-
PDF
- Split View
-
Views
-
Cite
Cite
Frank Andrés Álvarez Vásquez, Juan Pablo Zaraza, Andrés Camilo Herrera, Iván Enrique Rodríguez, Reconstruction of thoracolumbar myelomeningocele using double keystone flap in a neonate: a Colombian pediatric case, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf222, https://doi.org/10.1093/jscr/rjaf222
Close - Share Icon Share
Abstract
Myelomeningocele (MMC) is a congenital neural tube defect requiring early surgical intervention to prevent severe complications. Surgical closure can be challenging due to the possibility of complications such as partial flap loss, necrosis, wound dehiscence, and cerebrospinal fluid leakage. The Keystone Design Perforator Island Flap is a versatile option for covering large defects in complex cases such as MMC. This case presents the successful application of a Type III Keystone flap to repair an extensive thoracolumbar defect in a neonate with MMC, providing effective coverage and reducing complications, positioning itself as a trustworthy technique in pediatric reconstructive surgery.
Introduction
Neural tube defects (NTDs) are a group of congenital malformations secondary to failure in the fusion of the vertebral arches during early fetal development. Myelomeningocele (MMC) is the most common and severe form of open spina bifida (SB) compatible with life. MMC is manifested by the protrusion of the meninges and spinal cord through a defect in the vertebral column, forming a visible mass on the back of the fetus or neonate [1, 2]. Its etiology is multifactorial, including genetic factors, nutritional deficiencies, and environmental factors such as exposure to teratogens, maternal diabetes, and maternal obesity [1–3].
The global prevalence of NTDs is estimated at 4 cases per 1000 live births, being lower in industrialized countries like the USA and most European countries, where it ranges from 0.5 to 0.8 per 1000 live births annually [1, 3]. However, it is considerably higher in developing countries. In Colombia, the incidence of NTDs is approximately 3 per 1000 live births, above the global average [1, 4], highlighting the importance of implementing strategies to improve folic acid supplementation, increase access to prenatal healthcare services, and reduce maternal malnutrition rates.
Early correction of MMC is crucial to prevent severe complications such as neurological damage, infections like meningitis, and physical deformities that could result in paralysis, and the neurosurgeon must perform this intervention within the first 24–48 h after birth to minimize the risk of these complications [5]. Immediate reconstruction is required to ensure a watertight repair of the dura and soft tissue coverage. Nowadays, intrauterine repair of MMC is possible with adequate fetal and maternal outcomes and is performed to protect the nerve fibers of the spinal cord from the toxic effect of amniotic fluid to prevent the occurrence of ventriculomegaly and hindbrain herniation [6].
However, large residual defects represent a challenge; traditional techniques, such as the direct primary closure are not always sufficient for an effective closure; but also transposed muscle flaps or skin grafts may lead to significant morbidity at the donor site, prolonged healing, and complications such as partial necrosis, dehiscence, and cerebrospinal fluid leaks. In this context, the KDPIF has emerged as a promising alternative, providing an effective solution for large defects (Fig. 1) [6–9].
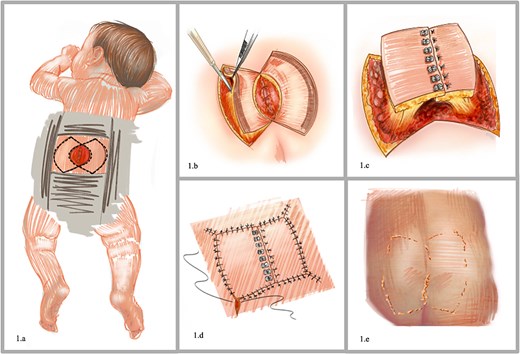
Preoperative planning. (a) Coverage defect in the lower lumbar region secondary to the resection of a myelomeningocele. (b) Diagram of the keystone perforator island flap design. (c) Advancements flaps. (d) Surgical wound closure. (e) Postoperative outcome with immediate defect closure.
Clinical case
A 1-month-old male with a history of myelomeningocele repair on day six of life developed surgical wound dehiscence, which necessitated reoperation. Following two unsuccessful repair attempts, he was referred to plastic surgery after excluding cerebrospinal fluid (CSF) fistula.
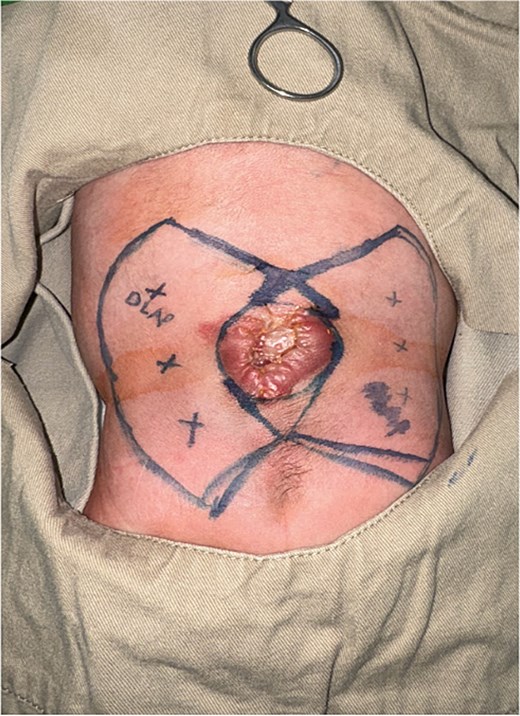
On initial examination, a fibrinoid mycotic eschar was noted in the dorsolumbar region, involving 5% of the total body surface area, with severe trophic changes in the perilesional tissues. During surgical escharectomy, a defect measuring 4 × 5 cm (20 cm2) was identified, involving the skin, subcutaneous tissue, and deep fascia, with exposure of the meningeal sac but no macroscopic evidence of infection or fistula (Fig. 2).

The reconstruction was planned using a Type III Keystone flap based on clusters of perforators from the left dorsolumbar and right lumbogluteal regions (Fig. 3). First, two prevertebral fascia flaps were dissected to cover the meningeal sac, then flap dissection was performed layer by layer, identifying and preserving the microvascular clusters to ensure their viability. The flaps were transferred and positioned over the defect, ensuring complete coverage of the meningeal sac (Fig. 4). Layered closure was achieved with a variant of the described classic closure of the type III flap of a straight line between the intersection of the flaps to a Z-shaped closure, with intraoperative evidence of adequate perfusion and no signs of congestion or vascular compromise in the immediate postoperative period and during postoperative follow-up (Fig. 5).

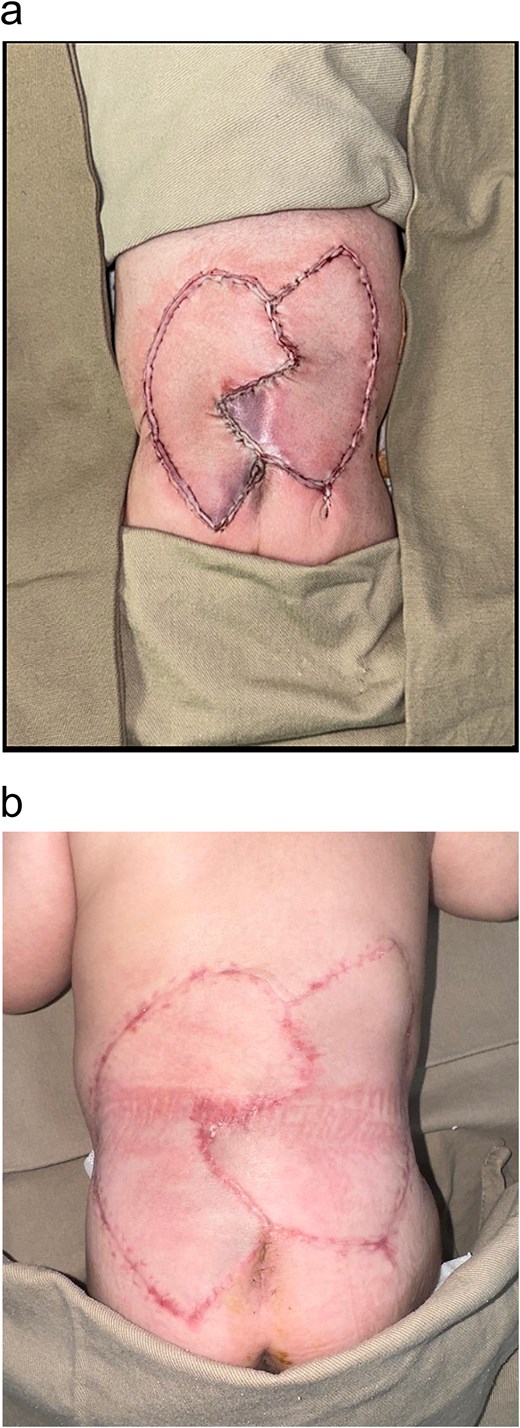
(a) Immediate reconstruction with a type III KDPIF with a Z-shaped closure variation. (b) 3 months postoperative follow-up.
Discussion
The KDPIF has become a highly versatile and efficient option for reconstruction due to its anatomical and functional design, which optimizes clinical outcomes. Unlike conventional flaps, the KDPIF leverages the reliable vascular supply provided by septocutaneous, musculocutaneous, and fasciocutaneous perforators, ensuring flap viability and durability [7, 8].
The “keystone” flap resembles an essential component in Roman arch architecture, which serves as a structural support to maintain the stability of the entire structure [7–9].
The main features of this flap are listed below:
Robust vascularization relies on pedicle-based irrigation, which also increases range of motion without compromising its viability [7, 8].
Possibility to achieve primary closure of both the defect and the donor area [7–9].
Like-to-like and anatomical subunit reconstruction, which contributes to obtaining superior aesthetic results [8–10].
Reducing surgical times and dissection does not require advanced instrumentation [7, 9].
It is performed in patients with irradiated tissues and a history of trauma or comorbidities that advise against extensive or microsurgical procedures [8, 9].
The classification of Keystone flaps includes four types, each suited to different defect sizes and locations. Type III, utilizing double keystone-shaped flaps, is indicated for large defects [7, 8].
In our case, a bilateral Type III Keystone flap, supplied by perforators from the dorsal intercostal artery, musculocutaneous perforators of the latissimus dorsi, lumbosacral arteries, and superior gluteal arteries, was used to close an extensive thoracolumbar defect in a newborn with MMC. This type of flap is ideal for defects larger than 5 cm, providing broad coverage without compromising essential vascular supply [7, 10]. This case highlights the potential of the Keystone flap as a crucial tool in the reconstruction of complex MMCs resection defects emphasizing its efficacy, safety, and adaptability in challenging surgical scenarios [10, 11]. Its application in pediatric patients in Colombia opens new opportunities to improve surgical care for vulnerable populations, establishing a valuable precedent for managing complex congenital conditions.
Conclusion
The KDPIF design allows excellent adaptation to body contours making it an efficient and safe option for reconstructing extensive and complex defects originated by trauma, burns, cancer, and congenital defects such as MMC. In this case, the flap application completely closed the thoracolumbar defect, providing stable and aesthetically suitable tissue coverage with long-term durability.
The incorporation of techniques like the KDPIF into clinical practice may represent a significant improvement in surgical outcomes. This innovative approach sets an important precedent for reconstructive plastic surgery in neonates with congenital malformations, offering an effective solution for challenging defects and expanding treatment possibilities in high-demand contexts.
Conflict of interest statement
None declared.
Funding
None declared.



