-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Hassani, Tarik Deflaoui, Anas Derkaoui, Yassir Akil, Mohammed Lakhloufi, Ahmed Vadel Jidou, Safae Ouahabi, Abdelali Guellil, Rachid Jabi, Mohammed Bouziane, Surgical management of giant retroperitoneal liposarcoma: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf056, https://doi.org/10.1093/jscr/rjaf056
Close - Share Icon Share
Abstract
Liposarcoma is a rare malignant tumor of mesenchymal origin. It accounts for ~7% of all mesenchymal sarcomas and 1% of cancers in general. Its incidence does not exceed 2.5 cases per million inhabitants per year. This tumor is generally locally invasive, often diagnosed at an advanced stage, and can grow to a considerable size and weight, culminating in a locally advanced form. We report a case of a 65-year-old patient with retroperitoneal liposarcoma treated by open surgical resection. The patient was admitted for the management of an abdomino-pelvic mass measuring 40 × 27 × 17 cm, progressively evolving over 5 years. The diagnosis was established by computed tomography scan. The postoperative course was uneventful, and after 1 year of chemotherapy, the patient died of respiratory distress.
Introduction
Liposarcomas (LPS) are malignant tumors resulting from the differentiation of adipocytes. They are among the most common subtypes of soft-tissue sarcomas (STS), accounting for ~15%–20% of all STS. This pathology is divided into four main subtypes: well-differentiated LPS (WDLPS, also known as atypical lipomatous tumors), dedifferentiated LPS (DDLPS), myxoid LPS (MLPS), and pleomorphic LPS [1].
It is locally invasive, usually diagnosed at a late stage, and can reach a significant size and weight, making it locally advanced.
What’s more, the recurrence rate is higher than for LPS in other locations [2].
Case presentation
A 65-year-old patient with a 15-years history of type 2 diabetes treated with insulin, presented with a progressively growing abdominopelvic mass over 5 years, worsening in the past 3 months with continuous right hypochondrium pain. No previous surgical history was reported Clinical examination revealed a stable patient with a distended abdomen, tenderness in the right hypochondrium, and a palpable large mass. Laboratory tests showed anemia (7.9 g/dl) and elevated C-reactive protein (250).
Preoperative staging, including computed tomography (CT) thorax, abdomen, and pelvis, showed no distant metastases. CT imaging (axial view, Fig. 1) identified a large retroperitoneal mass measuring 40 × 27 × 17 cm, involving the right kidney and its vasculature, displacing major structures like the inferior vena cava, duodenum, and pancreas. No magnetic resonance imaging (MRI) was performed.
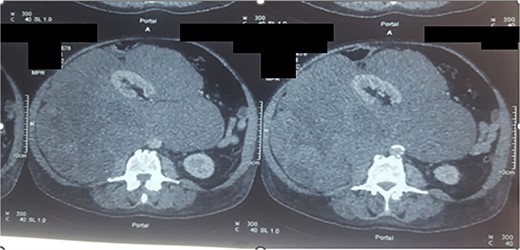
Axial section of CT scan, parenchymal window showing a large retroperitoneal mass measuring 40 × 27 × 17 cm (liposarcoma).
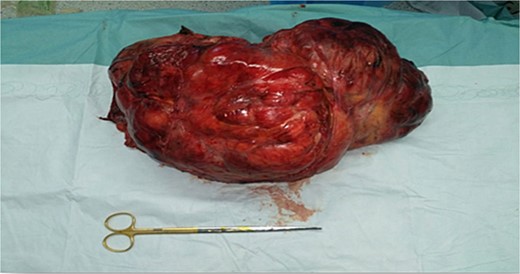
Preoperative preparation was completed, and with informed consent, open surgical resection involving the right kidney and abdominal drainage was performed (Fig. 2). The procedure lasted 6 hours and required blood transfusion (2 units). No intraoperative complications were reported. Intraoperative findings confirmed extensive adherence to surrounding tissues but no peritoneal carcinomatosis, ascites, or liver metastasis.
Histopathology (Fig. 3) reported a 40 × 27 × 17 cm encapsulated, high-grade (Grade III) dedifferentiated liposarcoma. No tumor proliferation was noted in the lymph nodes or adrenal gland. Postoperative recovery was uneventful, but the patient died after a year of chemotherapy due to respiratory distress.
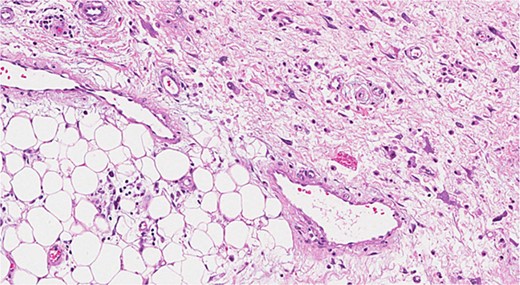
Dedifferentiated liposarcoma. This image shows a high-grade tumor.
Discussion
Sarcomas are rare primary tumors of mesenchymal origin, representing <1% of all cancers [2]. Between 10% and 15% of sarcomas are located in the retroperitoneum, where liposarcoma predominates, accounting for ~40%–50% of retroperitoneal sarcomas [3].
The progressive increase in tumour volume and the flexibility of the retroperitoneal space explain the long asymptomatic nature of the tumour [4].
In 80% of cases, clinical symptoms are mainly characterized by abdominal pain accompanied by a feeling of heaviness and abdominal mass [2].
It is important to remain vigilant during the workup of patients with large abdominopelvic masses, as rare coexistences or differential diagnoses may alter the treatment plan. Awareness of other possible diagnoses aside from sarcomas is essential to avoid mismanagement [5].
Abdominal CT and MRI are highly specific in suggesting the lipomatous nature of the lesion. Although poorly differentiated liposarcoma is easy to diagnose, using MRI, distinguishing between a lipoma and a well-differentiated liposarcoma is often a challenge due to the radiological similarities between these two types of lesion. However, there are certain radiological characteristics that can be used to differentiate them. Apart from the large size of the lesion, the presence of thick septa, nodular or globular lesions, nonfatty areas and a reduced proportion of adipose tissue in the lesion strongly suggest liposarcoma [6].
The patient’s progressively enlarging mass over five years, with worsening symptoms in the final three months, highlights the importance of early and thorough investigation of atypical symptoms. Prompt identification and intervention could prevent advanced disease and mitigate poor outcomes [7].
The definitive diagnosis is based on anatomopathological examination of the tumour resection specimen, which also classifies the tumour according to its histological variety [8].
Several histological varieties of liposarcoma, with increasing malignancy, have been described, including well-differentiated liposarcoma, myxoid liposarcoma, pleomorphic liposarcoma, round cell liposarcoma and dedifferentiated liposarcoma. In the case of our patient, histological examination concluded that the patient had a well-differentiated liposarcoma [9].
In our patient, histological examination showed a dedifferentiated liposarcoma.
Well-differentiated LPS have a better prognosis than other types of liposarcoma. Although they may recur locally after excision, their metastatic potential remains low. On the other hand, the myxoid form, which is the most malignant and most frequent (50% of cases), has a rapid recurrence rate and a poorer prognosis [1].
Prognostic factors include tumour grade, local recurrence and distant metastases. Other elements have also been associated with prognosis, such as complete resection, tumor volume, patient age, presence of synchronous metastases, retroperitoneal localization, and invasion of adjacent organs [10].
Surgical resection with negative margins is considered the first-line treatment for primary retroperitoneal LPS, as it improves local tumor control [11].
Retroperitoneal tumors are often large (median 30 cm) and can affect neighboring visceral organs as well as critical structures. Complete resection of the tumour is the standard of treatment, and when the tumour clearly invades adjacent organs or structures, resection of these areas is required. However, the ideal extent of resection remains a matter of debate, with some specialist sarcoma centers recommending removal of adjacent organs or structures even in the absence of clear signs of tumor invasion. Retrospective studies have shown that the extended or compartmental resection technique reduces locoregional recurrence rates and, in some cases, improves overall survival, particularly in the presence of low- or intermediate-grade tumors [12, 13].
Ultimately, the optimal extent of resection must take into account the histological subtype and strike a balance between the potential morbidity of surgery and the expected oncological results [11].
Conclusion
Retroperitoneal liposarcoma is a rare malignancy, often asymptomatic for long periods, leading to late diagnosis. Abdominal CT provides an accurate diagnosis. Surgical resection, with the widest possible margins, remains the only effective treatment.
Conflict of interest statement
None declared.
Funding
None declared.
References
Rives-Lange C, Poghosyan T, Dariane C, et al. .



