-
PDF
- Split View
-
Views
-
Cite
Cite
Raju Sah, Sushil B Rawal, Srijan Malla, Jyoti Rayamajhi, Pawan S Bhat, A left paraduodenal hernia causing bowel obstruction: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf045, https://doi.org/10.1093/jscr/rjaf045
Close - Share Icon Share
Abstract
Paraduodenal hernias (PDHs) are rare congenital internal hernias, constituting 50% of internal hernias and 0.2%–0.9% of small bowel obstructions. Left PDHs are more common and arise from midgut malrotation during embryonic development. We present the case of a 59-year-old male with acute small bowel obstruction caused by a left PDH. Imaging revealed clustered small bowel loops in the left upper quadrant, a hallmark of left PDH. Diagnostic laparoscopy confirmed the condition but was converted to open surgery due to dense adhesions. The herniated loops, initially edematous, were viable after reduction and warm compression. The hernia orifice was closed with non-absorbable sutures. Early diagnosis using imaging, particularly CT, is crucial, with findings such as clustered bowel loops, displaced structures, and engorged mesenteric vessels converging at the hernia orifice. Surgical intervention is the definitive treatment, highlighting the importance of prompt recognition to prevent complications and ensure favorable outcomes.
Introduction
Paraduodenal hernias (PDHs) are rare congenital internal hernias that account for approximately 50% of all internal hernias and 0.2%–0.9% of small bowel obstructions [1, 2]. Left PDHs, which comprise about 75% of these cases, result from abnormal midgut rotation and fixation during embryonic development, leading to small bowel loops herniating into a sac near the ligament of Treitz [2, 3].
The rarity and nonspecific clinical presentations of PDHs often make diagnosis challenging. They can mimic other causes of bowel obstruction, with symptoms ranging from intermittent abdominal pain to acute presentations in cases of strangulation or obstruction [4, 5]. Delayed diagnosis increases the risk of severe complications, including bowel ischemia, necrosis, and perforation, which can be life-threatening [4].
This report describes a 59-year-old male presenting with acute small bowel obstruction due to a left PDH, managed surgically with favorable outcomes. The case highlights the critical importance of timely diagnosis and appropriate surgical intervention in managing such rare presentations. Similar cases of left PDHs causing acute obstruction, managed successfully through surgery, have been reported by Patel et al. and Bhargav et al. [6, 7].
Case report
A 59-year-old male presented to the emergency department with a 3-day history of abdominal pain, vomiting, and inability to pass stool or flatus. His medical history included laparoscopic cholecystectomy nine years earlier and controlled hypertension managed with medication.
On examination, the patient was conscious and hemodynamically stable, with a pulse rate of 80/min, respiratory rate of 20/min, and blood pressure of 120/70 mmHg. Cardiovascular and respiratory examinations were unremarkable. Abdominal examination revealed distension, tenderness, and hyperactive bowel sounds. A laparoscopic cholecystectomy scar was noted, and hernial sites were intact.
An abdominal X-ray showed distended small bowel loops with multiple air-fluid levels (Fig. 1). A CT scan of the abdomen and pelvis revealed multiple distended jejunal loops (maximum diameter 5.6 cm) clustered in the left upper quadrant, with proximal and distal narrowing suggestive of a closed-loop obstruction, consistent with a paraduodenal hernia (Fig. 2).
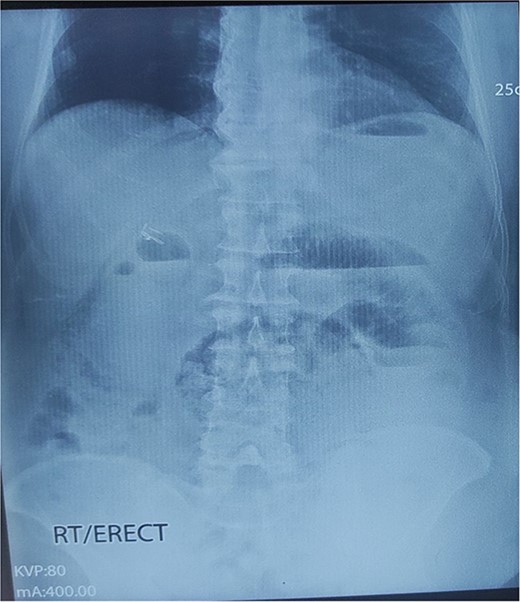
X-ray abdomen erect showing dilated small bowel loop with multiple air-fluid levels.
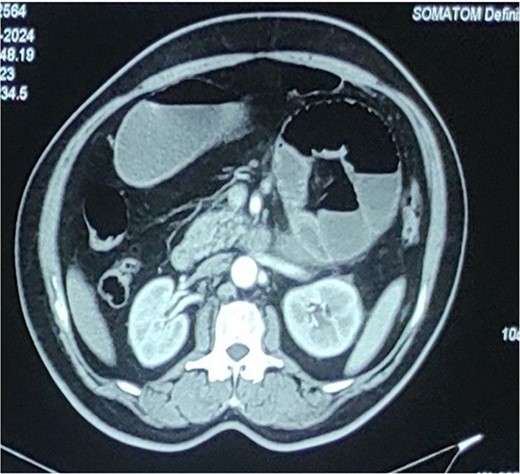
Computed tomography abdomen and pelvis showing distended multiple jejunal loops bunched together in the left upper quadrant with narrowing of both proximal and distal ends suggestive of closed loop obstruction (? Paraduodenal hernia).
Diagnostic laparoscopy confirmed a left paraduodenal hernia with entrapped bowel loops. Due to dense adhesions, the procedure was converted to open surgery. Enterolysis was performed to free the bowel loops, which were edematous, inflamed, and dusky. Warm compressions were applied for 10–15 min, gradually restoring the loops to a healthy pink color with active peristalsis, confirming their viability. The hernia orifice was securely closed with non-absorbable sutures to prevent recurrence (Fig. 3).
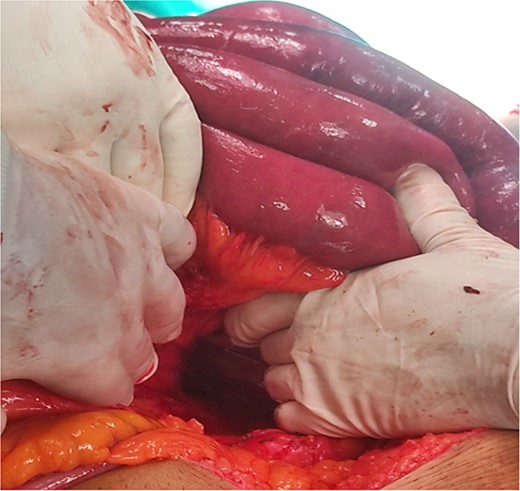
Intraoperative image showing reduced herniated jejunal loops and hernial defect.
Postoperatively, the patient recovered uneventfully. The patient was closely monitored for potential complications, such as bowel ischemia, perforation, or recurrence of obstruction, and was discharged on the seventh postoperative day and remained asymptomatic during follow-up.
Discussion
Internal hernias are rare, accounting for <1% of all abdominal hernias and representing an uncommon cause of bowel obstruction. Among these, PDHs are the most frequent, comprising 30%–53% of cases [1, 2]. Their development is attributed to midgut malrotation during embryogenesis, where incomplete mesenteric fusion creates a hernia orifice [8, 9]. Left-sided PDHs arise from the fossa of Landzert near the ligament of Treitz, with the hernia sac lying lateral to the fourth part of the duodenum and posterior to the inferior mesenteric vein and ascending left colic artery. PDHs are more common in males, with a male-to-female ratio of 3:1, and are typically diagnosed in the third or fourth decade of life [10].
The clinical presentation of PDHs varies widely. Chronic cases may manifest as intermittent, crampy abdominal pain, often exacerbated by eating or positional changes, and are frequently misdiagnosed as irritable bowel syndrome or psychosomatic disorders [11]. Acute presentations, as in this case, involve severe abdominal pain, vomiting, and obstipation, necessitating urgent evaluation. Diagnosis depends significantly on imaging, particularly contrast-enhanced CT, which reveals findings such as clustered small bowel loops in the left upper quadrant near the ligament of Treitz, displacement of adjacent structures, and engorged mesenteric vessels forming a "whirl sign." However, spontaneous or positional reduction of the hernia can complicate preoperative diagnosis [12, 13].
Surgical intervention is the definitive treatment for PDHs. The primary objectives are to reduce herniated bowel loops, assess bowel viability, and close or widen the hernia defect to prevent recurrence. The choice of surgical approach depends on the patient’s condition, the surgeon’s expertise, and the hernia’s complexity. Open surgery, as performed in this case, provides superior visualization and is preferred in cases involving dense adhesions or ischemic bowel. Conversely, laparoscopic approaches are increasingly used for their benefits of reduced postoperative pain, shorter recovery times, and improved cosmetic outcomes, particularly in uncomplicated cases [14, 15].
In this case, the bowel viability was successfully restored through warm compressions, evidenced by the return of a healthy pink color and active peristalsis. Non-absorbable sutures were used to securely close the hernia defect, with care taken to avoid injury to critical structures, including the inferior mesenteric vein.
This case highlights the importance of early diagnosis and timely surgical intervention in achieving favorable outcomes in PDHs. Clinicians should maintain a high index of suspicion for PDHs in patients presenting with bowel obstruction, especially in the absence of prior abdominal surgery. Early use of contrast-enhanced CT imaging, careful evaluation for specific findings, and consideration of PDH as a differential diagnosis in young male patients with recurrent, unexplained abdominal pain are crucial. Timely recognition and intervention are essential to prevent complications such as bowel ischemia, necrosis, or perforation, significantly improving patient outcomes.
Conclusion
Left PDHs are a rare but important differential diagnosis of small bowel obstruction, particularly in patients without prior abdominal surgeries. Early recognition using contrast-enhanced CT, which reveals features such as clustered bowel loops and mesenteric vessel displacement, is critical to prevent complications like ischemia or necrosis. Both open and laparoscopic surgeries are effective, with the choice determined by the hernia’s complexity and patient factors. In this case, open surgery was required due to laparoscopic reduction failure, concerns about bowel ischemia, and the need for enhanced visualization. Timely diagnosis and intervention not only reduce complications but also minimize hospital stays and healthcare costs.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Funding
None declared.



