-
PDF
- Split View
-
Views
-
Cite
Cite
Tarik Deflaoui, Yassir Akil, Anas Derkaoui, Rihab Amara, Abdelali Guellil, Rachid Jabi, Mohammed Bouziane, Use of the omentum in the management of mesenteric contusions: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf193, https://doi.org/10.1093/jscr/rjaf193
Close - Share Icon Share
Abstract
Closed abdominal trauma can result in severe mesenteric injury, potentially progressing to intestinal necrosis requiring resection. We report the case of a 24-year-old female patient, victim of a road traffic accident, with two mesenteric contusions: one responsible for intestinal necrosis requiring a double stoma, and the other located upstream, with preservation of a feeding vessel. An innovative technique was used to preserve this vascularization: a pedicled omental flap, still attached to the omental apron, was mobilized to cover and stabilize the mesenteric vessel. The omentum was fixed using resorbable sutures to ensure stabilization without compromising vascularization. The proximal location of the affected intestinal segment allowed for tension-free omental transposition. The post-operative outcome was favorable, with continuity restored two months later. This case highlights the importance of the role of the omentum in digestive reconstruction and vascular preservation, and proposes a reflection on its integration into standardized surgical protocols.
Introduction
Closed abdominal trauma with mesenteric involvement is rare but potentially serious, potentially progressing to intestinal ischemia requiring resection [1]. The omentum, a richly vascularized structure with angiogenic properties, plays an essential role in tissue repair and vascular protection [2, 3]. Although its use is well documented in contexts such as prevention of anastomotic fistulas or coverage of vascular grafts, its application in the management of mesenteric trauma remains less explored.
We present here an illustrative case of the use of the omentum to stabilize a threatened mesenteric vessel after severe abdominal trauma, and discuss its potential in surgical practice.
Case presentation
A 24-year-old female patient with no previous medical history was involved in a road traffic accident. On admission, the patient was hemodynamically and respiratory stable (BP 120/70 mmHg, HR 80 bpm, SaO₂ 97% on 1 L O₂). Abdominal examination revealed mild distension with diffuse tenderness, more marked in the left iliac fossa. Biological examinations showed an initial hyperleukocytosis, anemia, elevated C-reactive protein, moderate ionic disturbances, and a slight increase in lipase. A thoraco-abdomino-pelvic computerized tomography (CT) scan revealed abundant hemoperitoneum, a mesenteric laceration 60 cm from Treitz’s angle and a second mesenteric laceration 2.2 m downstream, with integrity of the colon, spleen, and liver.
An emergency exploratory laparotomy was performed. Exploration confirmed the presence of intestinal ischemia secondary to the distal mesenteric laceration, necessitating a 30 cm segmental resection of the small bowel with a double ileal stoma (Fig. 1). A second, more proximal mesenteric lesion, located 60 cm from Treitz’s angle, had a functional feeder vessel despite compromised vascularization.

To preserve the mesenteric vascularization and avoid secondary ischemia, a pedicled omental flap, remaining attached to the omental apron, was carefully mobilized. The flap was transposed and sutured to the mesenteric border of the intestine using resorbable 3/0 sutures, ensuring contact with the injured vessel without exerting excessive traction (Fig. 2 and Video 1).
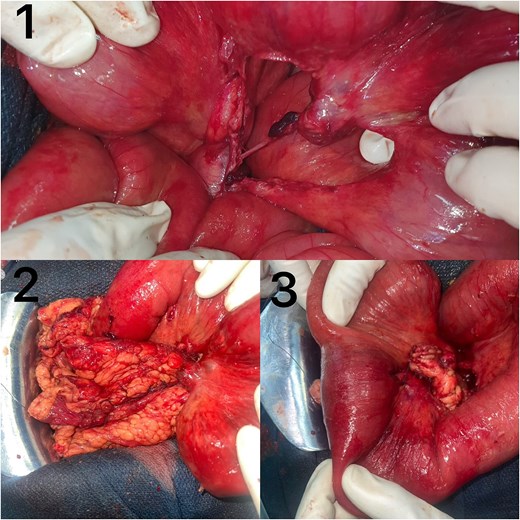
(1) Mesenteric contusion with a preserved nourishing vessel ensuring a viable ileal segment. (2) Anterior view of the omental coverage of the nourishing vessel. (3) Posterior view of the omental coverage of the nourishing vessel, also fixed to the posterior mesenteric border of the ileum.
The choice of this technique was dictated by several intraoperative considerations:
Avoiding further intestinal resection by preserving the threatened mesenteric vessel.
Minimizing thrombosis risk through a mechanical and angiogenic protective effect of the omentum.
The proximal location of the lesion (60 cm from Treitz) allowed for tension-free transposition, unlike in more distal lesions where greater mobilization might have been required.
The post-operative course was marked by good clinical recovery. Oral feeding was gradually resumed. Two months after the initial operation, continuity was successfully restored, with no post-operative complications.
Discussion
Mesenteric trauma accounts for ⁓1%–5% of traumatic abdominal injuries [4]. They are associated with a risk of intestinal necrosis due to underlying vascular damage. Imaging, in particular CT with injection, is essential to identify signs of ischemia and guide management [5]. Surgical management relies on systematic exploration of the mesentery and intestine to assess tissue viability. In cases of extensive necrosis, resection with delayed restoration of continuity is preferred, especially in unstable patients [6].
The omentum is a multifunctional structure with angiogenic, anti-inflammatory, and immunomodulatory properties. It is commonly used in digestive and vascular surgery for:
Promoting revascularization in cases of vascular injury [7].
Protecting intestinal anastomoses and preventing fistulas [8].
Stabilizing fragile structures, such as vascular grafts or threatened intestinal segments [9].
In our case, using the omentum to stabilize the mesenteric vessel ensured its patency and prevented further intestinal resection. When compared to conventional approaches:
Observation alone carries a high risk of delayed thrombosis and ischemia.
Vascular grafting is more complex, requiring microvascular anastomoses with inherent thrombosis risks.
Immediate resection could have led to unnecessary loss of viable intestine, increasing morbidity.
Integrating the omentum into a standardized mesenteric trauma management protocol could be based on the following criteria:
Presence of residual mesenteric vascularization, suggesting a chance of recovery.
Absence of complete mesenteric thrombosis, which would necessitate resection.
Hemodynamic stability, allowing for a conservative approach.
The proximal location of the lesion is a key factor in determining feasibility. In our case, the segment was close enough to Treitz’s angle to allow tension-free omental transposition. In more distal lesions, extended mobilization may be required, posing a risk of traction-related ischemia.
Future prospective studies comparing omental transposition with conventional techniques could help refine its indications and optimize its use in digestive trauma.
Conclusion
This case illustrates the value of the omentum in the management of traumatic mesenteric contusions. Its role in vascular stabilization and prevention of intestinal ischemia could be further explored in digestive reconstruction protocols. Prospective, comparative studies are needed to assess the effectiveness of this technique compared with conventional approaches, and to define clear indications.
Conflict of interest statement
None declared.
Funding
None declared.
References
Collins D, Hogan AM, O’Shea D, Winter DC.



