-
PDF
- Split View
-
Views
-
Cite
Cite
Kaleab H Gebreselassie, Rakeb T Mamo, Yitayew E Mohammed, Tessema B Welderufael, Kalkidan K Mekoya, Transurethral migration of vesical gossypiboma following open prostatectomy: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf170, https://doi.org/10.1093/jscr/rjaf170
Close - Share Icon Share
Abstract
Gossypiboma refers to a retained surgical sponge within the body after a surgical procedure. It is commonly reported in the abdominal cavity and is rare in the urinary bladder (vesical gossypiboma). There are only a few reports of vesical gossypiboma in the literature, and patients often present long after the initial surgery. Features of recurrent urinary tract infections (UTIs) are common symptoms of vesical gossypiboma, but transurethral migration is a rare manifestation. We present a case of vesical gossypiboma with transurethral migration in a 64-year-old patient who underwent an open trans-vesical prostatectomy 3 months before visiting our hospital. He was repeatedly treated for recurrent UTIs until the diagnosis of vesical gossypiboma was finally confirmed using cystourethroscopy. We successfully removed the retained gauze via open bladder exploration. Gossypiboma can easily be overlooked, and we urge urologists to maintain a high index of suspicion to diagnose similar cases promptly.
Introduction
Gossypiboma is a retained surgical sponge (RSS) in the body after surgical procedure. The incidence of gossypiboma is under-reported, probably due to the medico-legal issues and misdiagnosis. Although intraabdominal gossypiboma is the most common type, the condition has been reported to occur in 1/100–3000 patients across all surgical disciplines [1, 2]. There have been few reports of gossypiboma of urinary bladder in the medical literature and even fewer regarding migration through the urethra [1–3].
Patients with vesical gossypiboma can manifest with both acute and chronic urinary symptoms, the most common ones being recurrent urinary tract infections (UTIs) and lower urinary tract symptoms (LUTS), such as dysuria, urgency, and urinary frequency. Rarely, transurethral migration of vesical gossypiboma with or without hematuria can also present [4, 5].
Vesical gossypiboma usually poses a diagnostic challenge to the clinician with significant patient morbidity, probably due to its delayed non-specific presentation and inconclusive imaging findings. The treatment of vesical gossypiboma has to be individualized depending on the size of the gauze and its nature, adhesion, as well as age of the patient [3, 6]. Herein, we reported transurethral migration of vesical gossypiboma in a 64-year-old patient who underwent open prostatectomy 3 months before visiting our hospital.
Case report
A 64-year-old male patient was referred to our hospital with a history of severe LUTS and recurrent episodes of UTI. The patient was diagnosed with benign prostatic hyperplasia at a primary hospital in the past year and had undergone trans-vesical prostatectomy 3 months before visiting our hospital. He reported persistent and severe LUTS after the surgery and was repeatedly treated with oral antibiotics for recurrent UTIs. He also developed an acute urinary retention and a suprapubic catheter was placed at a local hospital. The physical examination revealed a physically fit adult with a suprapubic Foley catheter and healed surgical scar.
Complete blood count, renal function test, and urinalysis were within the normal limits and the urine culture revealed no growth. Abdominopelvic ultrasonography was unremarkable. Cystourethroscopy examination was performed with the impression of urethral or bladder neck stenosis, and showed a large whitish spongiform structure impacted within the urethral lumen (Fig. 1).
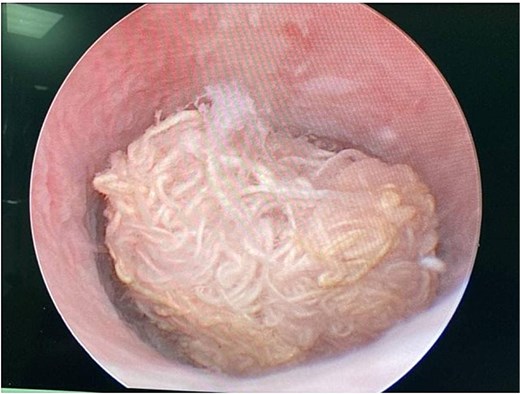
Cystourethroscopy showing a retained spongiform structure in the urethra.
A gentle attempt to remove the retained sponge using endoscopic forceps was failed. Antegrade cystoscopic evaluation under spinal anesthesia showed the same spongiform structure in the bladder with distal migration through the urethra. A gentle attempt to remove the sponge through the suprapubic access also failed, resulting in partial protrusion of the retained gauze through the suprapubic wound (Fig. 2A).
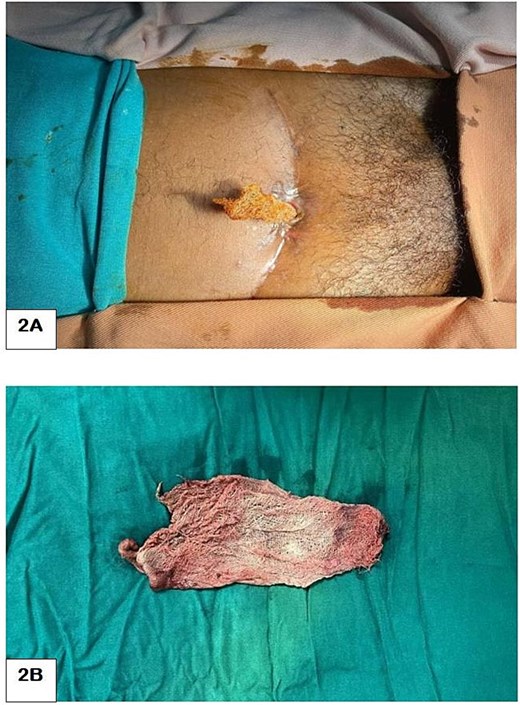
A piece of surgical gauze protruding through the suprapubic cystostomy site after trial of antegrade cystoscopic removal (A) and postoperative picture showing the removed surgical gauze (B).
The patient was then counseled for open surgical exploration of the urinary bladder under regional anesthesia. Up on surgical exploration, the RSS was adherent to the bladder mucosa and was removed successfully (Fig. 2B). Transurethral catheter was placed for a week and the patient was discharged home on the next day. The patient reported improvement of his symptoms after catheter removal and was passing urine normally during his follow-up visits.
Discussion
The term “Gossypiboma” is derived from a combination of Latin word “Gossypium” (cotton) and Swahili word “Boma” (place of concealment). Although it has been reported to occur in all surgical disciplines, the most common location is the abdominal cavity, followed by pelvis. Gossypiboma is rarely seen in clinical practice due to medico-legal issues and other reasons. It is estimated to occur in 1/1000–1500 for abdominal operation and 1/100–3000 cases for all surgical procedures [1, 2]. Vesical gossypiboma is relatively rare as very few isolated cases have been reported, and its migration through the urethra, is even rarer [2, 3, 6]. In our case, the patient had a retained vesical gauze with urethral migration causing urine retention.
Risk factors for gossypiboma include unplanned surgeries of longer duration, operations entailing more than one major procedure, emergency surgeries, more than one surgical team, high intraoperative blood loss, unexpected intraoperative factors, failure of material count or incorrect counts, and obesity [3, 4, 6]. Since our patient was operated at some other hospital, we couldn’t identify the possible risk factors.
Vesical gossypiboma can manifest at any time, ranging from the immediate to several decades after the procedure. The most common presentations include LUTS and recurrent UTI, as in the index case. They may mimic bladder stone, bladder mass, invasive adnexal mass, pelvic abscess, or fistulation [3, 5]. The detection of gossypiboma is clinically and radiologically challenging. An ultrasonography, plain abdominal radiography, CT (computed tomography) scan and MRI (Magnetic Resonant Imaging) are all useful in the diagnosis, but can also be inconclusive. Cystoscopy has a good diagnostic as well as therapeutic advantage, as it can give information regarding the nature of the retained foreign body. A high index of suspicion is very important to make a timely diagnosis [2, 4].
Once vesical gossypiboma is diagnosed, it should be removed. The methods of removal depend on the size and its fragility and the adhesion. Open bladder exploration is commonly performed for removal of the vesical gossypiboma, but endoscopic or percutaneous removal can also be performed in selected cases. In our case, open bladder exploration was done after failed trial of cystoscopic removal. Vesical gossypiboma is an avoidable condition and prevention is preferable solution; by thorough exploration of the surgical site and meticulous count of surgical materials at the end of every procedure [2, 3, 5].
Conclusion
Vesical gossypiboma should be considered as a differential diagnosis in patients with persistent or worsening of LUTS following open bladder or prostate surgery. Open surgical removal is an alternative option to endoscopy attempt of treatment. Gossypiboma is an avoidable condition, and prevention is preferable.
Conflict of interest statement
None declared.
Funding
None declared.



