-
PDF
- Split View
-
Views
-
Cite
Cite
Taifen Kang, Weihua Huang, Yi Li, Guangyao Zhong, Hong Zhang, Laparoscopic resection of an isolated iliac artery aneurysm with synthetic graft implantation, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf031, https://doi.org/10.1093/jscr/rjaf031
Close - Share Icon Share
Abstract
The current treatment options for isolated iliac artery aneurysm (IIAA) are mainly endovascular treatment (ET) and open surgery. ET carries risks such as endoleaks and stent displacement, while open elective surgical repair of IIAAs carries significant risk of mortality. Therefore, this report presents a case of laparoscopic surgery for IIAA, providing a new approach for treating IIAA. Under laparoscopic guidance, the IIAA was resected, and an artificial graft was implanted to complete the surgery. At 6 months follow-up, the patient remained well, and the artificial graft was patent.
Introduction
True isolated iliac artery aneurysm (IIAA) is quite a rare disease where the lesion is confined to the iliac artery, without the aortic involvement [1]. As early as 2001, Dion et al. [2] reported complete laparoscopic management of abdominal aortic aneurysms, which attracted the attention of surgeons due to its minimally invasive nature and rapid recovery. However, due to the long learning curve and technical difficulties associated with laparoscopic vascular surgery, it has not been widely applied in clinical practice. Reports of laparoscopic treatment of IIAA are rare; here we describe a case of IIAA treated successfully using the laparoscopic technique.
Case presentation
A 62-year-old woman presented to her primary care with 1 year history of constipation and was transferred to the author's hospital after computed tomography (CT) examination revealed a left iliac aneurysm on 15 April 2024. The patient was 13 years post pituitary tumor resection and 3 years post bilateral hip replacement. On physical examination, a pulsatile mass was palpable in the left lower abdomen, which was mildly tender, and no other positive signs were found. CT indicated that the left common iliac artery exhibited fusiform dilation measuring 81 mm × 65 mm × 91 mm, with a proximal neck of 7 mm, bending nearly 90° to the left (Fig. 1a and b). Due to a short proximal neck, significant angulation of the aneurysm neck, and a large aneurysm sac, the patient was not a suitable candidate for endovascular treatment. To minimize the trauma associated with open surgery, the patient underwent laparoscopic left IIAA resection and synthetic graft implantation on 17 April 2024.
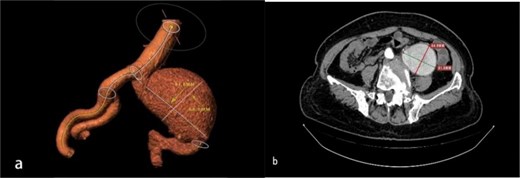
(a, b) Preoperative left common iliac artery aneurysm size and location.
The patient was placed under general anesthesia in a head-down position at a 30° angle, with the body tilted 15° to the right. A five-port approach was utilized (Fig. 2).
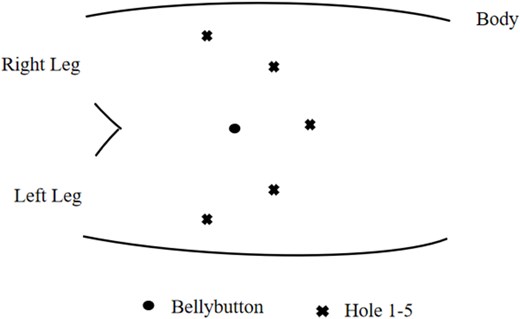
Schematic illustration of the position of the five laparoscopic ports.
The aneurysm was explored by incising the peritoneum over the left colonic sulcus. Then the abdominal aorta, right iliac artery, and the left iliac artery aneurysm were exposed and controlled (Fig. 3a). Above the bifurcation of the abdominal aorta, the decortication was freed retroperitoneally for 3 cm. The vascular occlusion bands and Bulldog vascular clamps were sequentially applied to the abdominal aorta, right common iliac artery, left external iliac artery, and left internal iliac artery. The excision of the aneurysm was performed with an appropriately long synthetic graft (Gore HT08708OW) anastomosed end to end with the left common iliac artery and the left external iliac artery at an oblique incision, respectively. Perform silk ligation of the left internal iliac artery and close with a Hemlock clip. After successful anastomosis, blood flow was restored without the use of any balloon occlusion devices (Fig. 3b).
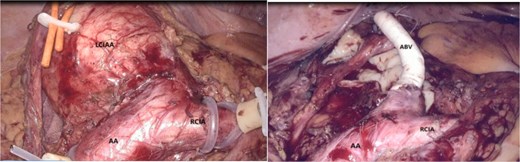
(a, b) Laparoscopic visualization of iliac artery aneurysms (AA abdominal aorta, RCIA right common iliac artery, LCIAA left common iliac artery aneurysm, ABV artificial blood vessel).
The surgery lasted 300 min, with an abdominal aorta occlusion time of 140 min and an iliac artery graft anastomosis time of 120 min. The patient resumed his mobility on the second postoperative day. The patient had an uneventful postoperative recovery with relief of constipation. A CT scan on the fifth postoperative day confirmed the patency of the synthetic graft (Fig. 4). The total length of hospital stay was 9 days. At the 6-month follow-up via phone call, the patient was reported to be in good condition. A color Doppler ultrasound performed at the primary care showed that the graft was patent.

Postoperative CT showing the left common iliac artery aneurysm being repaired with the artificial graft in situ and left internal iliac artery being ligated.
Discussion
The European Society for Vascular Surgery 2024 Clinical Guidelines recommend considering surgical treatment for IIAA when the diameter exceeds 40 mm [3].
In recent decades, endovascular treatment (ET) has been established to open surgery and has become more common in clinical practice [4]. ET is widely accepted due to its minimally invasive nature, reduced bleeding, and lower mortality rates [5]. Depending on the aneurysmal and aortic and contralateral iliac artery anatomy, aneurysmal neck length, position and degree of distortion, either a single stent placement in the diseased iliac artery or kissing stents can be deployed to treat the aneurysmal condition. Sahgal et al. [6] suggest that for a durable endovascular repair of IIAA, with an isolated stent graft, there must be sufficient proximal and distal neck of the aneurysm, ideally >15 mm and the internal artery should not be involved. If the proximal neck to the aorta is <15 mm, application of a bifurcated stent graft would be the therapy of choice [7]. After stent implantation for IIAA, residual arterial sacs may still compress surrounding organs, leading to complications [5, 8]. Considering this case, the patient’s constipation symptoms are attributed to compression of the rectum and colon by IIAA, and these symptoms may not resolve after ET. In recent years, it has been increasingly recognized that vascular interventional therapy may lead to various complications, including endoleaks, stent migration, aneurysm rupture, and thrombus formation. In this case, the neck was 7 mm, and the aneurysm diameter was 81 mm. Based on these facts, we did not consider ET to be the optimal treatment choice for this patient.
Open iliac artery reconstruction is highly invasive. This prompted us to consider other, more suitable treatment options.
In 2001, Dion et al. [2] reported the use of laparoscopic techniques for treating abdominal aortic aneurysms; however, this method has not been widely adopted, and there are few reports on laparoscopic treatment of IIAA. In this case, the aneurysm diameter reached 81 mm with a length of 91 mm, categorizing it as a giant IIAA. Our experience from this surgery includes the following insights:
(1) Laparoscopic IIAA resection and synthetic graft implantation are technically feasible and align with hemodynamic principles.
(2) Positioning the patient with the head down at a 30° angle and tilted 15° to the right allowed for better exposure of the IIAA through a transabdominal approach into the retroperitoneal space beside the descending colon.
(3) The five-port technique, assisted by an operator, improved efficiency.
(4) The use of vascular occlusion bands and clamps for double-layer blood flow occlusion ensured effective blockage without damaging the vessel wall.
(5) Exposure of the iliac artery was superior under laparoscopic guidance, facilitating the procedure.
(6) The magnifying effect of the laparoscope enhanced the precision of vessel anastomosis.
(7) Creating a beveled incision at the anastomosis increased the surface area and effectively prevented narrowing.
(8) Laparoscopic surgery allowed for earlier mobilization postoperatively. This is consistent with the findings reported by Leissner et al. [9], where the laparoscopic surgical approach accelerates recovery by reducing abdominal wall trauma and the resultant inflammatory and pain responses.
In summary, laparoscopic techniques for treating IIAA offer advantages such as fewer complications, quicker recovery, clear visualization, and precise magnification.
Conflict of interest statement
The authors declare that they have no conflicts of interest.
Funding
This study was supported by the Internal Startup Fund of the Sixth Affiliated Hospital of Jinan University (JDLY2022002).



