-
PDF
- Split View
-
Views
-
Cite
Cite
Fu-Xiang Lin, Fu Feng, Zhan-Ping Xu, Real-time transrectal ultrasound-guided transurethral resection of prostate cyst: a novel technique and initial clinical experience, Journal of Surgical Case Reports, Volume 2025, Issue 6, June 2025, rjaf407, https://doi.org/10.1093/jscr/rjaf407
Close - Share Icon Share
Abstract
This study introduces real-time transrectal ultrasound (TRUS)-guided transurethral resection of prostate cysts (TURP-Cyst) and reports initial outcomes. Eight patients with symptomatic prostatic cysts underwent the procedure. Mean cyst size was 2.5 ± 0.3 cm, operative time 35.0 ± 16.0 min, and blood loss 14.0 ± 3.6 ml. No major complications occurred. Postoperative catheterization lasted 1.9 ± 0.6 days. At 6 months, TRUS confirmed cyst resolution in all cases. The International Prostate Symptom Score improved from 19.5 ± 1.2 to 7.5 ± 2.5 (P < .001), and quality of life score from 4.4 ± 0.5 to 1.3 ± 0.5 (P < .001). No significant complications like urinary incontinence or erectile dysfunction were observed, and no cyst recurrences were noted. Real-time TRUS-guided TURP-Cyst is safe and effective, offering precise localization, minimal trauma, and significant LUTS improvement. Larger studies with longer follow-ups are needed to validate these results.
Introduction
Prostatic cysts, although relatively uncommon, can lead to significant lower urinary tract symptoms (LUTS) and negatively impact the quality of life [1]. Traditional management strategies, including transurethral resection, transperineal aspiration, and open surgical excision, often encounter challenges such as inadequate visualization of the cyst, potential injury to surrounding structures, and high recurrence rates [2–7]. In recent years, advancements in endoscopic techniques and imaging modalities have paved the way for more minimally invasive alternatives for treating prostatic cysts.
The application of transurethral resection principles and instruments to the treatment of prostate cysts (TURP-Cyst) offers a promising approach. The use of real-time transrectal ultrasound (TRUS) guidance in this context not only enhances the localization of the cyst but also allows for precise dissection while minimizing the risk of injury to adjacent tissues. This study introduces a novel technique involving real-time TRUS-guided TURP-Cyst for the treatment of prostatic cysts and presents initial clinical outcomes focusing on cyst resolution, surgical complications morbidity, and improvements in LUTS.
By highlighting the role of TRUS in enhancing surgical precision and safety, we aim to demonstrate how this new technique overcomes limitations associated with traditional methods. Additionally, this paper explores whether TRUS serves as an invaluable tool for surgeons of varying experience levels, thereby improving surgical success rates and patient satisfaction. Through a series of patient studies, our goal is to evaluate the efficacy and reliability of this method, providing a fresh perspective on the treatment of prostatic cysts.
This introduction aims to set the stage for a detailed discussion on the advantages and clinical implications of using real-time TRUS-guided TURP-Cyst, emphasizing its potential impact on patient care and surgical practices.
Materials and methods
A prospective study was conducted on eight consecutive patients with symptomatic prostatic cysts who underwent TURP-Cyst under real-time TRUS guidance between January 2019 and June 2023. Inclusion criteria were: (i) symptomatic prostatic cysts confirmed by transrectal ultrasound (TRUS), magnetic resonance imaging (MRI), or computed tomography (CT); (ii) cyst size greater than 1.5 cm; and (iii) willingness to participate in the study and provide informed consent. Exclusion criteria included active urinary tract infection, uncontrolled coagulopathy, and prior prostatic surgery.
Preoperative evaluation included a thorough medical history, physical examination, TRUS or MRI or CT imaging (Fig. 1), urine analysis, and measurement of serum prostate-specific antigen (PSA). Baseline lower urinary tract symptoms (LUTS) were assessed using the International Prostate Symptom Score (IPSS) and quality of life (QoL) questionnaires.
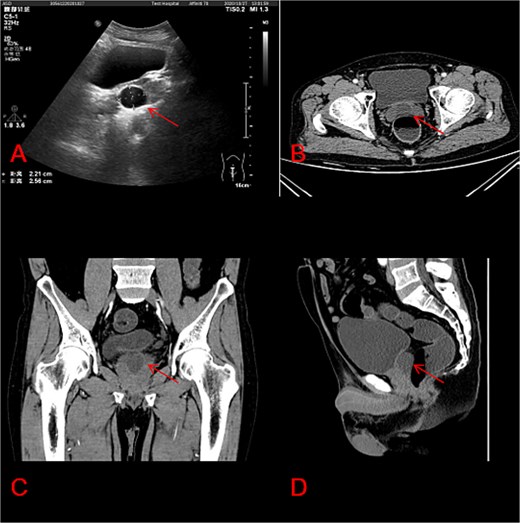
Characteristics of prostate cysts in ultrasound and CT imaging. (A) Prostate cysts in ultrasound; (B) prostate cysts in CT axial section; (C) prostate cysts in CT coronal section; (D) another view of prostate cysts in CT sagittal section.
Under general anesthesia, patients were positioned in lithotomy position, and a rigid TRUS probe was inserted rectally. The cyst was identified, and its boundaries were marked on the probe sheath for reference during the procedure. A 26 Fr resectoscope was then introduced, and the cyst was enucleated using standard TURP techniques, guided by real-time TRUS visualization. Special care was taken to preserve the prostatic capsule and avoid damage to the urethra, neurovascular bundles, and ejaculatory ducts. Postoperatively, a 20 Fr three-way Foley catheter was placed (Fig. 2). The surgical steps are demonstrated in the accompanying video (Supplementary Video 1), which shows real-time coordination between endoscopic visualization and TRUS imaging.

Real-time images are displayed on the cystourethroscope monitor and ultrasound during surgery.
Operative parameters such as cyst size, operative time, blood loss, and any complications were meticulously recorded. Intraoperative blood loss was estimated by measuring the volume of irrigation fluid used and subtracting the volume recovered through aspiration or outflow. The remaining fluid volume was assumed to be absorbed or lost due to hemodilution, from which we estimated blood loss based on visual assessment and clinical judgment. Follow-up evaluations were scheduled at one, three, and 6 months postoperatively. These assessments included TRUS to confirm cyst resolution, IPSS, and QoL scoring, and an evaluation of complications and recurrence rates. This structured follow-up allowed us to closely monitor patient recovery and outcomes, ensuring comprehensive data collection for analysis. All patients presented with lower urinary tract symptoms (LUTS), including frequency, urgency, weak stream, and intermittent flow. Some also reported a sensation of incomplete bladder emptying. These symptoms were quantified using the IPSS pre- and postoperatively.
By detailing these methods, we aim to provide a clear understanding of the surgical technique and its implementation, facilitating replication and further investigation into the efficacy and safety of real-time TRUS-guided TURP-Cyst for the treatment of prostatic cysts.
Unfortunately, technical limitations at the time of recording prevented us from capturing both the endoscopic and ultrasound images simultaneously. However, we are currently working on refining the surgical documentation process for future cases and will aim to produce higher-quality, synchronized recordings for subsequent publications.
Results
The mean age of the patients was 39.1 ± 8.7 years. Preoperative measurements using TRUS or MRI indicated a mean cyst size of 2.5 ± 0.3 cm (range 1.9–3.0 cm). All procedures were successfully completed without the need for conversion to open surgery or other endoscopic techniques. The mean operative time was 35.0 ± 16.0 min (range 10–60 min), and the mean blood loss was 14.0 ± 3.6 ml (range 10–20 ml) (Table 1). No major intraoperative complications such as capsular perforation or significant bleeding occurred.
Operative outcomes and demographic data for patients undergoing transurethral resection of prostatic cysts
| Variable . | Mean ± SD . | Range . |
|---|---|---|
| Age (years) | 39.1 ± 8.7 | 29–55 |
| Cyst size (cm) | 2.5 ± 0.3 | 1.9–3.0 |
| Operative time (min) | 35.0 ± 16.0 | 10–60 |
| Blood loss (ml) | 14.0 ± 3.6 | 10–20 |
| Variable . | Mean ± SD . | Range . |
|---|---|---|
| Age (years) | 39.1 ± 8.7 | 29–55 |
| Cyst size (cm) | 2.5 ± 0.3 | 1.9–3.0 |
| Operative time (min) | 35.0 ± 16.0 | 10–60 |
| Blood loss (ml) | 14.0 ± 3.6 | 10–20 |
Operative outcomes and demographic data for patients undergoing transurethral resection of prostatic cysts
| Variable . | Mean ± SD . | Range . |
|---|---|---|
| Age (years) | 39.1 ± 8.7 | 29–55 |
| Cyst size (cm) | 2.5 ± 0.3 | 1.9–3.0 |
| Operative time (min) | 35.0 ± 16.0 | 10–60 |
| Blood loss (ml) | 14.0 ± 3.6 | 10–20 |
| Variable . | Mean ± SD . | Range . |
|---|---|---|
| Age (years) | 39.1 ± 8.7 | 29–55 |
| Cyst size (cm) | 2.5 ± 0.3 | 1.9–3.0 |
| Operative time (min) | 35.0 ± 16.0 | 10–60 |
| Blood loss (ml) | 14.0 ± 3.6 | 10–20 |
The mean postoperative catheterization time was 1.9 ± 0.6 days (range, 1–3 days). All patients were discharged on the first postoperative day. At the 6-month follow-up, TRUS examination confirmed the complete resolution of the cysts in all cases. The mean IPSS score improved significantly from 19.5 ± 1.2 preoperatively to 7.5 ± 2.5 at 6 months (P < .001), and the mean QoL score improved from 4.4 ± 0.5 to 1.3 ± 0.5 (P < .001). There were no reports of significant complications such as urinary incontinence, erectile dysfunction, or stricture formation during the study period. No cases of cyst recurrence were observed (Table 2).
Postoperative outcomes and symptom improvement following transurethral resection of prostatic cysts at 6-month follow-up
| Variable . | Mean ± SD . | Range . | Improvement . |
|---|---|---|---|
| Catheterization time (days) | 1.9 ± 0.6 | 1–3 | |
| IPSS Score (preoperative) | 19.5 ± 1.2 | ||
| IPSS Score (6-month follow-up) | 7.5 ± 2.5 | Significantly improved (P < .001) | |
| QoL Score (preoperative) | 4.4 ± 0.5 | ||
| QoL Score (6-month follow-up) | 1.3 ± 0.5 | Significantly improved (P < .001) |
| Variable . | Mean ± SD . | Range . | Improvement . |
|---|---|---|---|
| Catheterization time (days) | 1.9 ± 0.6 | 1–3 | |
| IPSS Score (preoperative) | 19.5 ± 1.2 | ||
| IPSS Score (6-month follow-up) | 7.5 ± 2.5 | Significantly improved (P < .001) | |
| QoL Score (preoperative) | 4.4 ± 0.5 | ||
| QoL Score (6-month follow-up) | 1.3 ± 0.5 | Significantly improved (P < .001) |
Postoperative outcomes and symptom improvement following transurethral resection of prostatic cysts at 6-month follow-up
| Variable . | Mean ± SD . | Range . | Improvement . |
|---|---|---|---|
| Catheterization time (days) | 1.9 ± 0.6 | 1–3 | |
| IPSS Score (preoperative) | 19.5 ± 1.2 | ||
| IPSS Score (6-month follow-up) | 7.5 ± 2.5 | Significantly improved (P < .001) | |
| QoL Score (preoperative) | 4.4 ± 0.5 | ||
| QoL Score (6-month follow-up) | 1.3 ± 0.5 | Significantly improved (P < .001) |
| Variable . | Mean ± SD . | Range . | Improvement . |
|---|---|---|---|
| Catheterization time (days) | 1.9 ± 0.6 | 1–3 | |
| IPSS Score (preoperative) | 19.5 ± 1.2 | ||
| IPSS Score (6-month follow-up) | 7.5 ± 2.5 | Significantly improved (P < .001) | |
| QoL Score (preoperative) | 4.4 ± 0.5 | ||
| QoL Score (6-month follow-up) | 1.3 ± 0.5 | Significantly improved (P < .001) |
These results highlight the efficacy and safety of real-time TRUS-guided TURP-Cyst in treating symptomatic prostatic cysts, demonstrating significant improvements in symptoms and quality of life with minimal complications. The absence of cyst recurrence within the study period further supports the potential of this technique as an effective treatment option.
Discussion
Prostatic cysts are a rare condition, particularly those located in the midline, which have attracted clinical attention due to their potential to cause severe lower urinary tract symptoms (LUTS). Literature reports have established a link between prostatic cysts and LUTS, especially among younger patients where even relatively small cysts can lead to symptoms like urinary frequency, urgency, and voiding difficulties [1, 2]. These symptoms may be attributed to the compressive effects of the cyst’s location on the urethral outlet or bladder neck [8].
Various surgical approaches have been described for managing midline prostatic cysts, including transurethral unroofing, laser resection (e.g. holmium laser), laparoscopic cyst excision, and cyst puncture sclerotherapy [2–7]. For specific cases, such as anteriorly protruding midline cysts, traditional transurethral approaches may pose challenges, leading to innovative techniques like holmium laser-assisted cyst incision with cystoscope retroflexion [6]. These procedures not only ensure safety and efficacy but also minimize risks such as retrograde ejaculation [5].
Moreover, the nature and origin of the cyst influence treatment decisions [9]. Congenital prostatic cysts, such as those originating from remnants of the Müllerian duct system (e.g. prostatic utricle cysts), generally exhibit low malignant potential [10], yet they might contribute to fertility issues like infertility or hemospermia [11, 12]. In some instances, the presence of a cyst has been associated with elevated prostate-specific antigen (PSA) levels, necessitating biopsy to exclude malignancy despite the absence of radiographic evidence of malignant transformation [13].
In clinical practice, researchers emphasize the importance of individualized treatment plans, especially when balancing surgical intervention with preserving sexual function in young patients, such as avoiding complications like retrograde ejaculation caused by TURP [7]. Conservative management remains a reasonable option for small asymptomatic cysts, with regular follow-up recommended to monitor changes [14].
This study demonstrates the feasibility and preliminary effectiveness of real-time TRUS-guided TURP-Cyst for treating prostatic cysts. The technique allowed for precise cyst localization, real-time monitoring of cyst wall excision, and reduced risk of damage to adjacent structures. The improvements in IPSS and QoL scores, combined with the absence of significant complications and cyst recurrence, support the safety and efficacy of this approach.
Compared to traditional methods, real-time TRUS-guided TURP-Cyst offers several advantages. Real-time visualization enables meticulous dissection along the cyst wall, minimizing thermal injury to surrounding prostatic tissue and reducing the risk of complications such as incontinence and erectile dysfunction. The use of standard TURP instruments and techniques familiar to most urologists facilitates the adoption of this novel approach. Additionally, preserving the prostatic capsule and neurovascular bundles may further protect against postoperative functional impairment [2–7].
While our results are promising, this study is limited by its small sample size, single-center design, and relatively short follow-up period. Larger, multicenter studies with longer follow-ups are needed to confirm these findings and compare outcomes of real-time TRUS-guided TURP-Cyst with other established techniques for prostatic cyst management. Furthermore, cost-effectiveness analyses and patient-reported outcomes measures would provide valuable insights into the overall impact of this new approach. While formal uroflowmetry was not included as part of our initial protocol, we acknowledge its importance in assessing voiding function. Our primary outcome measures focused on symptom scores (IPSS and QoL) and imaging confirmation of cyst resolution. We agree that objective urodynamic data would strengthen future studies, and we plan to incorporate uroflowmetry in our follow-up research.
By addressing these limitations and continuing research efforts, we aim to refine clinical decision-making and improve patient care in the management of prostatic cysts.
Conclusion
Real-time TRUS-guided TURP-Cyst represents a safe and effective technique for treating prostatic cysts, offering precise localization of the cyst, reduced surgical trauma, and significant improvements in lower urinary tract symptoms (LUTS). This study introduces a novel method that integrates the advantages of TURP instrumentation with real-time TRUS guidance, contributing to the growing body of evidence supporting minimally invasive, image-guided approaches in the management of prostatic cysts.
The preliminary outcomes from this study are promising, demonstrating notable enhancements in patient quality of life and symptom relief without major complications. However, it is important to acknowledge the limitations of this research, including its small sample size, single-center design, and relatively short follow-up period.
Future research should focus on validating these findings in larger, multicenter studies with extended follow-up periods to assess long-term outcomes such as functional preservation and recurrence rates. Additionally, evaluating the cost-effectiveness and patient-reported outcomes of this technique will provide further insights into its overall impact and feasibility. By addressing these areas, we aim to refine clinical practices and improve patient care in the treatment of prostatic cysts.
In summary, the integration of real-time TRUS guidance with TURP-Cyst offers a promising advancement in the field, warranting further investigation and broader clinical application.
Author contributions
Fu-Xiang Lin (as the principal investigator, responsible for designing the study protocol, performing surgical procedures or conducting clinical research, analyzing data, and writing core sections of the paper), Fu Feng (have participated in patient care, data collection, or data analysis), Zhan-Ping Xu (as the corresponding author, responsibility for overall guidance of the research, including setting the research direction, integrating results, revising and submitting the manuscript, and being the point of contact with the journal editorial office).
Conflict of interest statement
None declared.
Funding
2023 Medical Research Project of Foshan Health Bureau (20230824A010489).



