-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Mahmoudi, Youness Slimi, Mohammed Frikal, Abdelali Guellil, Rachid Jabi, Mohammed Bouziane, Bone metaplasia in gallbladder lithiasis: an astonishing clinical phenomenon of a rare case, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf252, https://doi.org/10.1093/jscr/rjaf252
Close - Share Icon Share
Abstract
We present a rare case of acute cholecystitis in a 51-year-old patient. The gallbladder exhibited bone metaplasia, a condition infrequently observed in clinical practice. Acute cholecystitis was confirmed through clinical, radiological, and biological investigations, and the patient underwent cholecystectomy. Histopathological analysis of the surgical specimen revealed bone metaplasia in the gallbladder wall, a phenomenon associated with chronic inflammation due to gallstones. This article highlights the significance of post-surgical histopathological evaluation and discusses follow-up options for such rare conditions.
Introduction
Acute cholecystitis is an inflammation of the gallbladder, often caused by the presence of gallstones obstructing the cystic duct. It typically manifests as pain in the right upper quadrant of the abdomen, along with symptoms such as fever, nausea, and vomiting. While this condition is common, the occurrence of bone metaplasia in the gallbladder remains exceedingly rare and is poorly documented in medical literature.
Bone metaplasia refers to the transformation of non-bony tissues into bone tissue. Although this condition is more frequently observed in other organs, such as the lungs or soft tissues, after chronic irritation, its occurrence in the gallbladder, particularly in a patient with acute cholecystitis, is exceptional and raises questions regarding its underlying mechanisms and treatment options.
Here, we report a case of bone metaplasia discovered during histopathological examination of the gallbladder in a 51-year-old patient admitted for chronic cholecystitis.
Case presentation
A 51-year-old male was admitted to the emergency department with acute pain in the right upper quadrant of the abdomen, accompanied by nausea, vomiting, and moderate fever. His medical history included recurrent abdominal pain and digestive disturbances, with episodes of dyspepsia. On examination, the patient was febrile, with marked tenderness on palpation of the right upper quadrant and a positive Murphy’s sign.
Diagnostic work-up
The diagnosis of acute cholecystitis was promptly suspected based on clinical symptoms and confirmed by further investigations:
Laboratory results: Blood tests revealed elevated inflammatory markers (C-reactive protein and white blood cell count) and mild elevation of transaminases.
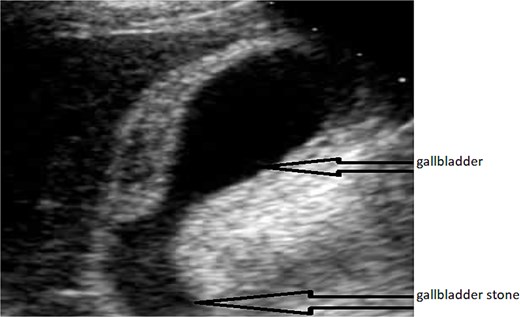
Abdominal ultrasound: A distended gallbladder with thickened walls and visible gallstones, typical of acute cholecystitis (Fig. 1).
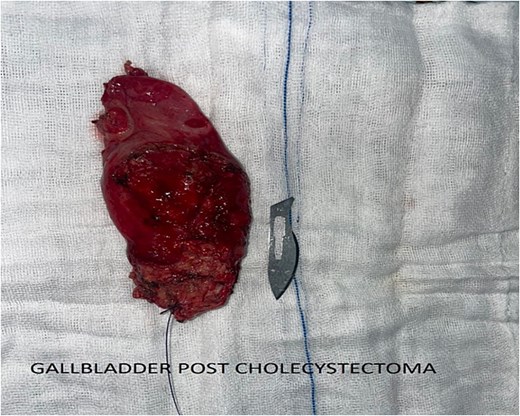
An urgent laparoscopic cholecystectomy was performed. However, upon histopathological analysis of the removed gallbladder (Fig. 2), bone metaplasia was identified in the gallbladder wall (Fig. 3). This finding was unexpected, although similar cases have been reported in the literature in the context of chronic gallbladder conditions.
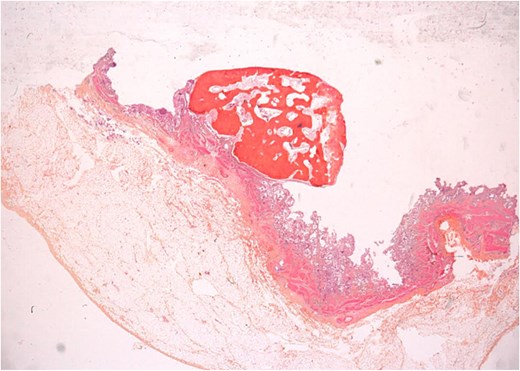
Microscopic image showing bone metaplasia in the gallbladder wall.
Bone metaplasia
Bone metaplasia in the gallbladder is an exceedingly rare pathological phenomenon. This process involves the transformation of normal gallbladder wall cells into bone-like cells in response to chronic irritation. The exact causes of this tissue transformation remain poorly understood, although it is hypothesized that persistent inflammation may promote this metaplasia. The process is analogous to the formation of bone tissue in non-bony tissues, as seen in cartilaginous or muscular tissues.
In our patient’s case, the presence of gallstones and acute cholecystitis likely triggered this histological transformation. Although bone metaplasia is typically not associated with immediate complications, it remains an area of surveillance in the context of chronic gallbladder diseases.
Therapeutic management
The patient underwent urgent cholecystectomy, the standard treatment for acute cholecystitis. Following the detection of bone metaplasia, no specific treatment was deemed necessary, as this condition generally does not pose a direct risk to the patient’s health. However, postoperative follow-up was recommended, including regular monitoring to prevent any long-term complications.
Discussion
Bone metaplasia is a rare phenomenon often associated with chronic inflammatory processes or persistent mechanical stimuli. In the case of the gallbladder, a recent study describes a similar case and suggests that chronic inflammation, such as that observed in cholecystitis, could induce the differentiation of mesenchymal cells into osteoblasts, leading to bone tissue formation [1]. This hypothesis is supported by the frequent occurrence of bone metaplasia in contexts of chronic inflammatory diseases.
Another study reported a case of bone metaplasia in the context of cholesterol polyps in the gallbladder [2]. The authors emphasized that bone metaplasia might be an adaptive response to prolonged inflammatory or mechanical stimuli, although the exact mechanisms remain unclear. This observation reinforces the idea that bone metaplasia is a rare but significant entity in gallbladder pathology.
A review by C. Ortiz-Hidalgo examined reported cases of bone metaplasia in the gallbladder and emphasized that this entity is often associated with chronic inflammatory diseases, such as cholecystitis [3]. The authors also discussed potential mechanisms, including the role of pro-inflammatory cytokines and growth factors in osteogenic differentiation.
Another study described a case of bone metaplasia in the gallbladder of a patient with chronic cholecystitis [4]. The authors suggested that bone metaplasia might result from a reparative response to prolonged inflammation, although further studies are needed to confirm this hypothesis.
Furthermore, an in-depth study of the molecular and cellular mechanisms of heterotopic ossification provided valuable insights into the underlying processes of bone metaplasia [5]. The authors identified several signaling pathways, including the bone morphogenetic protein pathway and the Wnt pathway, which play key roles in the differentiation of mesenchymal cells into osteoblasts. These mechanisms may also be involved in gallbladder bone metaplasia, though further research is needed to confirm this hypothesis.
All the aforementioned studies suggest that chronic inflammation plays a crucial role in the pathogenesis of this tissue transformation.
Conclusion
Bone metaplasia in the gallbladder remains a rare entity, often discovered incidentally during histopathological examination. While its pathogenesis is not fully elucidated, chronic inflammation seems to play a pivotal role. This case underscores the importance of thorough histological evaluation, even in seemingly routine clinical contexts such as acute cholecystitis.
Author contributions
M.M. has written the article, consulted the patient, and prepared the patient for surgery and participated in the surgery. S.Y. has helped collecting data. F.M. has helped collecting data. G.A. supervised the writing of manuscript. J.R. supervised the writing of manuscript. B.M. has supervised the writing of the paper, and been the leader surgeon of the case.
Conflict of interest statement
None declared.
Funding
None declared.
References
Rege TA, Vargas SO. Cholecystitis and cholelithiasis associated with an intramural fasciitis-like proliferation and osseous metaplasia.



