-
PDF
- Split View
-
Views
-
Cite
Cite
Robert K Ewusi-Wilson, Alfred Osafo-Kwaako, Mawutor Dzogbefia, Majeste Koaume, Sensorineural hearing loss and retinopathy in sickle cell patients, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf177, https://doi.org/10.1093/jscr/rjaf177
Close - Share Icon Share
Abstract
Two male patients who have sickle cell disease present to the eye clinic with proliferative retinopathy as well as severe profound sensorineural hearing loss in both ears.
Introduction
Sickle cell disease (SCD) is a disorder which affects multiple systems involving red blood cells containing abnormal haemoglobin S [1, 2]. The disease has complications that manifests as chronic haemolytic anaemia and vaso-occlusive crises that cause severe pain as well as long-term and widespread organ damage [3, 4]. The vascular events result in hypoxia, ischemia, and infarction of the involved tissue in the eye and other organs of the body such as the auditory system. Severe systemic manifestations occur in sickle cell (SC) disease and severe ocular manifestations occur in haemoglobin SC and S-Thal [2, 5, 6]. Sickle cell retinopathy (SCR) is classified into proliferative sickle cell retinopathy (PSR) and non-proliferative sickle cell retinopathy (NPSR) [7, 8]. PSR is the major cause of vision loss in which peripheral neovascularization can lead to vitreous haemorrhage and/or retinal detachment [8, 9]. NPSR changes include salmon patches, iridescent spots, and black sunbursts [10]. The cochlear is at risk of vascular insults because of its microvasculature. Vaso-occlusion has been associated sensorineural hearing loss with endothelial dysfunction playing a major role [11].
There is dearth of information on the correlation between sensorineural hearing loss and PSR among Ghanaian SC patients.
We report on two cases of PSR and bilateral sensorineural hearing loss in two SC patients as a precursor to a cross-sectional study on the correlation between sensorineural hearing loss and PSR among Ghanaian SC patients.
Case report 1
A 50-year-old male of African descent reported to the eye clinic for the first time with complaints of not seeing clearly in the left eye since 2022 and it has been intermittent. Patient also complained of difficulty with hearing in both ears which was worse in the right ear since December 2021.
Patient’s medical history was remarkable for SCD (HbSC) and did not have comorbidities like hypertension and diabetes as well as no trauma to the eyes. Patient also said he had never been on admission at any hospital or ever been transfused with blood before.
Ear assessment by the otolaryngologist revealed intact tympanic membranes bilaterally on otoscopy. Pure-tone audiometry showed severe to profound sensorineural hearing loss across all tested frequencies from 250 to 8000 Hz and tympanometry revealed normal middle ear functioning in both ears.
The patient’s corrected visual acuity were 6/5 in the right eye and hand movement in the left eye which did not improve with pin hole.
On ophthalmic examination with slitlamp biomicroscope the patient had bilateral temporal iris atrophy with the pupillary margin in the right eye having a torn iris sphincter and mid dilated as well (Fig. 1). The lens in both eyes were clear using Lens Opacities Classification System III (LOCS III) and as well as the vitreous in the right eye. In the right eye fundus, there were drusens at the macular and in the peripheral retina there were black sunbursts lesions (Fig. 2a and b). There was vitreous haemorrhage and no retinal detachment in the left eye, and this obscured the view of the fundus (Fig. 3).
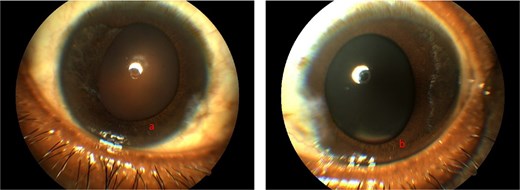
Showing anterior segment photography of right eye (a) and left eye (b) respectively with iris atrophy temporally and torn iris sphincters.
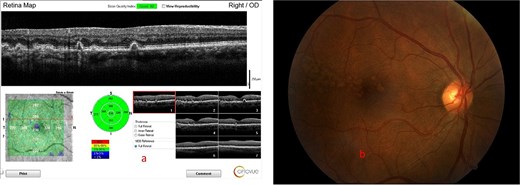
Showing the optical coherence tomography (OCT) scan of the macular with large drusens (a) and fundus photograph of the macular with large drusens at the macular (b) in the right eye.

Showing ocular ultrasound of vitreous hemorrhage in the left eye.
Case report 2
A 44-year-old male of African descent reported to the eye clinic with complaints of not seeing in the left eye which started in 2017 with something floating in his vision. Patient also complained of difficulty hearing after a week the eye problem had started.
Patient’s medical history was remarkable for SCD (HbSC) and did not have comorbidities like hypertension and diabetes as well as no trauma to the eyes. Patient also said he had never been on admission at any hospital or ever been transfused with blood before.
Ear assessment by the otolaryngologist revealed intact tympanic membranes bilaterally on otoscopy. Pure-tone audiometry showed moderate falling steadily through severe to profound sensorineural hearing loss across all tested frequencies from 250 to 8000 Hz in the right ear and severe sensorineural hearing loss across all tested frequencies from 250 to 8000 Hz in the left eye. Tympanometry revealed normal middle ear functioning in both ears.
The patient’s corrected visual acuity were 6/12−3 in the right eye and no perception of light in the left eye.
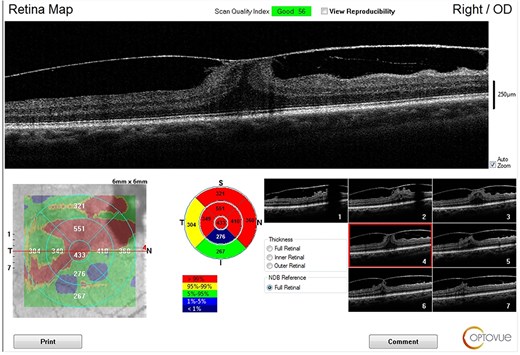
On ophthalmic examination with slitlamp biomicroscope the patient had iris atrophy with torn iris sphincter nasally in the right eye and mid dilated as well. The lens in the right eye was clear using LOCS III grading (Fig. 4a). The left eye had a complicated cataract, and this obscured the view of the fundus (Fig. 4b). There were vitreous tractions at the macular (Fig. 5) and black sunbursts lesions in the peripheral retina in the right eye during funduscopy.
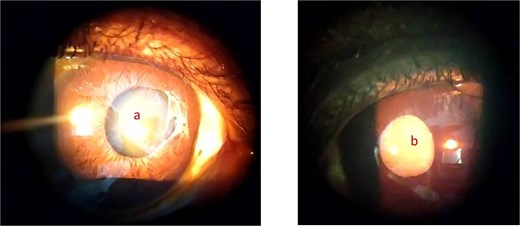
Showing anterior segment photograph of the right eye with iris atrophy (a) and complicated cataract in the left eye (b).
Discussion
Vitreous hemorrhage is a sight threatening complication of SCD [12]. During vaso-occlusive crisis in SCD, ischemia stimulates angiogenesis which leads to neovascularization, pre-retinal or vitreous hemorrhage and tractional retinal detachment in the eye whiles in the ear it leads to ischemia of the cochlear resulting in sensorineural hearing loss. However, ischemia of cochlear is reversible upon early detection and intervention to prevent permanent hearing loss [13, 14]. Although vitreous hemorrhage and sensorineural hearing loss in SCD are associated with vaso-occlusive crises, which lead to ischemic events in the eye and ear, our patients had no previous crises. Most patients experience floaters or a sudden loss of vision usually unilaterally.
There was anterior segment ischemia in the eyes in addition to intact tympanic membranes and normal middle ear function bilaterally, along with profound sensorineural hearing loss.
The present cases highlight the diagnostic difficulty of vitreous hemorrhage. The presence or complain of floaters by patients should raise a suspicion of a possible early vitreous hemorrhage which should warrant a dilated funduscopy with an indirect ophthalmoscope and a slitlamp biomicroscope. Other imaging modalities such as ocular ultrasound sonography and optical coherence tomography can be employed.
The first patient presented with a vitreous haemorrhage which is usually as a result of a previous vaso-occlusive crisis which leads to neovascularization as a result of ischemia stimulating angiogenesis. These weak new blood vessels caused the vitreous haemorrhage [15].
The second patient who presented with a complicated cataract likely had developed a vitreous haemorrhage in the past which could have induced fibrovascular proliferation which led to scarring and subsequently tractional retinal detachment [16]. Longstanding retinal detachments can lead to complicated cataract [17]. Visual loss in PSR occurs most commonly due to vitreous haemorrhage and tractional retinal detachment [18].
The patients also presented with black sunbursts in their right eyes which are as a result of migration and proliferation of retinal pigment epithelium which likely occurred in response to haemorrhage [19].
HbSC patients usually deny having SCD because they have less history of hospitalization unlike those with HbSS, thereby complicating the management [10].
Conclusion
Accurate diagnosis and management of patients with vitreous haemorrhage can be challenging in resource-limited settings, however, SC patients with complaints of floaters should report to the eye clinic as early as possible. Additionally, such patients will need a dilated funduscopy to rule out vitreous haemorrhage as well as get peripheral retinal laser photocoagulation done in both eyes if the media in the eye with the vitreous haemorrhage is still clear.
Patients with SCD who present with sensorineural hearing loss should be encouraged to have their eyes examined before they possibly develop a vitreous haemorrhage or if they develop a vitreous haemorrhage first, then their ears as well as other organs should be examined for any complication resulting from the vaso-occlusive crisis. SC patients will need routine check-ups to examine and manage them for other conditions.
There is a need for a joint cross-sectional study of patients with SC by ophthalmology and otology researchers to identify any possible correlation between sensorineural hearing loss and PSR in SC patients. This will identify early signs that can prompt the early institution of treatment to prevent damage of other end organs.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
None declared.



