-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Almomen, Moath A Alfaleh, Omar Alanzi, Mohsen M Bashammakh, Sellar–suprasellar pituitary lymphoma mimicking pituitary adenoma: a case report with literature review, Journal of Surgical Case Reports, Volume 2025, Issue 10, October 2025, rjaf447, https://doi.org/10.1093/jscr/rjaf447
Close - Share Icon Share
Abstract
Sellar–suprasellar lymphoma (SSL) is an extremely rare tumor, constituting fewer than 1%. It is a variant of primary central nervous system lymphoma. SSL is usually seen in people around 60 years of age, exhibiting a slight female predominance. Diffuse large B-cell lymphoma represents the most predominant subtype. We report a 57-year-old female with a 9-month history of worsening severe left-sided headaches involving the left eye, associated with nausea, vomiting, blurred vision, and significant unintentional weight loss. Initial imaging revealed a pituitary tumor, and she was diagnosed with a pituitary macroadenoma. She underwent endoscopic trans-sphenoidal debulking. Histopathological examination confirmed a high-grade diffuse large B-cell lymphoma. She was treated with chemotherapy and radiotherapy which reduced the mass and improved her symptoms. Our case underscores the importance of considering SSL, particularly in patients with unusual sellar masses. Effective treatment needs a multidisciplinary approach, integrating radiotherapy and endocrine support when demanded.
Introduction
Sellar–suprasellar lymphoma (SSL) is a very rare tumor, constituting fewer than 1% of surgically treated pituitary masses [1]. It is a variant of primary central nervous system lymphoma, which affects the brain, spinal cord, or eyes without systemic spread [2]. SSL is usually seen in people around 60 years of age, exhibiting a slight female predominance, and commonly presents with headache, hypopituitarism, and vision disturbances [3]. Notably, most reported cases of SSL are of B-cell origin, with diffuse large B-cell lymphoma representing the predominant subtype [4]. Given its rarity, diagnosis is often difficult and usually confirmed through histopathological analysis [5].
Case presentation
A 57-year-old female known to have type 2 diabetes mellitus, hypertension, dyslipidemia, and hyperprolactinemia presented with severe, pulsatile left-sided headaches impacting the left eye, rated 10/10 in severity, and associated with lacrimation and blurred vision in the affected eye, nausea, vomiting, and unintentional weight loss of 20 kg over 9 months. Afterward, her blurry vision progressed to left temporal hemianopia accompanied by intermittent fevers, night sweats, and fatigue. The initial neurological examination was unremarkable; however, the patient later developed decreased visual acuity bilaterally, with greater impairment on the left side, and lower limb motor strength was also reduced.
The initial evaluation included a brain magnetic resonance imaging (MRI), showing a small pituitary mass measuring 1.3 × 2.1 × 1.9 cm with suprasellar extension, neighboring the optic chiasm (Figs 1 and 2). Laboratory results revealed a high prolactin level of 110 ng/ml and normal thyroid function tests. A pituitary macroadenoma, specifically a prolactinoma, was presumed, and cabergoline was initiated.
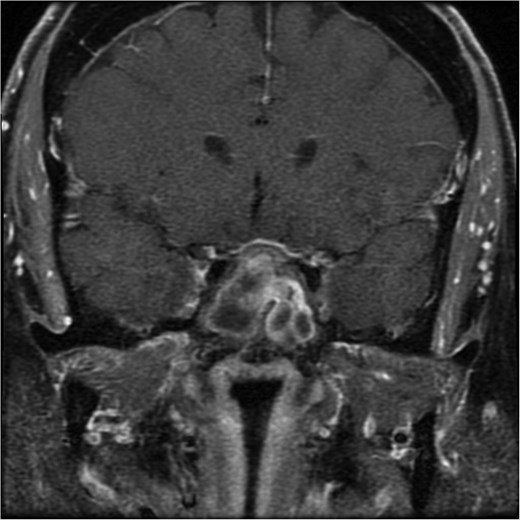
A coronal brain MRI showing a heterogeneous, enhancing lesion located within the sphenoid sinus, extending superiorly to the sellar and parasellar regions. The mass shows irregular borders and appears to cause a mild compression of the optic chiasm.
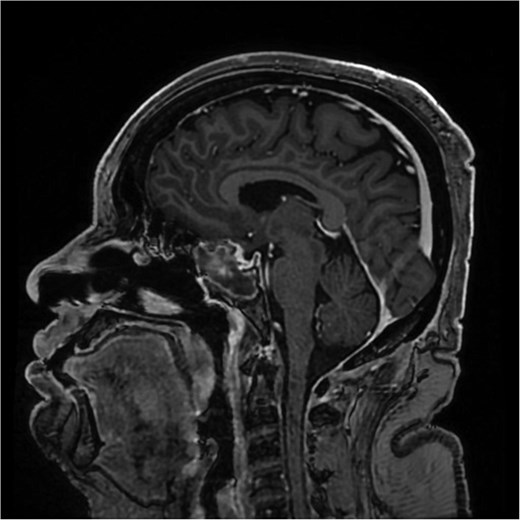
A sagittal brain MRI reveals the same mass with superior extension to the sellar and suprasellar regions. The lesion is exerting a compression to the optic chiasm. The mass effect extends posteriorly toward the clivus, with irregular margins indicating invasive potential. Adjacent structures like the pituitary stalk appear to be displaced.
Despite treatment with cabergoline, follow-up prolactin level remained elevated, and imaging showed a growing tumor size. Clinically, the patient's symptoms persisted, with worsening headaches. Afterward, her prolactin level had dramatically risen to 2000 ng/ml. She was admitted with daily severe headaches, abdominal pain, vomiting, and oral intake intolerance. A brain MRI demonstrated an enlarged sellar and suprasellar mass measuring 3.2 × 1.7 × 3.0 cm, compressing the optic chiasm. Additionally, her prolactin level diminished to 2.7 ng/ml, raising concern of a growing pituitary macroadenoma.
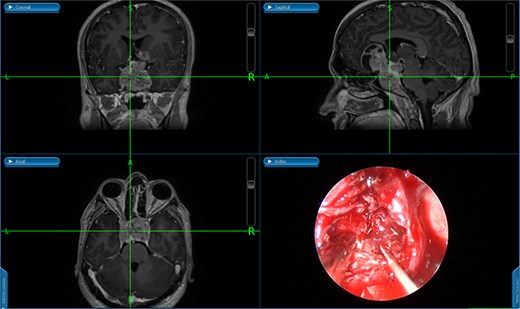
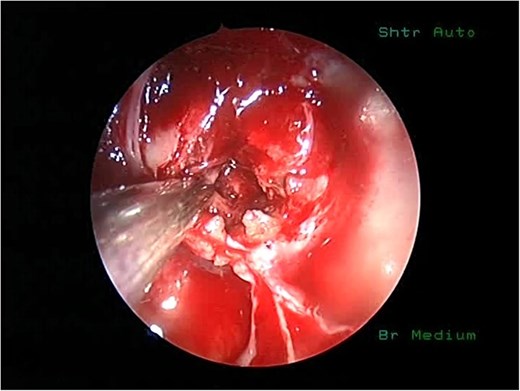
She underwent endoscopic trans-sphenoidal debulking of the suprasellar lesion (Figs 3 and 4). Postoperatively, the patient developed complications, including diabetes insipidus and panhypopituitarism, requiring levothyroxine and corticosteroid replacement therapy. Histopathology revealed a diagnosis of high-grade primary central nervous system (CNS) B-cell lymphoma. Microscopic analysis showed sheets of atypical lymphoid cells with high mitotic activity. Consequently, the patient was initiated on rituximab and high-dose methotrexate (HD-MTX). Nevertheless, methotrexate was terminated due to the onset of acute kidney injury. Given the patient's intolerance to further HD-MTX, nivolumab was commenced based on PD-L1 expression. While there was partial symptom relief, the tumor response was inadequate. Therefore, the patient underwent whole-brain radiotherapy with a boost to the pituitary region, receiving a total dose of 45 Gy over 25 fractions. This treatment was effective, though she experienced alopecia, mild nausea, blurred vision, headaches, and severe vulvar itching.
During the follow-up appointment, the patient exhibited positive progress, and her nausea was managed with ondansetron. Her MRI demonstrated stable disease with a slight tumor size reduction. She maintained hormone replacement therapy and was scheduled for routine MRI follow-ups. The treatment of endocrine imbalances led to an improvement in her quality of life, coupled by ongoing multidisciplinary support.
Discussion
A review of the literature demonstrated the difference in characteristics of patients with SSL (Table 1). The age and gender distribution of SSL exhibits variability among the studied cases. The participants comprised younger adults aged 37–45 years, middle-aged adults aged 45–61 years, and older adults aged 61–86 years, representing the majority of reported cases [1–15]. The gender decomposition demonstrated 12 females and 5 males [1–15].
| Study . | Age, gender . | Clinical features . | Endocrine imbalances . | Imaging finding . | Histopathology . | Management . | Follow-up . |
|---|---|---|---|---|---|---|---|
| [6] | 82, M | Headache, hemianopia, vision loss, and papilledema | Panhypopituitarism | Heterogeneously isointense bilobed tumor enlarging the pituitary fossa with severe compression to the optic chiasm and hypothalamus | DLBCL | Palliative field RT | N/R |
| [1] | 47, F | Worsening headache, blurry vision, right CN III and V palsies, and bitemporal hemianopia | Hyperprolactinemia | Sellar mass with partial involvement of the right internal carotid artery within the cavernous sinus | DLBCL | Surgery, CHT (DeAngelis protocol, R-CHOP, R-ICE), prophylactic intrathecal MTX, autologous stem cell transplantation | Clinical remission following 8 months of stem cell transplantation |
| [3] | 61, M | Headache, unilateral ptosis, unclear vision, anorexia and weakness | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Sellar mass reaching to the cavernous sinus and right sphenoid | DLBCL | CHT (rituximab, MTX, lenalidomide), intrathecal dexamethasone, and cytarabine | Clinical improvement, mass size reduction following two courses of chemotherapy |
| [3] | 65, F | Headache, N/V, increased urination and thirst, anorexia, and weakness | Panhypopituitarism | Sellar mass which was not differentiated from the optic chiasm | DLBCL | CHT | Died 8 months following diagnosis |
| [12] | 74, M | Bitemporal visual field deficit, worsening weakness, seizure episodes, dizziness with falls, altered mental status, dementia, impotence, constipation | Deficiency of anterior pituitary hormones | Sellar and suprasellar tumor with erosion of the left sellar floor | Large B-cell lymphoma | Surgery, a course of 4600 cGy conventional RT | Died shortly after RT |
| [12] | 65, M | Diplopia, right retrobulbar pain, low energy, and libido | Deficiency of anterior pituitary hormones | Sellar and suprasellar lesion extending into the right cavernous sinus with associated erosion of the sphenoid sinus. | High-grade, large B- cell lymphoma | Surgery, stereotactic radiosurgery and Codox-M of 4 cycles | Died 2 years later due to pulmonary failure |
| [15] | 86, F | Fever spikes, chills, night sweats, and weight loss | Partial deficiency of anterior pituitary hormones | Sellar mass within a slightly enlarged pituitary fossa | B-cell lymphoma | Surgery and CHT | Died 3 months following diagnosis |
| [13] | 41, F | Polyuria, polydipsia, amenorrhea syndrome and galactorrhea | Partial deficiency of anterior pituitary hormones Hyperprolactinemia | Intrasellar and suprasellar mass with thickening of the pituitary stalk and obstructive hydrocephalus | High-grade, large B-cell lymphoma | Surgery, RT (25 fractions of 200 cGy for a total dose of 5000 cGy) and intrathecal MTX | Symptom free for 7 months following management |
| [2] | 69, F | Right frontotemporal headache which developed later to right ptosis, diplopia, and III CN palsy | Hyperprolactinemia High IGF-1 Central hypothyroidism | Large sellar and suprasellar mass with sphenoid bone remodeling with optic chiasm compression and right cavernous sinus invasion | DLBCL | 4 cycles of MATRix regimen (methotrexate, cytarabine, thiotepa, and rituximab) | Died of sepsis 3 months later |
| [9] | 45, F | Headache, dizziness, unclear vision, bitemporal hemianopsia, ptosis, numbness of the face | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Heterogeneous sellar–suprasellar lesion with impingement on the optic nerves and chiasm, and involvement of the cavernous sinuses with thickening of the pituitary stalk | B-cell lymphoma | Surgery, CHT (MTX, vincristine, procarbazine and dexamethasone), R-ICE regimen and autologous transplant | Preserved neurological function 3 months postoperatively, with no signs of disease recurrence. |
| [4] | 61, F | Worsening headaches and acromegaly | High GHRH and IGF-1 Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Isointense, homogenously enhancing sellar tumor without evidence of pituitary stalk displacement | DLBCL, somatotroph hyperplasia | 3 cycles of R-CHOP with 3600 cGy of stereotactic RT and 180 cGy for 20 fractions within 27 days | No evidence of mass after 2 months of RT and normalization of prolactin and IGF-1 within 5 months |
| [10] | 37, M | Headaches and progression of visual acuity, bilateral blurred vision, and bitemporal hemianopia | No imbalances | Large intrasellar tumor with a widening of the sella turcica, extending backward into the anteropontal cisterns, which were narrowed, upward enclosing the hypothalamic infundibulum and optic chiasm, cavernous sinus, and sphenoidal involvement | Large B-cell lymphoma | Surgery, 6 cycles of CHOP (cyclophosphamide, vincristine, adriamycin, prednisone), whole-brain RT (dose of 40 Gy and boosted to the tumor 50 Gy) | Stable residual tumor and after 52 months of follow-up, the patient had a mild visual field defect in the right eye. |
| [11] | 59, F | Headache and diplopia | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Sellar mass extending to the suprasellar cistern and involving the pituitary stalk and cavernous sinuses | High-grade B-cell non-Hodgkin’s lymphoma | No management | Died before starting therapy |
| [14] | 71, F | CN VII palsy, bilateral temporal hemianopsia, syncopal spells, acromegaly | High GH and IGF-1 | Well-defined mass extending into the suprasellar cistern, compressing the optic chiasm, and penetrating right cavernous sinus | Large B-cell lymphoma, adenoma, and lymphocytic hypophysitis | Surgery and intensity-modulated RT at dose of 5040 cGy | Complete remission after 1 year of therapy |
| [5] | 73, F | Headache, double vision, retro-orbital pain | Diabetes insipidus | Sellar mass extending to the suprasellar cistern, cavernous sinus, and orbital apex with involvement of the optic chiasm and optic nerve | DLBCL | Surgery, R-CHOP, and high-dose MTX | Improvement after 15 months of RT |
| [7] | 67, F | Headache and left visual field defect | No imbalances | Pituitary mass extending downward to the sphenoid sinus | Diffuse, large, high-grade B-cell pituitary lymphoma | Surgery, stereotactic RT and CHT (4 cycles) | No recurrence after 15 months of follow-ups |
| [8] | 60, F | Weakness, headache, and ptosis | Partial deficiency of anterior pituitary hormones | Pituitary sellar mass extending into the suprasellar region, compressing the optic chiasm, and infiltrating the left cavernous sinus | DLBCL | Surgery, CHT with intraspinal MTX infusion, and R-MPV regimen | Died from hospital-acquired infection |
| Our case | 57, F | Headache, left eye lacrimation, blurry vision, temporal hemianopia, nausea, vomiting, and weight loss | Hyperprolactinemia | Large sellar and suprasellar mass, compressing the optic chiasm, and extending posteriorly toward the clivus with displacement of pituitary stalk | DLBCL | Surgery, rituximab and high-dose MTX which was replaced with nivolumab and whole-brain RT (total dose of 45 Gy over 25 fractions) | Clinically improved with a slight reduction in the mass size |
| Study . | Age, gender . | Clinical features . | Endocrine imbalances . | Imaging finding . | Histopathology . | Management . | Follow-up . |
|---|---|---|---|---|---|---|---|
| [6] | 82, M | Headache, hemianopia, vision loss, and papilledema | Panhypopituitarism | Heterogeneously isointense bilobed tumor enlarging the pituitary fossa with severe compression to the optic chiasm and hypothalamus | DLBCL | Palliative field RT | N/R |
| [1] | 47, F | Worsening headache, blurry vision, right CN III and V palsies, and bitemporal hemianopia | Hyperprolactinemia | Sellar mass with partial involvement of the right internal carotid artery within the cavernous sinus | DLBCL | Surgery, CHT (DeAngelis protocol, R-CHOP, R-ICE), prophylactic intrathecal MTX, autologous stem cell transplantation | Clinical remission following 8 months of stem cell transplantation |
| [3] | 61, M | Headache, unilateral ptosis, unclear vision, anorexia and weakness | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Sellar mass reaching to the cavernous sinus and right sphenoid | DLBCL | CHT (rituximab, MTX, lenalidomide), intrathecal dexamethasone, and cytarabine | Clinical improvement, mass size reduction following two courses of chemotherapy |
| [3] | 65, F | Headache, N/V, increased urination and thirst, anorexia, and weakness | Panhypopituitarism | Sellar mass which was not differentiated from the optic chiasm | DLBCL | CHT | Died 8 months following diagnosis |
| [12] | 74, M | Bitemporal visual field deficit, worsening weakness, seizure episodes, dizziness with falls, altered mental status, dementia, impotence, constipation | Deficiency of anterior pituitary hormones | Sellar and suprasellar tumor with erosion of the left sellar floor | Large B-cell lymphoma | Surgery, a course of 4600 cGy conventional RT | Died shortly after RT |
| [12] | 65, M | Diplopia, right retrobulbar pain, low energy, and libido | Deficiency of anterior pituitary hormones | Sellar and suprasellar lesion extending into the right cavernous sinus with associated erosion of the sphenoid sinus. | High-grade, large B- cell lymphoma | Surgery, stereotactic radiosurgery and Codox-M of 4 cycles | Died 2 years later due to pulmonary failure |
| [15] | 86, F | Fever spikes, chills, night sweats, and weight loss | Partial deficiency of anterior pituitary hormones | Sellar mass within a slightly enlarged pituitary fossa | B-cell lymphoma | Surgery and CHT | Died 3 months following diagnosis |
| [13] | 41, F | Polyuria, polydipsia, amenorrhea syndrome and galactorrhea | Partial deficiency of anterior pituitary hormones Hyperprolactinemia | Intrasellar and suprasellar mass with thickening of the pituitary stalk and obstructive hydrocephalus | High-grade, large B-cell lymphoma | Surgery, RT (25 fractions of 200 cGy for a total dose of 5000 cGy) and intrathecal MTX | Symptom free for 7 months following management |
| [2] | 69, F | Right frontotemporal headache which developed later to right ptosis, diplopia, and III CN palsy | Hyperprolactinemia High IGF-1 Central hypothyroidism | Large sellar and suprasellar mass with sphenoid bone remodeling with optic chiasm compression and right cavernous sinus invasion | DLBCL | 4 cycles of MATRix regimen (methotrexate, cytarabine, thiotepa, and rituximab) | Died of sepsis 3 months later |
| [9] | 45, F | Headache, dizziness, unclear vision, bitemporal hemianopsia, ptosis, numbness of the face | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Heterogeneous sellar–suprasellar lesion with impingement on the optic nerves and chiasm, and involvement of the cavernous sinuses with thickening of the pituitary stalk | B-cell lymphoma | Surgery, CHT (MTX, vincristine, procarbazine and dexamethasone), R-ICE regimen and autologous transplant | Preserved neurological function 3 months postoperatively, with no signs of disease recurrence. |
| [4] | 61, F | Worsening headaches and acromegaly | High GHRH and IGF-1 Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Isointense, homogenously enhancing sellar tumor without evidence of pituitary stalk displacement | DLBCL, somatotroph hyperplasia | 3 cycles of R-CHOP with 3600 cGy of stereotactic RT and 180 cGy for 20 fractions within 27 days | No evidence of mass after 2 months of RT and normalization of prolactin and IGF-1 within 5 months |
| [10] | 37, M | Headaches and progression of visual acuity, bilateral blurred vision, and bitemporal hemianopia | No imbalances | Large intrasellar tumor with a widening of the sella turcica, extending backward into the anteropontal cisterns, which were narrowed, upward enclosing the hypothalamic infundibulum and optic chiasm, cavernous sinus, and sphenoidal involvement | Large B-cell lymphoma | Surgery, 6 cycles of CHOP (cyclophosphamide, vincristine, adriamycin, prednisone), whole-brain RT (dose of 40 Gy and boosted to the tumor 50 Gy) | Stable residual tumor and after 52 months of follow-up, the patient had a mild visual field defect in the right eye. |
| [11] | 59, F | Headache and diplopia | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Sellar mass extending to the suprasellar cistern and involving the pituitary stalk and cavernous sinuses | High-grade B-cell non-Hodgkin’s lymphoma | No management | Died before starting therapy |
| [14] | 71, F | CN VII palsy, bilateral temporal hemianopsia, syncopal spells, acromegaly | High GH and IGF-1 | Well-defined mass extending into the suprasellar cistern, compressing the optic chiasm, and penetrating right cavernous sinus | Large B-cell lymphoma, adenoma, and lymphocytic hypophysitis | Surgery and intensity-modulated RT at dose of 5040 cGy | Complete remission after 1 year of therapy |
| [5] | 73, F | Headache, double vision, retro-orbital pain | Diabetes insipidus | Sellar mass extending to the suprasellar cistern, cavernous sinus, and orbital apex with involvement of the optic chiasm and optic nerve | DLBCL | Surgery, R-CHOP, and high-dose MTX | Improvement after 15 months of RT |
| [7] | 67, F | Headache and left visual field defect | No imbalances | Pituitary mass extending downward to the sphenoid sinus | Diffuse, large, high-grade B-cell pituitary lymphoma | Surgery, stereotactic RT and CHT (4 cycles) | No recurrence after 15 months of follow-ups |
| [8] | 60, F | Weakness, headache, and ptosis | Partial deficiency of anterior pituitary hormones | Pituitary sellar mass extending into the suprasellar region, compressing the optic chiasm, and infiltrating the left cavernous sinus | DLBCL | Surgery, CHT with intraspinal MTX infusion, and R-MPV regimen | Died from hospital-acquired infection |
| Our case | 57, F | Headache, left eye lacrimation, blurry vision, temporal hemianopia, nausea, vomiting, and weight loss | Hyperprolactinemia | Large sellar and suprasellar mass, compressing the optic chiasm, and extending posteriorly toward the clivus with displacement of pituitary stalk | DLBCL | Surgery, rituximab and high-dose MTX which was replaced with nivolumab and whole-brain RT (total dose of 45 Gy over 25 fractions) | Clinically improved with a slight reduction in the mass size |
N/R, not reported; DLBCL, diffuse large B-cell lymphoma; RT, radiotherapy; CN, cranial nerve; CHT, chemotherapy; R-CHOP, rituximab-cyclophosphamide, vincristine, adriamycin, prednisone; R-ICE, rituximab, ifosfamide, carboplatin, etoposide; DeAngelis CHT protocol, methotrexate, vincristine, procarbazine, cytarabine; MTX, methotrexate; R-MPV, rituximab, methotrexate, vincristine, and procarvazine.
| Study . | Age, gender . | Clinical features . | Endocrine imbalances . | Imaging finding . | Histopathology . | Management . | Follow-up . |
|---|---|---|---|---|---|---|---|
| [6] | 82, M | Headache, hemianopia, vision loss, and papilledema | Panhypopituitarism | Heterogeneously isointense bilobed tumor enlarging the pituitary fossa with severe compression to the optic chiasm and hypothalamus | DLBCL | Palliative field RT | N/R |
| [1] | 47, F | Worsening headache, blurry vision, right CN III and V palsies, and bitemporal hemianopia | Hyperprolactinemia | Sellar mass with partial involvement of the right internal carotid artery within the cavernous sinus | DLBCL | Surgery, CHT (DeAngelis protocol, R-CHOP, R-ICE), prophylactic intrathecal MTX, autologous stem cell transplantation | Clinical remission following 8 months of stem cell transplantation |
| [3] | 61, M | Headache, unilateral ptosis, unclear vision, anorexia and weakness | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Sellar mass reaching to the cavernous sinus and right sphenoid | DLBCL | CHT (rituximab, MTX, lenalidomide), intrathecal dexamethasone, and cytarabine | Clinical improvement, mass size reduction following two courses of chemotherapy |
| [3] | 65, F | Headache, N/V, increased urination and thirst, anorexia, and weakness | Panhypopituitarism | Sellar mass which was not differentiated from the optic chiasm | DLBCL | CHT | Died 8 months following diagnosis |
| [12] | 74, M | Bitemporal visual field deficit, worsening weakness, seizure episodes, dizziness with falls, altered mental status, dementia, impotence, constipation | Deficiency of anterior pituitary hormones | Sellar and suprasellar tumor with erosion of the left sellar floor | Large B-cell lymphoma | Surgery, a course of 4600 cGy conventional RT | Died shortly after RT |
| [12] | 65, M | Diplopia, right retrobulbar pain, low energy, and libido | Deficiency of anterior pituitary hormones | Sellar and suprasellar lesion extending into the right cavernous sinus with associated erosion of the sphenoid sinus. | High-grade, large B- cell lymphoma | Surgery, stereotactic radiosurgery and Codox-M of 4 cycles | Died 2 years later due to pulmonary failure |
| [15] | 86, F | Fever spikes, chills, night sweats, and weight loss | Partial deficiency of anterior pituitary hormones | Sellar mass within a slightly enlarged pituitary fossa | B-cell lymphoma | Surgery and CHT | Died 3 months following diagnosis |
| [13] | 41, F | Polyuria, polydipsia, amenorrhea syndrome and galactorrhea | Partial deficiency of anterior pituitary hormones Hyperprolactinemia | Intrasellar and suprasellar mass with thickening of the pituitary stalk and obstructive hydrocephalus | High-grade, large B-cell lymphoma | Surgery, RT (25 fractions of 200 cGy for a total dose of 5000 cGy) and intrathecal MTX | Symptom free for 7 months following management |
| [2] | 69, F | Right frontotemporal headache which developed later to right ptosis, diplopia, and III CN palsy | Hyperprolactinemia High IGF-1 Central hypothyroidism | Large sellar and suprasellar mass with sphenoid bone remodeling with optic chiasm compression and right cavernous sinus invasion | DLBCL | 4 cycles of MATRix regimen (methotrexate, cytarabine, thiotepa, and rituximab) | Died of sepsis 3 months later |
| [9] | 45, F | Headache, dizziness, unclear vision, bitemporal hemianopsia, ptosis, numbness of the face | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Heterogeneous sellar–suprasellar lesion with impingement on the optic nerves and chiasm, and involvement of the cavernous sinuses with thickening of the pituitary stalk | B-cell lymphoma | Surgery, CHT (MTX, vincristine, procarbazine and dexamethasone), R-ICE regimen and autologous transplant | Preserved neurological function 3 months postoperatively, with no signs of disease recurrence. |
| [4] | 61, F | Worsening headaches and acromegaly | High GHRH and IGF-1 Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Isointense, homogenously enhancing sellar tumor without evidence of pituitary stalk displacement | DLBCL, somatotroph hyperplasia | 3 cycles of R-CHOP with 3600 cGy of stereotactic RT and 180 cGy for 20 fractions within 27 days | No evidence of mass after 2 months of RT and normalization of prolactin and IGF-1 within 5 months |
| [10] | 37, M | Headaches and progression of visual acuity, bilateral blurred vision, and bitemporal hemianopia | No imbalances | Large intrasellar tumor with a widening of the sella turcica, extending backward into the anteropontal cisterns, which were narrowed, upward enclosing the hypothalamic infundibulum and optic chiasm, cavernous sinus, and sphenoidal involvement | Large B-cell lymphoma | Surgery, 6 cycles of CHOP (cyclophosphamide, vincristine, adriamycin, prednisone), whole-brain RT (dose of 40 Gy and boosted to the tumor 50 Gy) | Stable residual tumor and after 52 months of follow-up, the patient had a mild visual field defect in the right eye. |
| [11] | 59, F | Headache and diplopia | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Sellar mass extending to the suprasellar cistern and involving the pituitary stalk and cavernous sinuses | High-grade B-cell non-Hodgkin’s lymphoma | No management | Died before starting therapy |
| [14] | 71, F | CN VII palsy, bilateral temporal hemianopsia, syncopal spells, acromegaly | High GH and IGF-1 | Well-defined mass extending into the suprasellar cistern, compressing the optic chiasm, and penetrating right cavernous sinus | Large B-cell lymphoma, adenoma, and lymphocytic hypophysitis | Surgery and intensity-modulated RT at dose of 5040 cGy | Complete remission after 1 year of therapy |
| [5] | 73, F | Headache, double vision, retro-orbital pain | Diabetes insipidus | Sellar mass extending to the suprasellar cistern, cavernous sinus, and orbital apex with involvement of the optic chiasm and optic nerve | DLBCL | Surgery, R-CHOP, and high-dose MTX | Improvement after 15 months of RT |
| [7] | 67, F | Headache and left visual field defect | No imbalances | Pituitary mass extending downward to the sphenoid sinus | Diffuse, large, high-grade B-cell pituitary lymphoma | Surgery, stereotactic RT and CHT (4 cycles) | No recurrence after 15 months of follow-ups |
| [8] | 60, F | Weakness, headache, and ptosis | Partial deficiency of anterior pituitary hormones | Pituitary sellar mass extending into the suprasellar region, compressing the optic chiasm, and infiltrating the left cavernous sinus | DLBCL | Surgery, CHT with intraspinal MTX infusion, and R-MPV regimen | Died from hospital-acquired infection |
| Our case | 57, F | Headache, left eye lacrimation, blurry vision, temporal hemianopia, nausea, vomiting, and weight loss | Hyperprolactinemia | Large sellar and suprasellar mass, compressing the optic chiasm, and extending posteriorly toward the clivus with displacement of pituitary stalk | DLBCL | Surgery, rituximab and high-dose MTX which was replaced with nivolumab and whole-brain RT (total dose of 45 Gy over 25 fractions) | Clinically improved with a slight reduction in the mass size |
| Study . | Age, gender . | Clinical features . | Endocrine imbalances . | Imaging finding . | Histopathology . | Management . | Follow-up . |
|---|---|---|---|---|---|---|---|
| [6] | 82, M | Headache, hemianopia, vision loss, and papilledema | Panhypopituitarism | Heterogeneously isointense bilobed tumor enlarging the pituitary fossa with severe compression to the optic chiasm and hypothalamus | DLBCL | Palliative field RT | N/R |
| [1] | 47, F | Worsening headache, blurry vision, right CN III and V palsies, and bitemporal hemianopia | Hyperprolactinemia | Sellar mass with partial involvement of the right internal carotid artery within the cavernous sinus | DLBCL | Surgery, CHT (DeAngelis protocol, R-CHOP, R-ICE), prophylactic intrathecal MTX, autologous stem cell transplantation | Clinical remission following 8 months of stem cell transplantation |
| [3] | 61, M | Headache, unilateral ptosis, unclear vision, anorexia and weakness | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Sellar mass reaching to the cavernous sinus and right sphenoid | DLBCL | CHT (rituximab, MTX, lenalidomide), intrathecal dexamethasone, and cytarabine | Clinical improvement, mass size reduction following two courses of chemotherapy |
| [3] | 65, F | Headache, N/V, increased urination and thirst, anorexia, and weakness | Panhypopituitarism | Sellar mass which was not differentiated from the optic chiasm | DLBCL | CHT | Died 8 months following diagnosis |
| [12] | 74, M | Bitemporal visual field deficit, worsening weakness, seizure episodes, dizziness with falls, altered mental status, dementia, impotence, constipation | Deficiency of anterior pituitary hormones | Sellar and suprasellar tumor with erosion of the left sellar floor | Large B-cell lymphoma | Surgery, a course of 4600 cGy conventional RT | Died shortly after RT |
| [12] | 65, M | Diplopia, right retrobulbar pain, low energy, and libido | Deficiency of anterior pituitary hormones | Sellar and suprasellar lesion extending into the right cavernous sinus with associated erosion of the sphenoid sinus. | High-grade, large B- cell lymphoma | Surgery, stereotactic radiosurgery and Codox-M of 4 cycles | Died 2 years later due to pulmonary failure |
| [15] | 86, F | Fever spikes, chills, night sweats, and weight loss | Partial deficiency of anterior pituitary hormones | Sellar mass within a slightly enlarged pituitary fossa | B-cell lymphoma | Surgery and CHT | Died 3 months following diagnosis |
| [13] | 41, F | Polyuria, polydipsia, amenorrhea syndrome and galactorrhea | Partial deficiency of anterior pituitary hormones Hyperprolactinemia | Intrasellar and suprasellar mass with thickening of the pituitary stalk and obstructive hydrocephalus | High-grade, large B-cell lymphoma | Surgery, RT (25 fractions of 200 cGy for a total dose of 5000 cGy) and intrathecal MTX | Symptom free for 7 months following management |
| [2] | 69, F | Right frontotemporal headache which developed later to right ptosis, diplopia, and III CN palsy | Hyperprolactinemia High IGF-1 Central hypothyroidism | Large sellar and suprasellar mass with sphenoid bone remodeling with optic chiasm compression and right cavernous sinus invasion | DLBCL | 4 cycles of MATRix regimen (methotrexate, cytarabine, thiotepa, and rituximab) | Died of sepsis 3 months later |
| [9] | 45, F | Headache, dizziness, unclear vision, bitemporal hemianopsia, ptosis, numbness of the face | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Heterogeneous sellar–suprasellar lesion with impingement on the optic nerves and chiasm, and involvement of the cavernous sinuses with thickening of the pituitary stalk | B-cell lymphoma | Surgery, CHT (MTX, vincristine, procarbazine and dexamethasone), R-ICE regimen and autologous transplant | Preserved neurological function 3 months postoperatively, with no signs of disease recurrence. |
| [4] | 61, F | Worsening headaches and acromegaly | High GHRH and IGF-1 Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Isointense, homogenously enhancing sellar tumor without evidence of pituitary stalk displacement | DLBCL, somatotroph hyperplasia | 3 cycles of R-CHOP with 3600 cGy of stereotactic RT and 180 cGy for 20 fractions within 27 days | No evidence of mass after 2 months of RT and normalization of prolactin and IGF-1 within 5 months |
| [10] | 37, M | Headaches and progression of visual acuity, bilateral blurred vision, and bitemporal hemianopia | No imbalances | Large intrasellar tumor with a widening of the sella turcica, extending backward into the anteropontal cisterns, which were narrowed, upward enclosing the hypothalamic infundibulum and optic chiasm, cavernous sinus, and sphenoidal involvement | Large B-cell lymphoma | Surgery, 6 cycles of CHOP (cyclophosphamide, vincristine, adriamycin, prednisone), whole-brain RT (dose of 40 Gy and boosted to the tumor 50 Gy) | Stable residual tumor and after 52 months of follow-up, the patient had a mild visual field defect in the right eye. |
| [11] | 59, F | Headache and diplopia | Hyperprolactinemia Partial deficiency of anterior pituitary hormones | Sellar mass extending to the suprasellar cistern and involving the pituitary stalk and cavernous sinuses | High-grade B-cell non-Hodgkin’s lymphoma | No management | Died before starting therapy |
| [14] | 71, F | CN VII palsy, bilateral temporal hemianopsia, syncopal spells, acromegaly | High GH and IGF-1 | Well-defined mass extending into the suprasellar cistern, compressing the optic chiasm, and penetrating right cavernous sinus | Large B-cell lymphoma, adenoma, and lymphocytic hypophysitis | Surgery and intensity-modulated RT at dose of 5040 cGy | Complete remission after 1 year of therapy |
| [5] | 73, F | Headache, double vision, retro-orbital pain | Diabetes insipidus | Sellar mass extending to the suprasellar cistern, cavernous sinus, and orbital apex with involvement of the optic chiasm and optic nerve | DLBCL | Surgery, R-CHOP, and high-dose MTX | Improvement after 15 months of RT |
| [7] | 67, F | Headache and left visual field defect | No imbalances | Pituitary mass extending downward to the sphenoid sinus | Diffuse, large, high-grade B-cell pituitary lymphoma | Surgery, stereotactic RT and CHT (4 cycles) | No recurrence after 15 months of follow-ups |
| [8] | 60, F | Weakness, headache, and ptosis | Partial deficiency of anterior pituitary hormones | Pituitary sellar mass extending into the suprasellar region, compressing the optic chiasm, and infiltrating the left cavernous sinus | DLBCL | Surgery, CHT with intraspinal MTX infusion, and R-MPV regimen | Died from hospital-acquired infection |
| Our case | 57, F | Headache, left eye lacrimation, blurry vision, temporal hemianopia, nausea, vomiting, and weight loss | Hyperprolactinemia | Large sellar and suprasellar mass, compressing the optic chiasm, and extending posteriorly toward the clivus with displacement of pituitary stalk | DLBCL | Surgery, rituximab and high-dose MTX which was replaced with nivolumab and whole-brain RT (total dose of 45 Gy over 25 fractions) | Clinically improved with a slight reduction in the mass size |
N/R, not reported; DLBCL, diffuse large B-cell lymphoma; RT, radiotherapy; CN, cranial nerve; CHT, chemotherapy; R-CHOP, rituximab-cyclophosphamide, vincristine, adriamycin, prednisone; R-ICE, rituximab, ifosfamide, carboplatin, etoposide; DeAngelis CHT protocol, methotrexate, vincristine, procarbazine, cytarabine; MTX, methotrexate; R-MPV, rituximab, methotrexate, vincristine, and procarvazine.
Clinical manifestations mainly featured neurological and ophthalmological complaints with headaches and visual abnormalities being the most common [1–11]. Several individuals indicated particular visual field impairments, such as bitemporal hemianopsia, diplopia, and ptosis [1, 2, 3, 5–12]. Involvement of cranial nerves, particularly third and fifth nerve palsies was frequently noted and observed along with retrobulbar pain [1, 2, 12]. Furthermore, some cases had weight loss, nausea, vomiting, polydipsia, polyuria, galactorrhea, and cognitive changes as their main presentation [3, 8, 12, 13].
Brain scans like MRI and CT demonstrated sellar or sellar–suprasellar masses of 1–5 cm extending into adjacent structures such as cavernous sinus, sphenoid sinus, or suprasellar cistern, leading to compression of the optic chiasm or hypothalamus [1, 2, 3, 7, 8, 13–15]. Additionally, certain cases featured isointensity or hypointensity on T1- and T2-weighted MRI sequences, accompanied with heterogeneous contrast, frequently resembling a mix of viable mass tissue or pituitary adenomas [1–3, 8, 10]. Certain patients displayed unique bilobed tumors causing hypothalamic compression, a hypermetabolic fludeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT). lesion invading the sphenoid sinus, or dumbbell-shaped masses eroding the sellar floor attributes more indicative of lymphoma [3, 6, 12]. Thickening of the pituitary stalk and invasion of cranial nerves were less common but signified an aggressive disease [11].
Management techniques differed according to the underlying pathology. The primary method to alleviate mass impact and obtain a histological diagnosis was trans-sphenoidal resection, performed using either endoscopic or microsurgical techniques [1, 5, 7–15]. Chemotherapy, including rituximab-cyclophosphamide, vincristine, adriamycin, prednisone (R-CHOP) and methotrexate-based protocols was the main treatment for pituitary lymphomas while radiation therapy (4600–5040 cGy) was used for residual disease [2–4, 6–12, 15]. Other care strategies were documented, including palliative radiation for patients declining aggressive treatment and high-dose glucocorticoids for suspected autoimmune hypophysitis [1, 3]. Furthermore, advanced therapies such as bone marrow transplantation were utilized in a patient with systemic lymphoma involvement [6].
The follow-up results of reported cases revealed a substantial variability. Certain patients achieved remission following chemotherapy and radiotherapy, although others experienced relapses needing salvage chemotherapy [1, 4, 7, 13]. Fatalities had been documented in several cases months after diagnosis [2, 3, 8, 11, 15]. Additionally, a few people needed hormone replacement therapy to treat their endocrine abnormalities [4, 12, 13]. The visual prognosis varied with certain patients attaining complete recovery, while others suffered persistent deficits [2, 10].
Conclusion
Our case underscores the importance of considering SSL, particularly in patients with unusual sellar masses. Persisting symptoms despite management for pituitary adenoma, accelerated tumor growth, and hormonal abnormalities necessitate detailed imaging and early biopsy. Effective treatment needs a multidisciplinary approach, integrating radiotherapy, and endocrine support when demanded. Early recognition of this rare entity is essential for optimal outcomes.
Conflict of interest statement
The authors declare no conflicts of interest.
Funding
No external funding was received for this study.



