, applied in reverse.
However, DePalma warned of the potential risk of proximal femoral fracture when forceful adduction precedes reduction [3]. In the present case, multiple attempts involving internal rotation failed to reduce the dislocation. Ultimately, successful reduction was achieved using a combination of flexion, abduction, and external rotation, a method conceptually similar to DePalma's second technique. This highlights the importance of adapting reduction strategies based on joint biomechanics and individual anatomy.
The favorable outcome in this case may be attributed in part to the early reduction, which was performed within 3 h of injury. Delayed reduction, particularly beyond 6 h, has been associated with significantly increased rates of avascular necrosis of the femoral head [4, 6].
Post-reduction management for anterior dislocations remains a topic of debate, and there are no standardized guidelines. Some authors advocate for early mobilization, noting no clear association with increased complications [7]. Nonetheless, due to the presence of a subchondral depression and potential for femoral head collapse, we adopted a cautious approach, mirroring protocols typically used for uncomplicated posterior dislocations. According to Clegg et al., patients with posterior dislocation without fracture should follow a staged weight-bearing protocol beginning with toe-touch for 4 weeks [8]. Based on this approach, our patient began partial weight-bearing at 4 weeks. At final follow-up, the patient remained free from radiographic complications, although mild groin discomfort persisted. Given the presence of a femoral head depression, the risk of future osteoarthritis remains, warranting close long-term monitoring.
Conclusion
When standard maneuvers fail, a reduction technique employing flexion, abduction, and external rotation may serve as a reliable alternative for treating obturator-type anterior hip dislocations. Early and accurate diagnosis, along with urgent reduction, are essential components in preventing complications and achieving favorable clinical outcomes. Careful post-reduction management, tailored to individual risk factors, is equally important in optimizing recovery.
Conflict of interest statement
None declared.
Funding
None declared.



