-
PDF
- Split View
-
Views
-
Cite
Cite
Abdulaziz Aldrees, Ahad Alotaibi, Mariam Alshammari, Sultan Alhabdan, Rare incidental retroperitoneal schwannoma discovered as an adrenal mass upon pre-renal transplant workup: case report, Journal of Surgical Case Reports, Volume 2025, Issue 12, December 2025, rjaf879, https://doi.org/10.1093/jscr/rjaf879
Close - Share Icon Share
Abstract
Schwannomas are benign tumors originating from Schwann cells of the peripheral nervous system. They can occur anywhere in the body but are typically located in the head, neck, and flexor surfaces of the extremities. Retroperitoneal schwannoma is sporadic and accounts for only 4% of all retroperitoneal tumors and 3% of all schwannomas. The lesion was incidentally discovered in most patients upon investigation for another reason. We are reporting a case of a patient known to have hypertension, which was complicated by end-stage renal disease, and she started on hemodialysis in 2021. The patient planned for a kidney transplant, and a pre-renal transplant workup showed incidental findings of an adrenal mass. Further imaging and investigation revealed a non-functioning tumor. She planned for a laparoscopic adrenalectomy. Intraoperatively, the mass was retroperitoneal, close to the adrenal gland but not arising from it. Postoperative histopathology revealed a Schwannoma.
Introduction
Schwannomas (neurilemmomas) are encapsulated nerve sheath tumors that are usually located on the head, neck, and flexor surfaces of the extremities. Retroperitoneal schwannoma (RS) is exceptionally rare, accounting for only 4% of all retroperitoneal tumors and 3% of all schwannomas [1]. The diagnosis is challenging and is often an incidental finding with late presentation [2]. Patients usually exhibit non-specific complaints like abdominal pain, discomfort, constipation, or if it reaches a significant size, it may cause compressive symptoms [3]. Furthermore, some may be present with deep venous thrombosis [2]. Radiology images play an essential role in the diagnostic approach [3]. Enhanced computed tomography (CT) scan typically identifies a well-defined tumor with slightly lower density than soft tissue due to the high content of myelin and fat [3]. Magnetic resonance imaging (MRI) is superior to CT in defining the margins and identifying the nerve origin [3]. However, the diagnosis of schwannoma based on imaging or even with needle biopsy is difficult and has many limitations [4, 5]. Hence, complete surgical resection is recommended in almost all cases and provides an accurate pathological examination [4]. Differential diagnosis includes neurofibromas, paragangliomas, and ganglioneuromas.
Neurofibromas are round or irregular masses along nerves with well-defined borders but no capsule, sometimes containing cysts, hemorrhages, and showing heterogeneous enhancement on images [6]. Paraganglioma is primarily located in the sympathetic chain on both sides of the spine. It may be complemented by cystic degeneration, calcification, or necrosis, and may be accompanied by paroxysmal hypertension, and the enhancement after enhanced study is more evident than that of schwannoma [6]. The ganglioneuroma has clear boundaries and may exhibit pseudopodia-like or embedded growth. It shows uniform density with calcification or fatty degeneration, less cystic consolidation, and unclear enhancement [6]. Needle biopsy is rarely recommended due to pitfalls and higher complication risks, especially near blood vessels, where damage risk is elevated [5]. Moreover, tumor heterogeneity can cause an inaccurate needle biopsy or misdiagnosis of malignant tumors [5]. A retrospective study of 79 patients between 2010 and 2020 was conducted based on pathological examination after surgical resection with RS, and it was concluded that preoperative diagnosis of RS is usually impossible due to its rarity and lack of special clinical and radiographic features. RS should be considered in the differential diagnosis for unilateral well-circumscribed heterogeneous retroperitoneal masses with heterogeneous or delayed enhancement [7]. In this report, we present a case of an incidental RS that was discovered as an adrenal mass upon pre-renal transplant workup.
Case report
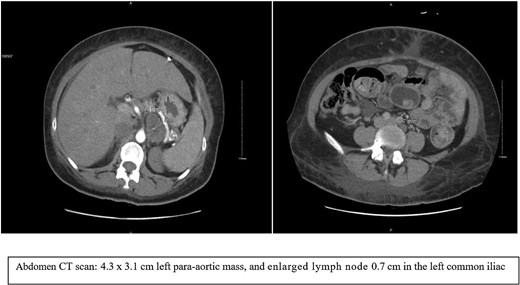
We are reporting a 38-year-old female patient known to have uncontrolled type 2 diabetes mellitus and hypertension, which was complicated by end-stage renal disease (ESRD), and she started on hemodialysis in 2021. The patient planned for a kidney transplant, and a pre-renal transplant workup was initiated. Abdomen (CT) was done as part of the workup, and an incidental finding of an adrenal mass were found. The patient was referred to our clinic for further management. She was asymptomatic. CT abdomen reviewed as shown in Fig. 1, which showed a 4.3 × 3.1 cm left para-aortic mass with punctate calcification and heterogeneous enhancement; the mass abuts the left adrenal, stomach, and posterior border of the pancreas; the region of the mass is indeterminate. There are a few prominent para-aortic and retroperitoneal lymph nodes; the largest measures 0.7 cm in the left common iliac group. A left suprarenal heterogeneous mass could arise from the left adrenal gland; further evaluation by MRI is advised. The case was flagged as suspected oncology case.
MRI as shown in (Fig. 2), a 2.2 × 4.5 × 3.5 cm well-defined, mostly separable left para-aortic mass from the spleen and pancreas, arising from the left adrenal gland. It is hypointense on T1, heterogeneously hyperintense on T2, with slow enhancement, mild diffusion restriction, central calcification, and necrosis—no invasion into adjacent structures. Differential diagnoses include ganglioneuroma and hemangioma. Further positron emission tomography (PET/CT) is recommended to confirm benignity and rule out adrenocortical carcinoma.
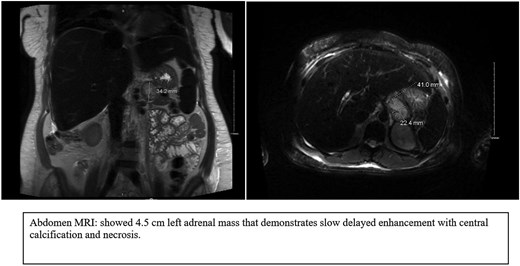
MRI images showed a well-defined left para-aortic mass that mostly arises from the left adrenal gland.
A PET/CT scan (Fig. 3) showed mild heterogeneous fluorodeoxyglucose (FDG) uptake in a mixed-density left adrenal mass with calcifications. The radiologist suspected a left adrenal mass, with differential diagnoses including pheochromocytoma or previous hemorrhage.
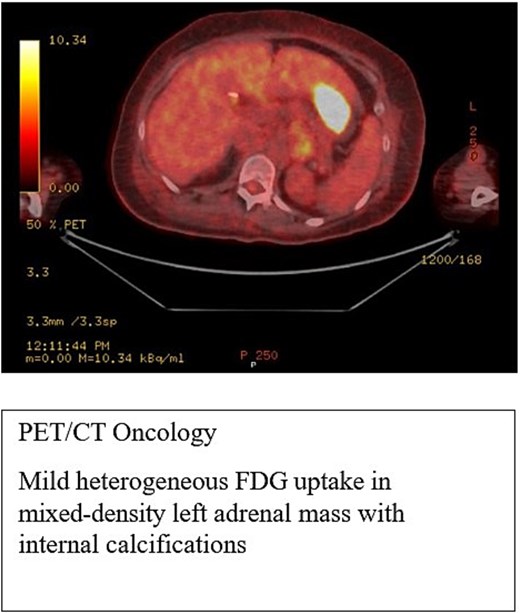
PET-CT scan showed heterogeneous FDG uptake in a mixed-density left adrenal mass with internal calcifications.
The endocrinology team reviewed the patient before surgery. A workup was ordered and was negative for metanephrine and normetanephrine. A 1 mg dexamethasone suppression test was performed, but was not fully suppressed, likely due to ESRD, as per endocrinology. The patient showed no signs of Cushing’s syndrome, pheochromocytoma, or adrenal tumors like Conn’s syndrome, and was cleared for surgery.
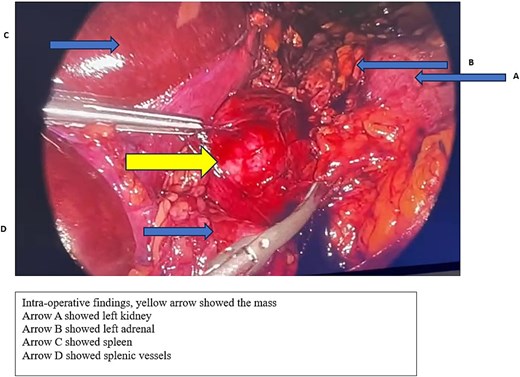
The patient was admitted electively for the planned laparoscopic left adrenalectomy. Intraoperatively, the left adrenal gland was identified and appeared normal. A large para-aortic mass, ~5–6 cm, was found near the adrenal, adherent to it, and attached to the splenic artery. The mass was resected and completely removed. Veins draining into the renal vein were clipped. The final procedure involved resection of the retroperitoneal mass without removal of the adrenal gland, as shown in Fig. 4. The patient tolerated the surgery well and had an uncomplicated postoperative course.
Final histopathology: no intact adrenal gland was found, and a panel of immunostains was performed. Tumor cells are positive for S100 and negative for NFP, SMA, HMB45, MelanA, and Desmin, indicating a neural origin or Schwann cell origin.
Discussion
RSs are rare. Similar cases have been reported, and a literature review by Wilson et al. documented 121 cases from 1986 to 2018 [8]. In most reported cases, the patients were asymptomatic, and the lesion was discovered incidentally during investigations for other reasons, as in our patient [8]. The rarity of these cases makes the pre-operative diagnosis difficult to establish, but a benign schwannoma is a differential consideration for any suspected suprarenal malignant lesions [8]. A few radiological features by CT scan can help in the differential diagnosis. These features include well-encapsulated margins, punctate calcifications, and marked heterogeneity with a centrally cystic/necrotic core, which was presented in 50% of the reported cases [8]. Generally, patients with post-operative pathology of Schwannomas had good outcomes and prognosis with a low incidence of recurrence [9].
Conclusion
RS is exceptionally very rare and accounts for only 4% of all retroperitoneal tumors and 3% of all schwannomas. The diagnosis is challenging and most often found to be incidental upon investigation for another reason. Radiology images play an essential role in the diagnostic approach, but the rarity of these cases makes the pre-operative diagnosis difficult to establish. Surgical resection is the mainstay for management, and the histopathologic examination is the most reliable method to diagnose adrenal schwannoma.
Conflict of interest statement
None declared.
Funding
There was no financial support.



