-
PDF
- Split View
-
Views
-
Cite
Cite
Hamza A Abdul-Hafez, Manar Gharaba, Lubna Shihada, Mahmoud N Khadra, Mohammed A Barakat, Laith B Nassar, Khaled S Hashash, Spontaneous renal calyceal rupture from distal ureteric tiny stone: a rare case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf185, https://doi.org/10.1093/jscr/rjaf185
Close - Share Icon Share
Abstract
Pelvicalyceal rupture is a rare but clinically significant condition often associated with ureteral obstruction. We report a 24-year-old female presenting with acute right flank pain, nausea, and vomiting caused by a 3 mm distal ureteric stone. Imaging revealed hydroureteronephrosis with urine extravasation. Immediate double-J stent placement successfully resolved the obstruction and rupture. At a one-month follow-up, the patient showed complete recovery without recurrence. This case highlights the importance of timely diagnosis and intervention, even in tiny ureteric stones, to prevent severe complications.
Introduction
Pelvicalyceal rupture is a rare yet clinically serious condition characterized by a breach in the renal collecting system [1]. This occurrence is frequently caused by trauma. In non-traumatic instances, calculi are the leading cause of ureteral and renal pelvis rupture [2]. Other uncommon causes include ureteral blockage caused by posterior urethral valves, prostatic hyperplasia, pelvic neoplasms, and urinary tract infections [3].
The clinical manifestation of pelvicalyceal rupture can range from mild flank discomfort to systemic infection or sepsis in more severe situations [1]. Imaging methods, particularly computed tomography (CT), are critical for identifying urine leakage and determining the degree of the damage [4]. Early detection and treatment are critical for preventing complications such as urinomas, abscesses, and irreversible kidney impairment [2].
Here, we describe a rare case of a patient presenting with calyceal rupture as the first manifestation of a small ureteric stone. The patient was managed successfully with double-J (D-J) stent insertion with good clinical outcomes.
Case presentation
A 24-year-old female presented to our emergency department with a sudden onset of right-sided flank pain for two hours. The pain radiated to the groin and was accompanied by nausea and vomiting. Despite taking analgesic medications, her symptoms persisted, prompting her to seek medical help. She denied any history of previous similar pain, recent fever, dysuria, or hematuria. There was no history of trauma, recent surgeries, or notable past medical and surgical history.
On examination, her vital signs were within normal limits except for tachycardia, with a heart rate of 110 beats per minute. Her blood pressure was 125/80 mmHg, oxygen saturation was 98%, and she was afebrile. Abdominal examination revealed tenderness in the right side of the abdomen and costovertebral angle tenderness. Other systemic examinations, including cardiovascular, respiratory, and neurological systems, were unremarkable.
Laboratory findings showed red blood cells (6–10 per HPF) and white blood cells (10–20 per HPF) in her urine, with negative leukocyte esterase and nitrite. Other laboratory findings, including hemoglobin levels, coagulation profile, serum creatinine, blood urea nitrogen, inflammatory markers, and pregnancy test, were within normal limits.
Given the patient's symptoms, an urgent abdominal ultrasound was performed, which demonstrated moderate right-sided hydroureteronephrosis with perinephric-free fluid. Both kidneys appeared normal in size, shape, echostructure, and position. As a result, a contrast-enhanced CT scan of the abdomen and pelvis was performed, revealing an enlarged and edematous right kidney with moderate hydroureteronephrosis. A 3 mm distal ureteric stone was identified ~1.5 cm proximal to the vesicoureteric junction (Fig. 1). Moreover, significant perinephric and periureteral fluid and fat stranding were also noted (Fig. 1). Additionally, there was evidence of partially delayed calyceal contrast excretion with extravasation but no pelvic or ureteric excretion 20 minutes post-contrast injection (Fig. 1). These clinical and imaging findings were highly suggestive of renal calyceal rupture secondary to ureteric obstruction.
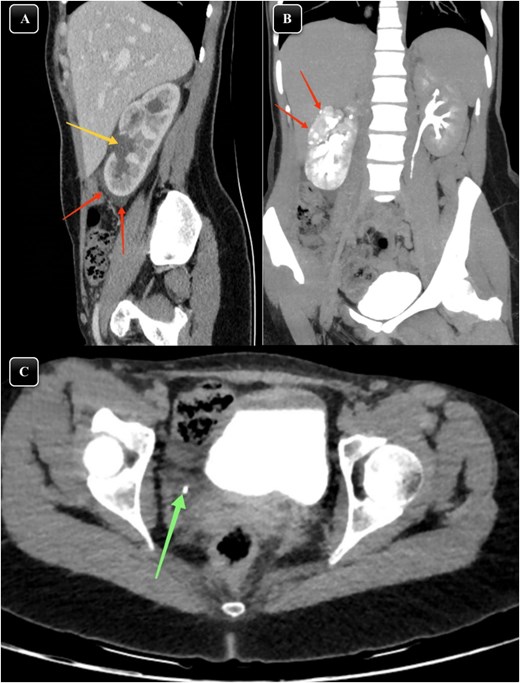
(A) Sagittal section of a contrasted CT scan obtained at the venous phase showing moderate right hydronephrosis (arrow) with perinephric free fluid and fat stranding (arrow). (B) MIP reconstructed coronal images of contrasted CT scans obtained at delayed phases showing delayed renal excretion of the right kidney with minimal contrast extravasation out of the pelvicalyceal system (arrows). (C) Axial section of contrasted CT scan showing distal right ureteric stone about 1.5 cm away from vesicoureteric junction (arrow) surrounded by minimal fat stranding and fluid.
However, the patient’s condition deteriorated despite intravenous analgesics, prompting urgent intervention. She was transferred to the operation room on the same day for insertion of a double J-stent. Under general anesthesia, a D-J stent was successfully placed in the right ureter using a cystoscope.
Postoperatively, the patient was admitted for monitoring and received intravenous fluids, analgesics, and antibiotics. Her clinical condition improved significantly, and follow-up imaging showed resolution of the obstruction and extravasation (Fig. 2). She was discharged in good clinical condition, with no pain or urinary symptoms. At the one-month follow-up, the D-J stent was removed without complications. The patient reported no recurrence of symptoms, and her clinical outcomes remained good.
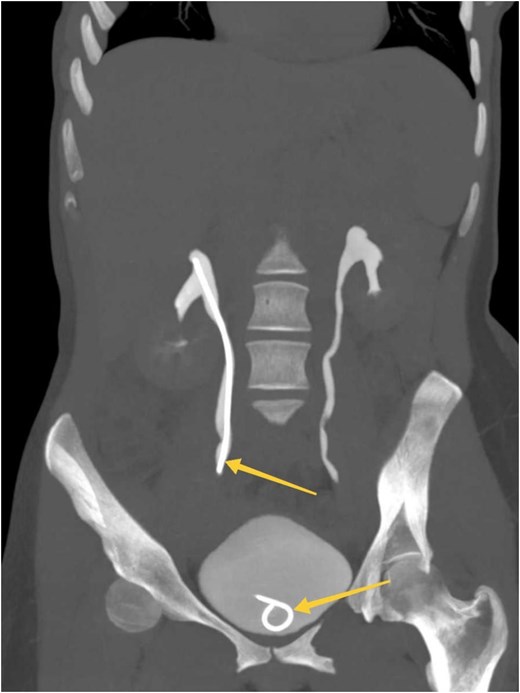
MIP reconstructed coronal images of contrasted CT scan obtained at delayed phases (bone window) showing symmetrical bilateral renal excretion with D-J stent in the right ureter and bladder (arrows).
Discussion
Spontaneous rupture of the calyceal system is an unusual clinical condition characterized by extravasation of the urine from the urinary collecting system, occurring at any level from the renal calyx to the urethra [5, 6]. Based on anatomical location, spontaneous renal rupture can be classified into three categories, including rupture of the renal parenchyma, rupture of the renal collecting system, or a combination of both [7]. The majority of cases have been identified at the fornix level, which is the most vulnerable point to rupture of the collecting system.
Spontaneous or non-traumatic rupture often occurs due to increased pressure within the urinary collecting system due to any cause of obstruction. Ureteric calculi are the leading cause, accounting for ~75% of cases. These calculi block urine flow, leading to elevated intrarenal pressure and subsequent rupture. Other causes include extrinsic compression from tumor or pregnancy, or intrinsic causes, such as tumors within the urinary tract or hematomas can limit urine flow and cause rupture. Other ruptures are related to iatrogenic causes like endoscopic interventions or lithotripsy. Pyelonephritis or other severe infections may contribute by inducing inflammation and swelling, leading to increased intrarenal pressure and rupture [8–10].
The likelihood of stone passage depends on stone size. Literature indicates that stones <5 mm typically pass spontaneously in 98% of cases, with minimal complications. Stones measuring 5–7 mm pass spontaneously in 60% of cases, while stones 7–9 mm and >9 mm have passage rates of 48% and 25%, respectively. However, stones <5 mm rarely cause obstruction severe enough to result in calyceal rupture. In our case, a 3 mm stone located 1.5 cm proximal to the vesicoureteric junction caused obstruction and rupture. These findings align with previous case reported by Khashan et al., who discuss a similar case involving a 3 mm stone causing obstructive uropathy and calyceal rupture [9–12].
Similar findings were reported by Assaker et al., who observed a 4 mm stone causing obstruction, and Gershman et al., who noted higher rates of spontaneous rupture with distal ureteric stones compared to proximal ones (76.7% vs. 24.3%). The greater likelihood of rupture with smaller distal ureteric stones is attributed to prolonged obstruction and the narrower diameter of the distal ureter [10].
Clinically, patients with spontaneous ureteral rupture present with nonspecific findings ranging from flank pain to acute abdomen [12]. In our case, the patient presented with right flank pain, vomiting, fever and chills. This presentation aligns with findings from Chen et al., who reported that 66.7% of patients with spontaneous rupture presented with acute flank pain, while 33.3% experienced acute abdominal pain [5]. In Table 1, we provide a summary of previous reported similar cases.
| # . | Author, year . | Age/gender . | Clinical presentation . | Risk factors . | Stone size . | Stone site . | CT findings . | Management . |
|---|---|---|---|---|---|---|---|---|
| 1 | Yin et al., 2022 [7] | 46/M | Left lower back pain, oliguria, no fever | A long history of renal stones, multiple ESWL treatments | Not specified | Left kidney | Perirenal hematoma, non-specific renal rupture | Nephrectomy due to renal parenchymal rupture |
| 2 | Khashan et al., 2023 [9] | 19/F | Acute right-sided lower abdominal pain, nausea, vomiting, chills, and no fever | N/A | 3 mm | Right ureterovesical junction | Mild to moderate right hydroureteronephrosis, perinephric edema | Conservative: IV fluids, ketorolac, ceftriaxone, tamsulosin, close monitoring, and passed stone spontaneously |
| 3 | Liao et al., 2021 [13] | 63/F | Acute flank pain, mild right flank tenderness | History of similar symptoms 1 month before | Largest: 1.9 × 1.0 cm | Right renal pelvis | Hydronephrosis, multiple calculi, renal calyceal rupture with extravasation | D-J ureteral stent placement |
| 4 | Yanaral et al., 2017 [14] | 86/F | Left flank pain for 7 days, nausea, vomiting | left kidney stone a month ago | 8 mm | Left renal pelvis | Hydronephrosis, contrast extravasation, and perirenal fluid | D-J ureteral stent placement and shock wave lithotripsy |
| 5 | Okpii et al., 2022 [15] | 77/M | Worsening left-sided abdominal pain 3 days prior to presentation | Suprapubic catheter due to multiple urethral strictures post-prostatectomy procedure | 12 mm | Left vesico-ureteric junction | Intra-abdominal free fluid on the left side, rupture of the left renal calyces with contrast extravasation | Nephrostomy due to multiple complex urethral strictures, laser stone fragmentation |
| 6 | Weber et al., 2022 [16] | 33/M | Cough, vomiting, flank pain, and inability to urinate | Recurrent ureteral stones | Not specified | Right kidney | A column of contrast in the right renal pelvis and ureter with a moderate amount of extraluminal contrast surrounding the right kidney | Treated conservatively |
| 7 | Porfyris et al., 2016 [17] | 75/M | Right flank pain and three episodes of vomiting | N/A | 5 mm | Right ureterovesical junction | Right hydroureteronephrosis, contrast extravasation, and retroperitoneum fluid collection | Antibiotics, ultrasound-guided nephrostomy tube insertion. |
| 8 | Pampana et al., 2013 [18] | 69/F | Right-sided flank pain that started 6 hours before, nausea | History of renal calculi in the younger age | Not specified | Right kidney | Contrast medium extravasation | D-J ureteral stent placement |
| 9 | Kheiri et al., 2018 [19] | 52/F | Right lower abdominal pain for 1 day | History of UTI | 7 mm | Right ureterovesical junction | Hydroureteronephrosis and ruptured calyx | D-J ureteral stent placement and lithotripsy |
| 10 | Taşkınlar et al., 2016 [20] | 1.5/F | Fever, vomiting, and abdominal pain | Retroperitoneal tumor pushing left kidney, UTI | 10 mm | Left kidney | Left perirenal urinoma and an extruded calculus in the urinoma, contrast extravasation. | D-J ureteral stent placement |
| 11 | Tas et al., 2013 [21] | 55/F | Acute flank pain for the last 6 days | History of right distal uretral stone | 6 mm | Right distal ureter | Rupture of right renal pelvis in two points, peripheral fluid accumulation, contrast extravasation | Ureteroscopic lithotripsy, D-J stent, and drain placement |
| 12 | Assaker et al., 2020 [10] | 53/M | Right back pain 4 hours prior to presentation, nausea, vomiting, no fever | Benign prostatic hyperplasia and chronic right hydrocele | 4 mm | Right ureterovesical junction | Fluid extravasation around the proximal ureter and at the perinephric renal space | D-J ureteral stent placement |
| 13 | Reva et al., 2013 [22] | 29/M | Left flank pain, nausea, and macroscopic hematuria | Klinefelter syndrome | 4 mm | Left ureterovesical junction | Contrast extravasation | D-J ureteral stent placement |
| 14 | Díaz et l., 2011 [23] | 46/M | Left flank pain | N/A | 7 mm | Left ureterovesical junction | Contrast extravasation at the level of the left renal pelvis | Double pigtail catheter for a two-week period |
| 15 | Prem et al., 2021 [24] | 30/F | Right-sided abdominal pain, and fever for a month. | Right urolithiasis and pyelonephritis treatment over 3 years. | Multiple with variable sizes | Right pelvis, upper ureter, and multiple calculi in right lower ureter | Ruptured right kidney, hydronephrosis, multiple renal and ureteric calculi, Urinoma formation in subcapsular region of liver, pneumoperitoneum | Exploratory laparotomy and right nephroureterectomy |
| 16 | Cruz et al., 2021 [8] | 36/F | Left flank pain since 2 days prior, nausea and vomiting, no fever | Previous nephrolithiasis history | 7 mm (proximal one) and 3 mm (distal one). | Proximal left ureter and another one distally | Left-sided hydronephrosis, multiple ureteral stones, trace left perinephric fluid. | Conservative treatment with alpha-blockers, analgesics, and antiemetics |
| 17 | Koktener et al., 2007 [6] | 63/M | Right-sided flank pain | History of T-cell lymphoma, and right-sided nephrolithiasis, chemotherapy | <5 mm | 3 cm caudal to the iliac bifurcation at right ureter | Contrast extravasation, a large amount of fluid around the right kidney, liver, pararenal, and paracolic region | D-J ureteral stent placement |
| 18 | Our case | 24/F | Right-sided flank pain | N/A | 3 mm | Right ureter about 1.5 cm away from vesicoureteric junction | Enlarged and edematous right-sided kidney with moderate hydroureteronephrosis. In addition to the presence of a tiny distal ureteric stone measuring 3 mm located about 1.5 cm away from vesicoureteric junction | D-J ureteral stent placement |
| # . | Author, year . | Age/gender . | Clinical presentation . | Risk factors . | Stone size . | Stone site . | CT findings . | Management . |
|---|---|---|---|---|---|---|---|---|
| 1 | Yin et al., 2022 [7] | 46/M | Left lower back pain, oliguria, no fever | A long history of renal stones, multiple ESWL treatments | Not specified | Left kidney | Perirenal hematoma, non-specific renal rupture | Nephrectomy due to renal parenchymal rupture |
| 2 | Khashan et al., 2023 [9] | 19/F | Acute right-sided lower abdominal pain, nausea, vomiting, chills, and no fever | N/A | 3 mm | Right ureterovesical junction | Mild to moderate right hydroureteronephrosis, perinephric edema | Conservative: IV fluids, ketorolac, ceftriaxone, tamsulosin, close monitoring, and passed stone spontaneously |
| 3 | Liao et al., 2021 [13] | 63/F | Acute flank pain, mild right flank tenderness | History of similar symptoms 1 month before | Largest: 1.9 × 1.0 cm | Right renal pelvis | Hydronephrosis, multiple calculi, renal calyceal rupture with extravasation | D-J ureteral stent placement |
| 4 | Yanaral et al., 2017 [14] | 86/F | Left flank pain for 7 days, nausea, vomiting | left kidney stone a month ago | 8 mm | Left renal pelvis | Hydronephrosis, contrast extravasation, and perirenal fluid | D-J ureteral stent placement and shock wave lithotripsy |
| 5 | Okpii et al., 2022 [15] | 77/M | Worsening left-sided abdominal pain 3 days prior to presentation | Suprapubic catheter due to multiple urethral strictures post-prostatectomy procedure | 12 mm | Left vesico-ureteric junction | Intra-abdominal free fluid on the left side, rupture of the left renal calyces with contrast extravasation | Nephrostomy due to multiple complex urethral strictures, laser stone fragmentation |
| 6 | Weber et al., 2022 [16] | 33/M | Cough, vomiting, flank pain, and inability to urinate | Recurrent ureteral stones | Not specified | Right kidney | A column of contrast in the right renal pelvis and ureter with a moderate amount of extraluminal contrast surrounding the right kidney | Treated conservatively |
| 7 | Porfyris et al., 2016 [17] | 75/M | Right flank pain and three episodes of vomiting | N/A | 5 mm | Right ureterovesical junction | Right hydroureteronephrosis, contrast extravasation, and retroperitoneum fluid collection | Antibiotics, ultrasound-guided nephrostomy tube insertion. |
| 8 | Pampana et al., 2013 [18] | 69/F | Right-sided flank pain that started 6 hours before, nausea | History of renal calculi in the younger age | Not specified | Right kidney | Contrast medium extravasation | D-J ureteral stent placement |
| 9 | Kheiri et al., 2018 [19] | 52/F | Right lower abdominal pain for 1 day | History of UTI | 7 mm | Right ureterovesical junction | Hydroureteronephrosis and ruptured calyx | D-J ureteral stent placement and lithotripsy |
| 10 | Taşkınlar et al., 2016 [20] | 1.5/F | Fever, vomiting, and abdominal pain | Retroperitoneal tumor pushing left kidney, UTI | 10 mm | Left kidney | Left perirenal urinoma and an extruded calculus in the urinoma, contrast extravasation. | D-J ureteral stent placement |
| 11 | Tas et al., 2013 [21] | 55/F | Acute flank pain for the last 6 days | History of right distal uretral stone | 6 mm | Right distal ureter | Rupture of right renal pelvis in two points, peripheral fluid accumulation, contrast extravasation | Ureteroscopic lithotripsy, D-J stent, and drain placement |
| 12 | Assaker et al., 2020 [10] | 53/M | Right back pain 4 hours prior to presentation, nausea, vomiting, no fever | Benign prostatic hyperplasia and chronic right hydrocele | 4 mm | Right ureterovesical junction | Fluid extravasation around the proximal ureter and at the perinephric renal space | D-J ureteral stent placement |
| 13 | Reva et al., 2013 [22] | 29/M | Left flank pain, nausea, and macroscopic hematuria | Klinefelter syndrome | 4 mm | Left ureterovesical junction | Contrast extravasation | D-J ureteral stent placement |
| 14 | Díaz et l., 2011 [23] | 46/M | Left flank pain | N/A | 7 mm | Left ureterovesical junction | Contrast extravasation at the level of the left renal pelvis | Double pigtail catheter for a two-week period |
| 15 | Prem et al., 2021 [24] | 30/F | Right-sided abdominal pain, and fever for a month. | Right urolithiasis and pyelonephritis treatment over 3 years. | Multiple with variable sizes | Right pelvis, upper ureter, and multiple calculi in right lower ureter | Ruptured right kidney, hydronephrosis, multiple renal and ureteric calculi, Urinoma formation in subcapsular region of liver, pneumoperitoneum | Exploratory laparotomy and right nephroureterectomy |
| 16 | Cruz et al., 2021 [8] | 36/F | Left flank pain since 2 days prior, nausea and vomiting, no fever | Previous nephrolithiasis history | 7 mm (proximal one) and 3 mm (distal one). | Proximal left ureter and another one distally | Left-sided hydronephrosis, multiple ureteral stones, trace left perinephric fluid. | Conservative treatment with alpha-blockers, analgesics, and antiemetics |
| 17 | Koktener et al., 2007 [6] | 63/M | Right-sided flank pain | History of T-cell lymphoma, and right-sided nephrolithiasis, chemotherapy | <5 mm | 3 cm caudal to the iliac bifurcation at right ureter | Contrast extravasation, a large amount of fluid around the right kidney, liver, pararenal, and paracolic region | D-J ureteral stent placement |
| 18 | Our case | 24/F | Right-sided flank pain | N/A | 3 mm | Right ureter about 1.5 cm away from vesicoureteric junction | Enlarged and edematous right-sided kidney with moderate hydroureteronephrosis. In addition to the presence of a tiny distal ureteric stone measuring 3 mm located about 1.5 cm away from vesicoureteric junction | D-J ureteral stent placement |
| # . | Author, year . | Age/gender . | Clinical presentation . | Risk factors . | Stone size . | Stone site . | CT findings . | Management . |
|---|---|---|---|---|---|---|---|---|
| 1 | Yin et al., 2022 [7] | 46/M | Left lower back pain, oliguria, no fever | A long history of renal stones, multiple ESWL treatments | Not specified | Left kidney | Perirenal hematoma, non-specific renal rupture | Nephrectomy due to renal parenchymal rupture |
| 2 | Khashan et al., 2023 [9] | 19/F | Acute right-sided lower abdominal pain, nausea, vomiting, chills, and no fever | N/A | 3 mm | Right ureterovesical junction | Mild to moderate right hydroureteronephrosis, perinephric edema | Conservative: IV fluids, ketorolac, ceftriaxone, tamsulosin, close monitoring, and passed stone spontaneously |
| 3 | Liao et al., 2021 [13] | 63/F | Acute flank pain, mild right flank tenderness | History of similar symptoms 1 month before | Largest: 1.9 × 1.0 cm | Right renal pelvis | Hydronephrosis, multiple calculi, renal calyceal rupture with extravasation | D-J ureteral stent placement |
| 4 | Yanaral et al., 2017 [14] | 86/F | Left flank pain for 7 days, nausea, vomiting | left kidney stone a month ago | 8 mm | Left renal pelvis | Hydronephrosis, contrast extravasation, and perirenal fluid | D-J ureteral stent placement and shock wave lithotripsy |
| 5 | Okpii et al., 2022 [15] | 77/M | Worsening left-sided abdominal pain 3 days prior to presentation | Suprapubic catheter due to multiple urethral strictures post-prostatectomy procedure | 12 mm | Left vesico-ureteric junction | Intra-abdominal free fluid on the left side, rupture of the left renal calyces with contrast extravasation | Nephrostomy due to multiple complex urethral strictures, laser stone fragmentation |
| 6 | Weber et al., 2022 [16] | 33/M | Cough, vomiting, flank pain, and inability to urinate | Recurrent ureteral stones | Not specified | Right kidney | A column of contrast in the right renal pelvis and ureter with a moderate amount of extraluminal contrast surrounding the right kidney | Treated conservatively |
| 7 | Porfyris et al., 2016 [17] | 75/M | Right flank pain and three episodes of vomiting | N/A | 5 mm | Right ureterovesical junction | Right hydroureteronephrosis, contrast extravasation, and retroperitoneum fluid collection | Antibiotics, ultrasound-guided nephrostomy tube insertion. |
| 8 | Pampana et al., 2013 [18] | 69/F | Right-sided flank pain that started 6 hours before, nausea | History of renal calculi in the younger age | Not specified | Right kidney | Contrast medium extravasation | D-J ureteral stent placement |
| 9 | Kheiri et al., 2018 [19] | 52/F | Right lower abdominal pain for 1 day | History of UTI | 7 mm | Right ureterovesical junction | Hydroureteronephrosis and ruptured calyx | D-J ureteral stent placement and lithotripsy |
| 10 | Taşkınlar et al., 2016 [20] | 1.5/F | Fever, vomiting, and abdominal pain | Retroperitoneal tumor pushing left kidney, UTI | 10 mm | Left kidney | Left perirenal urinoma and an extruded calculus in the urinoma, contrast extravasation. | D-J ureteral stent placement |
| 11 | Tas et al., 2013 [21] | 55/F | Acute flank pain for the last 6 days | History of right distal uretral stone | 6 mm | Right distal ureter | Rupture of right renal pelvis in two points, peripheral fluid accumulation, contrast extravasation | Ureteroscopic lithotripsy, D-J stent, and drain placement |
| 12 | Assaker et al., 2020 [10] | 53/M | Right back pain 4 hours prior to presentation, nausea, vomiting, no fever | Benign prostatic hyperplasia and chronic right hydrocele | 4 mm | Right ureterovesical junction | Fluid extravasation around the proximal ureter and at the perinephric renal space | D-J ureteral stent placement |
| 13 | Reva et al., 2013 [22] | 29/M | Left flank pain, nausea, and macroscopic hematuria | Klinefelter syndrome | 4 mm | Left ureterovesical junction | Contrast extravasation | D-J ureteral stent placement |
| 14 | Díaz et l., 2011 [23] | 46/M | Left flank pain | N/A | 7 mm | Left ureterovesical junction | Contrast extravasation at the level of the left renal pelvis | Double pigtail catheter for a two-week period |
| 15 | Prem et al., 2021 [24] | 30/F | Right-sided abdominal pain, and fever for a month. | Right urolithiasis and pyelonephritis treatment over 3 years. | Multiple with variable sizes | Right pelvis, upper ureter, and multiple calculi in right lower ureter | Ruptured right kidney, hydronephrosis, multiple renal and ureteric calculi, Urinoma formation in subcapsular region of liver, pneumoperitoneum | Exploratory laparotomy and right nephroureterectomy |
| 16 | Cruz et al., 2021 [8] | 36/F | Left flank pain since 2 days prior, nausea and vomiting, no fever | Previous nephrolithiasis history | 7 mm (proximal one) and 3 mm (distal one). | Proximal left ureter and another one distally | Left-sided hydronephrosis, multiple ureteral stones, trace left perinephric fluid. | Conservative treatment with alpha-blockers, analgesics, and antiemetics |
| 17 | Koktener et al., 2007 [6] | 63/M | Right-sided flank pain | History of T-cell lymphoma, and right-sided nephrolithiasis, chemotherapy | <5 mm | 3 cm caudal to the iliac bifurcation at right ureter | Contrast extravasation, a large amount of fluid around the right kidney, liver, pararenal, and paracolic region | D-J ureteral stent placement |
| 18 | Our case | 24/F | Right-sided flank pain | N/A | 3 mm | Right ureter about 1.5 cm away from vesicoureteric junction | Enlarged and edematous right-sided kidney with moderate hydroureteronephrosis. In addition to the presence of a tiny distal ureteric stone measuring 3 mm located about 1.5 cm away from vesicoureteric junction | D-J ureteral stent placement |
| # . | Author, year . | Age/gender . | Clinical presentation . | Risk factors . | Stone size . | Stone site . | CT findings . | Management . |
|---|---|---|---|---|---|---|---|---|
| 1 | Yin et al., 2022 [7] | 46/M | Left lower back pain, oliguria, no fever | A long history of renal stones, multiple ESWL treatments | Not specified | Left kidney | Perirenal hematoma, non-specific renal rupture | Nephrectomy due to renal parenchymal rupture |
| 2 | Khashan et al., 2023 [9] | 19/F | Acute right-sided lower abdominal pain, nausea, vomiting, chills, and no fever | N/A | 3 mm | Right ureterovesical junction | Mild to moderate right hydroureteronephrosis, perinephric edema | Conservative: IV fluids, ketorolac, ceftriaxone, tamsulosin, close monitoring, and passed stone spontaneously |
| 3 | Liao et al., 2021 [13] | 63/F | Acute flank pain, mild right flank tenderness | History of similar symptoms 1 month before | Largest: 1.9 × 1.0 cm | Right renal pelvis | Hydronephrosis, multiple calculi, renal calyceal rupture with extravasation | D-J ureteral stent placement |
| 4 | Yanaral et al., 2017 [14] | 86/F | Left flank pain for 7 days, nausea, vomiting | left kidney stone a month ago | 8 mm | Left renal pelvis | Hydronephrosis, contrast extravasation, and perirenal fluid | D-J ureteral stent placement and shock wave lithotripsy |
| 5 | Okpii et al., 2022 [15] | 77/M | Worsening left-sided abdominal pain 3 days prior to presentation | Suprapubic catheter due to multiple urethral strictures post-prostatectomy procedure | 12 mm | Left vesico-ureteric junction | Intra-abdominal free fluid on the left side, rupture of the left renal calyces with contrast extravasation | Nephrostomy due to multiple complex urethral strictures, laser stone fragmentation |
| 6 | Weber et al., 2022 [16] | 33/M | Cough, vomiting, flank pain, and inability to urinate | Recurrent ureteral stones | Not specified | Right kidney | A column of contrast in the right renal pelvis and ureter with a moderate amount of extraluminal contrast surrounding the right kidney | Treated conservatively |
| 7 | Porfyris et al., 2016 [17] | 75/M | Right flank pain and three episodes of vomiting | N/A | 5 mm | Right ureterovesical junction | Right hydroureteronephrosis, contrast extravasation, and retroperitoneum fluid collection | Antibiotics, ultrasound-guided nephrostomy tube insertion. |
| 8 | Pampana et al., 2013 [18] | 69/F | Right-sided flank pain that started 6 hours before, nausea | History of renal calculi in the younger age | Not specified | Right kidney | Contrast medium extravasation | D-J ureteral stent placement |
| 9 | Kheiri et al., 2018 [19] | 52/F | Right lower abdominal pain for 1 day | History of UTI | 7 mm | Right ureterovesical junction | Hydroureteronephrosis and ruptured calyx | D-J ureteral stent placement and lithotripsy |
| 10 | Taşkınlar et al., 2016 [20] | 1.5/F | Fever, vomiting, and abdominal pain | Retroperitoneal tumor pushing left kidney, UTI | 10 mm | Left kidney | Left perirenal urinoma and an extruded calculus in the urinoma, contrast extravasation. | D-J ureteral stent placement |
| 11 | Tas et al., 2013 [21] | 55/F | Acute flank pain for the last 6 days | History of right distal uretral stone | 6 mm | Right distal ureter | Rupture of right renal pelvis in two points, peripheral fluid accumulation, contrast extravasation | Ureteroscopic lithotripsy, D-J stent, and drain placement |
| 12 | Assaker et al., 2020 [10] | 53/M | Right back pain 4 hours prior to presentation, nausea, vomiting, no fever | Benign prostatic hyperplasia and chronic right hydrocele | 4 mm | Right ureterovesical junction | Fluid extravasation around the proximal ureter and at the perinephric renal space | D-J ureteral stent placement |
| 13 | Reva et al., 2013 [22] | 29/M | Left flank pain, nausea, and macroscopic hematuria | Klinefelter syndrome | 4 mm | Left ureterovesical junction | Contrast extravasation | D-J ureteral stent placement |
| 14 | Díaz et l., 2011 [23] | 46/M | Left flank pain | N/A | 7 mm | Left ureterovesical junction | Contrast extravasation at the level of the left renal pelvis | Double pigtail catheter for a two-week period |
| 15 | Prem et al., 2021 [24] | 30/F | Right-sided abdominal pain, and fever for a month. | Right urolithiasis and pyelonephritis treatment over 3 years. | Multiple with variable sizes | Right pelvis, upper ureter, and multiple calculi in right lower ureter | Ruptured right kidney, hydronephrosis, multiple renal and ureteric calculi, Urinoma formation in subcapsular region of liver, pneumoperitoneum | Exploratory laparotomy and right nephroureterectomy |
| 16 | Cruz et al., 2021 [8] | 36/F | Left flank pain since 2 days prior, nausea and vomiting, no fever | Previous nephrolithiasis history | 7 mm (proximal one) and 3 mm (distal one). | Proximal left ureter and another one distally | Left-sided hydronephrosis, multiple ureteral stones, trace left perinephric fluid. | Conservative treatment with alpha-blockers, analgesics, and antiemetics |
| 17 | Koktener et al., 2007 [6] | 63/M | Right-sided flank pain | History of T-cell lymphoma, and right-sided nephrolithiasis, chemotherapy | <5 mm | 3 cm caudal to the iliac bifurcation at right ureter | Contrast extravasation, a large amount of fluid around the right kidney, liver, pararenal, and paracolic region | D-J ureteral stent placement |
| 18 | Our case | 24/F | Right-sided flank pain | N/A | 3 mm | Right ureter about 1.5 cm away from vesicoureteric junction | Enlarged and edematous right-sided kidney with moderate hydroureteronephrosis. In addition to the presence of a tiny distal ureteric stone measuring 3 mm located about 1.5 cm away from vesicoureteric junction | D-J ureteral stent placement |
The optimal management of calyceal rupture remains debated, with treatment options ranging from conservative therapy to surgical intervention [10]. In Al-Mujalhem et al.'s study, 57.5% of cases were managed conservatively, while 35% required D-J stent placement [11]. Akpinar et al. reported successful conservative management in three out of four patients, with one case requiring D-J stenting. However, Chen et al. managed 72.2% of cases with D-J stents and 27.8% conservatively, all with favorable outcomes [5]. Stavridis et al. highlighted the effectiveness of D-J stent insertion [12], with occasional use of percutaneous drainage for infected urinomas [25]. In our case, ureteroscopy and D-J stent placement were performed, followed by conservative management, resulting in excellent clinical improvement. This approach highlights the importance of individualized treatment strategies based on the severity of the condition and the underlying cause.
Conflict of interest statement
None declared.
Funding
None declared.
Consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.



