-
PDF
- Split View
-
Views
-
Cite
Cite
Weibin Du, Fangbing Zhu, Yanfei Zhu, Chun He, A new attempt to treat Ellman III PASTA lesions: arthroscopic side-to-side anastomosis of longitudinal split tendon, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf108, https://doi.org/10.1093/jscr/rjaf108
Close - Share Icon Share
Abstract
To investigate the surgical method and therapeutic effect of longitudinal tendon splitting and side-to-side anastomosis on Ellman III partial articular supraspinatus tendon avulsion (PASTA) lesions under arthroscope. Thirty-two patients with Ellman III PASTA lesions were treated with the method. Joint range of motion, Visual Analogue Score (VAS), University of California at Los Angeles (UCLA), and American Shoulder and Elbow Surgeons (ASES) scores were recorded and compared before surgery and at the last follow-up, and postoperative pain and functional improvement were comprehensively evaluated. At the last postoperative follow-up, the patients had anterior flexion (168.69 ± 4.99) °, abduction (167.72 ± 4.88) °, external rotation (82.44 ± 3.20) °, and internal rotation (68.25 ± 4.04) °. At the last follow-up, VAS, UCLA, and ASES scores were improved, respectively. The technique of longitudinal tendon splitting and side-to-side anastomosis under arthroscopy has little damage to the normal tissue of bursa-sided supraspinatus muscle, which is an effective method for treating Ellman III PASTA lesions.
Introduction
At present, with the aging of the population and the popularity of sports, the incidence of rotator cuff injury shows an increasing trend, and the incidence of rotator cuff injury has been reported to be ~17%–37% [1, 2]. Partial tear of rotator cuff is divided into partial tear of articular-sided rotator cuff, tear internally and tear near the joint capsule according to different affected sites. Among them, partial tear of articular-sided rotator cuff is more common, which is two to three times as common as the tear near the joint capsule. It is often combined with other lesions, such as superior labrum anterior and posterior injury, biceps tendinopathy, osteoarthritis, and frozen shoulder, which are common causes of shoulder pain and mobility restriction in adults [3, 4]. Partial articular supraspinatus tendon avulsion (PASTA) lesions is a special type of rotator cuff injury, which is a partial tear of the articular-sided supraspinatus tendon. At present, relevant scholars have done a lot of research on the treatment of PASTA lesions, but no unified best treatment technique has been obtained [5–7].
The pathogenesis of partial tear of rotator cuff includes impact, instability, trauma, and tendon degeneration. Some studies suggest that the rotator cuff near the joint has a poor blood supply, and once partial tear occurs, the possibility of self-healing is less. After conservative treatment of PASTA injured patients, 53% of them had further tear, and 28% of them finally developed full-layer tear of the rotator cuff [8–11]. Current treatments for PASTA lesions include arthroscopic local debridement of edge, or acromioplasty, in situ repair of glenohumeral joint, repair through the tendon and conversion to full-layer repair. For PASTA injured patients with thickness of tear >50% of tendon, surgical repair may achieve better curative effect and avoid the progression of tear [7, 12].
Ellman III PASTA lesions is a partial tear on the articular side of the supraspinatus tendon to a depth >50% or 6 mm of the tendon thickness. For Ellman III PASTA lesions, both the repair through the tendon and the conversion to full-layer repair can obtain satisfactory curative effect. Although the rotator cuff tissue on the side of the bursae can be preserved and the repair of the rotator cuff footprint is more consistent with the anatomy, so as to achieve better bone-tendon healing, it is difficult to control the intraoperative anchor nail placement, threading and suture tension, and the technical requirements are high. The full-layer repair method is to transversely peel the rotator cuff tissue on the side of the residual bursae from the footprint of the rotator cuff. As the normal rotator cuff tissue is damaged greatly, it may be more suitable for patients with tear thickness of >80%–90% or patients with poor tendon quality on the side of the residual bursae. Different from the above methods, this study applied the idea of side-to-side anastomosis in the repair of giant U rotator cuff tear to the repair of Ellman III PASTA lesions. Guided by positioning needle, the tendon was split longitudinally along the direction of tendon fibers, and nailed fixation was completed through this channel. At the same time, external anchors were applied to strengthen the stitching effect. The technique preserves the attachment of rotator cuff tissue on the side of the bursae in the footprint area and has achieved good clinical effect.
Methods
Patients and data
Consent for publication was signed by our patients and approved by the Ethics Committee. In this study, 32 patients with Ellman III PASTA lesions in our hospital from July 2020 to July 2023, with an average age of 51.5 ± 6.7 years old, including 13 males and 19 females, were selected, all of whom underwent longitudinal tendon splitting and side-to-side anastomosis under arthroscopy.
Inclusion and exclusion criteria
Inclusion criteria: (i) no joint function restriction of shoulder before onset, (ii) diagnosed as Ellman III PASTA lesions by magnetic resonance imaging (MRI) and intraoperative arthroscopy, (iii) the time of pain and functional limitation ≥6 months, affecting life and work, (iv) conservative treatment for >3 months has no obvious effect, (5) stable vital signs, no obvious trauma, (vi) cooperate with surgical treatment, and (7) agree to sign informed consent.
Exclusion criteria: (i) severe vascular nerve injury and a fracture of shoulder, (ii) combined with shoulder joint diseases, such as rheumatoid arthritis, shoulder osteoarthritis, etc.,(iii) the anterior and posterior injuries of the upper glenoid labrum of the shoulder joint need to be repaired and fixed, (iv) anterior instability of shoulder joint, (v) previous history of shoulder surgery or brachial plexus injury.
Treatment methods
Surgical methods
In oblique lateral position after general anesthesia, the shoulder joint was routinely released, and the traction weight of the affected limb was 3–4 kg. After disinfection and towel, sterile marker pen marker approach location. Conventional posterior approach was used to investigate the injuries in glenohumeral joint and articular-sided rotator cuff. The extent and thickness of the articular-sided rotator cuff tear was evaluated by a conventional anterior approach to release the anterior space of rotator cuff, clean the denatured, worn and inactivated rotator cuff tissue, and thoroughly expose the normal rotator cuff tissue. If the articular-sided rotator cuff tear exceeds 50% of the rotator cuff tendon thickness, indwelling localization with an No.18 lumbar puncture needle is performed. Acromioplasty was performed for Blgliani II and III to clear the subacromial bursitis by posterior and lateral approaches. The posterior lateral channel was implanted with an arthroscopic lens, and the lateral channel was longitudinally split along the positioning needle on the surface of the tendon using a sharp knife blade according to the positioning needle of No.18 lumbar puncture needle to evaluate the extent of the tear of the articular-sided supraspinatus muscle and the cartilaginous junction of humerus head. After the bone bed was freshened, 1–2 4.5 mm linear anchors were inserted into the articular cartilage of the humerus head along the split longitudinal channel, and side-to-side anastomosis were performed after the suture. Depending on the closure of the tendon, 1–2 external anchors could be used for suture bridge fixation to close the split opening. The arthroscope was again placed inside the glenohumeral joint to evaluate the suture effect and examine the reconstruction of the rotator cuff footprint. Intraoperative operations are shown in Fig. 1.
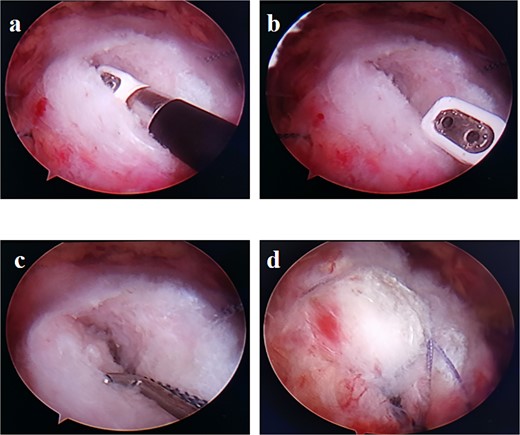
(a,b) Split the tendon lengthwise along the tendon fibers on the side of the bursae. (c) A side-to-side suture is performed after implantation of an inner row anchor. (d) The situation after the suture of the double-row anchors.
Postoperative management
Postoperative ice was applied to the affected shoulder to relieve swelling, gentle passive activities began on the first day after surgery, active functional exercise began 4 weeks after surgery, shoulder joint was fixed in mild external booth support for 4 weeks, and shoulder joint strength training began 12 weeks after surgery. The operative time was recorded, and Visual Analogue Score (VAS), University of California at Los Angeles (UCLA), and American Shoulder and Elbow Surgeons (ASES) scores before and at the last follow-up were compared, as well as the degree of shoulder range of motion, to comprehensively evaluate the degree of postoperative pain and functional improvement of patients.
Statistical analysis
All data were analysed with SPSS22.0, represented by mean ± standard deviation (|$\overline{x}$| ± s), and comparison of scores before and after treatment was conducted by paired sample t-test, P < 0.05 indicates a statistical difference.
Results
All 32 patients were followed up for 12–25 (16 ± 3.7) months. Radiography showed good rotator cuff healing and shoulder joint mobility. The range of motion of the affected shoulder joint improved significantly after surgery, and there was a statistical difference between the preoperative and the last follow-up (anterior flexion: 132.19 ± 7.42 vs. 168.69 ± 4.99, abduction: 113.63 ± 8.31 vs. 167.72 ± 4.88, external rotation: 58.03 ± 4.90 vs. 82.44 ± 3.20, internal rotation: 44.28 ± 3.79 vs. 68.25 ± 4.04, all P < 0.05, as shown in Table 1). VAS, UCLA, and ASES scores were significantly improved after surgery, and there was a statistical difference between before surgery and the last follow-up (VAS: 5.78 ± 1.04 vs. 1.09 ± 0.69, UCLA: 15.56 ± 3.83 vs. 32.09 ± 5.40, ASES: 48.25 ± 5.96 vs. 90.28 ± 3.31, all P < 0.05, see Table 1). There were no postoperative complications such as nerve injury, rotator cuff retear, infection, hematoma and fracture. Typical case is shown in Fig. 2. Consent for publication was signed by our patient and approved by the Ethics Committee.
Comparison of shoulder range of motion, VAS, UCLA, and ASES scores between the patients before and at the last follow-up
| Time . | Anterior flexion (°) . | Abduction (°) . | External rotation (°) . | Internal rotation (°) . | VAS (scores) . | UCLA (scores) . | ASES (scores) . |
|---|---|---|---|---|---|---|---|
| Preoperative | 132.19 ± 7.42 | 113.63 ± 8.31 | 58.03 ± 4.90 | 44.28 ± 3.79 | 5.78 ± 1.04 | 15.56 ± 3.83 | 48.25 ± 5.96 |
| Final follow-up | 168.69 ± 4.99 | 167.72 ± 4.88 | 82.44 ± 3.20 | 68.25 ± 4.04 | 1.09 ± 0.69 | 32.09 ± 5.40 | 90.28 ± 3.31 |
| t value | −29.013 | −29.267 | −40.757 | −34.280 | 33.982 | −29.864 | −49.718 |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Time . | Anterior flexion (°) . | Abduction (°) . | External rotation (°) . | Internal rotation (°) . | VAS (scores) . | UCLA (scores) . | ASES (scores) . |
|---|---|---|---|---|---|---|---|
| Preoperative | 132.19 ± 7.42 | 113.63 ± 8.31 | 58.03 ± 4.90 | 44.28 ± 3.79 | 5.78 ± 1.04 | 15.56 ± 3.83 | 48.25 ± 5.96 |
| Final follow-up | 168.69 ± 4.99 | 167.72 ± 4.88 | 82.44 ± 3.20 | 68.25 ± 4.04 | 1.09 ± 0.69 | 32.09 ± 5.40 | 90.28 ± 3.31 |
| t value | −29.013 | −29.267 | −40.757 | −34.280 | 33.982 | −29.864 | −49.718 |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
Data are presented as mean ± standard deviation. VAS: Visual Analogue Score, UCLA: University of California at Los Angeles, ASES: American Shoulder and Elbow Surgeons.
Comparison of shoulder range of motion, VAS, UCLA, and ASES scores between the patients before and at the last follow-up
| Time . | Anterior flexion (°) . | Abduction (°) . | External rotation (°) . | Internal rotation (°) . | VAS (scores) . | UCLA (scores) . | ASES (scores) . |
|---|---|---|---|---|---|---|---|
| Preoperative | 132.19 ± 7.42 | 113.63 ± 8.31 | 58.03 ± 4.90 | 44.28 ± 3.79 | 5.78 ± 1.04 | 15.56 ± 3.83 | 48.25 ± 5.96 |
| Final follow-up | 168.69 ± 4.99 | 167.72 ± 4.88 | 82.44 ± 3.20 | 68.25 ± 4.04 | 1.09 ± 0.69 | 32.09 ± 5.40 | 90.28 ± 3.31 |
| t value | −29.013 | −29.267 | −40.757 | −34.280 | 33.982 | −29.864 | −49.718 |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Time . | Anterior flexion (°) . | Abduction (°) . | External rotation (°) . | Internal rotation (°) . | VAS (scores) . | UCLA (scores) . | ASES (scores) . |
|---|---|---|---|---|---|---|---|
| Preoperative | 132.19 ± 7.42 | 113.63 ± 8.31 | 58.03 ± 4.90 | 44.28 ± 3.79 | 5.78 ± 1.04 | 15.56 ± 3.83 | 48.25 ± 5.96 |
| Final follow-up | 168.69 ± 4.99 | 167.72 ± 4.88 | 82.44 ± 3.20 | 68.25 ± 4.04 | 1.09 ± 0.69 | 32.09 ± 5.40 | 90.28 ± 3.31 |
| t value | −29.013 | −29.267 | −40.757 | −34.280 | 33.982 | −29.864 | −49.718 |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
Data are presented as mean ± standard deviation. VAS: Visual Analogue Score, UCLA: University of California at Los Angeles, ASES: American Shoulder and Elbow Surgeons.
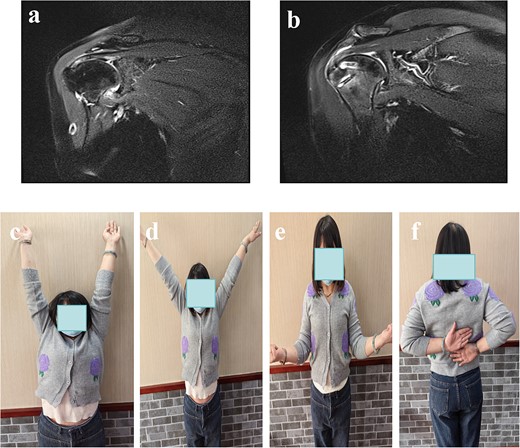
(a): Pre-operative MRI showed PASTA lesions. (b) The MRI showed good repair at 3 months postoperative follow-up. (c–f) The function of anterior flexion, abduction, external rotation and internal rotation 3 months postoperative follow-up.
Discussion
This study reports a new surgical procedure for Ellman III PASTA lesions. Different from traditional perforating tendon repair and conversion to full-layer repair, this technique uses a sharp blade to longitudinally split the tendon fibers on the bursae-sided of the supraspinatus tendon through the lateral channel to evaluate the extent of the tear of the articular-sided supraspinatus muscle and the cartilaginous junction of humerus head under direct vision. Both nail placement and suture can be performed through our open longitudinal channel. After the open channel is sutured,fixed and closed with 1–2 outrigger anchors after the side-to-side anastomosis, which is simple and reliable. Postoperative scores of VAS, UCLA, and ASES were significantly improved, and the shoulder range of motion was significantly improved, which were consistent with the results of Chen JJ et al. [13]. However, different from the surgical method reported by Chen JJ et al., our open channel is smaller, and the tear is closed by side-to-side anastomosis, supplemented by double-row suture bridge fixation, which increases the area of tendon-bone contact and has a better healing rate and a lower retear rate theoretically. Especially, when the inner and outer tear width of PASTA injured patients is >50% of the footprint area, the single row anchor repair technology cannot fully pressurize the outer part of PASTA injured patients. As a method to increase the tendon-bone contact area, the double-row anchor repair technique is recommended for rotator cuff repair, which can create a good environment for tendon healing and contribute to tendon-bone healing [14–18].
At present, the surgical repair of Ellman III PASTA lesions mainly includes perforating tendon repair and conversion to full-layer repair, both of which have certain advantages and disadvantages. The method of perforating tendon repair has great biomechanical advantages in maintaining the normal rotator cuff length and preserving the integrity of glenohumeral joint. Some studies have reported that perforating tendon repair can achieve satisfactory clinical results in the treatment of PASTA lesions [19–23]. However, a recent systematic review has shown that the perforating tendon repair method can lead to prolonged shoulder pain after surgery, with a high incidence of shoulder stiffness (18%), possibly due to longer operative time and interference with the glenohumeral cavity, as well as a mismatch in suture tension. In addition, the repair will inevitably cause a certain degree of damage to the complete tendon tissue of the lateral bursae, and the technology is relatively complex and the requirements are high for surgeon [24].
The PASTA lesions turned into a full-layer tear by tearing the rotator cuff tissue away from the footprint through a transverse split (the vertical direction of the tendon fibers) and then re-establishing the attachment of the rotator cuff. Previous studies have shown that this technique is clinically satisfactory, but to some extent, by converting supraspinatus tendon injury to full-layer tear, the bone and tendon are scarred rather than fibrochondral junction, which can easily lead to retearing. This technique only opens a channel along the direction of muscle fibers, which is different from transverse stripping of tendon attachment, and preserves as much as possible the bursae-sided tendon tissue. The rotator cuff was sutured to the footprint area through lateral sutures on both sides of the channel, and the open channel was effectively closed with less suture tension. This study results consistent with Huang P, etc [25]. There are also some considerations that need to be taken into account in the surgical procedures we studied: (i) It is necessary to evaluate the range and thickness of rotator cuff tear in the glenohumeral joint, and accurately locate the lumbar puncture needle. (ii) It is necessary to skillfully use a sharp blade in the subacromial space for longitudinal tendon splitting. (iii) It is necessary to implant inner row rivets in the cartilage margin as much as possible.
Of course, this study also has some limitations: (i) This study is a retrospective study with a small sample size and no control group was set for comparative study, which will be further improved in our future study. (ii) Long-term shoulder joint function score and range of motion evaluation were not performed in this study. (iii) It is unclear whether the rotator cuff healing rate has better results than other repair methods.
In conclusion, we applied the lateral suture technique of huge U-shaped rotator cuff tear to the repair process of Ellman III PASTA lesions, longitudinally split the tendon fibers of bursa-sided supraspinatus tendon and established a channel, which made nail insertion more convenient and reliable, suture simple and controllable, and easy to operate. Because of the longitudinal split, the normal tissue of the bursa-sided rotator cuff is less damaged during the operation. After the lateral suture and knot, the postoperative tension is less, the subjective feeling is better in the early postoperative stage and the rate of retear is lower, which is an effective method for the treatment of Ellman III PASTA lesions.
Author contributions
C.H. F.Z., Y.Z., and W.D. did the data collection and writing. C.H. and F.Z. were major contributors to writing the manuscript. Y.Z. and W.D. contributed to the conception and design of the study. All authors read and approved the final manuscript.
Conflict of interest statement
All the authors declare that they have no conflicts of interest.
Funding
This work is supported by Hangzhou Medical and Health Technology Planning Project (nos. 0020190358, 0020190844, B20200127, B20200203), Zhejiang Province Traditional Chinese Medicine Science and Technology Project (No. 2023ZR046), Hangzhou Agricultural and Social Development Research Guide Project (No. 20220919Y084), Hangzhou bio-medicine and health industry development support science and technology project (No. 2023WJC243, 2023WJC249), which supported us in data collection, analysis, and following up the patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The research programme complies with the guidelines of the Declaration of Helsinki. Approved by the Medical Ethics Committee of Jiangnan Hospital Affiliated to Zhejiang Chinese Medicine University (Hangzhou Xiaoshan Hospital of Traditional Chinese Medicine) (2019059). Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Written informed consent for publication of their therapeutic images was obtained from the patients. All subjects have given informed consent to publish identifying information/images in online open access publications. No minors were involved in the study.
References
Author notes
Weibin Du and Fangbing Zhu contributed equally to this paper.
- arthroscopy
- arthroscopes
- synovial bursa
- elbow region
- follow-up
- postoperative pain
- range of motion
- surgical procedures, operative
- sutures
- tendon
- shoulder region
- rotator cuff injuries
- supraspinatus muscle
- avulsion fracture
- splitting - mental defense mechanism
- anastomosis, side to side
- avulsed wound
- rotator cuff repair
- abduction
- supraspinatus tendon



