-
PDF
- Split View
-
Views
-
Cite
Cite
Tarik Deflaoui, Anas Derkaoui, Haitam Soussan, Yassir Akil, Rihab Amara, Abdelali Guellil, Rachid Jabi, Mohammed Bouziane, Duplication of the common bile duct associated with dorsal pancreas agenesis: a diagnostic enigma and a major therapeutic turning point, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjaf029, https://doi.org/10.1093/jscr/rjaf029
Close - Share Icon Share
Abstract
We present a pioneering case of a duplication of the common bile duct associated with agenesis of the dorsal pancreas in a 66-year-old man. After an episode of cholestatic jaundice, radiological investigations revealed complex vascular and biliary anomalies, redefining the therapeutic strategy. Instead of risky surgery, endoscopic biliopancreatic drainage resolved the symptoms. This rare and complex case offers new perspectives for the management of such anomalies, underlining the importance of a personalized, multidisciplinary approach.
Introduction
Duplication of the main bile duct (DCBD) is a rare congenital anomaly characterized by complex anatomical variations and often associated with severe biliopancreatic complications if not recognized and managed appropriately [1]. The coexistence of this condition with anomalies such as dorsal pancreatic agenesis is exceptionally rare and raises unique diagnostic and therapeutic challenges [2]. This case underscores the importance of a thorough clinical and radiological assessment in the management of rare biliopancreatic malformations.
Case presentation
We report the case of a 66-year-old man presenting with right hypochondrium pain associated with cholestatic jaundice, suggestive of biliopancreatic obstruction. The initial work-up included an abdominal CT scan, which revealed a DCBD, associated with significant dilatation of both main ducts and choledochocele. A Roux-en-Y-shaped hepaticojejunostomy construction was initially considered as the gold standard treatment after multidisciplinary discussion (Fig. 1).
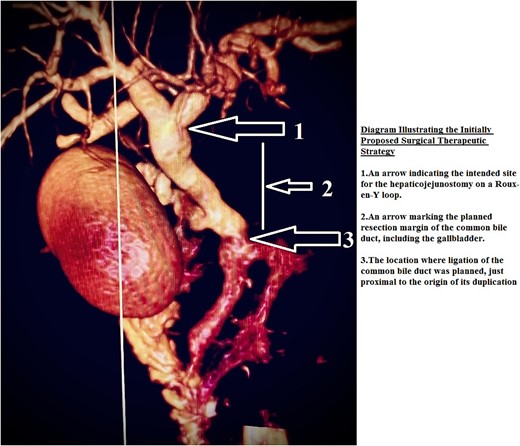
Diagram illustrating the initially proposed surgical therapeutic strategy.
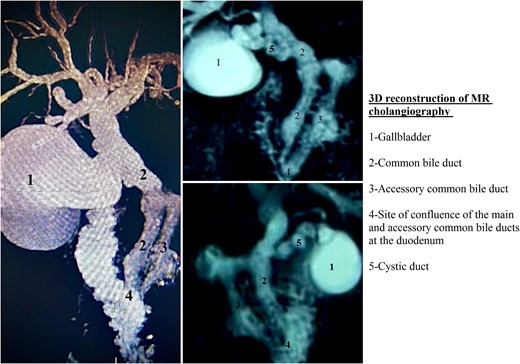
However, additional MRI (Fig. 2) revealed complex anatomical and vascular anomalies that significantly altered the therapeutic strategy: a complete atrophy of the dorsal pancreas, associated with chronic portal thrombosis complicated by a portal cavernoma with multiple peribiliary and intrahepatic shunts. These anomalies made Roux’s hepaticojejunostomy construction in Y risky, due to the complex vascularization and major hemorrhagic risk.
In view of this situation, endoscopic management was prioritized. A biliopancreatic drainage led to a quick clinical improvement, including resolution of jaundice and pruritus. At 6 months follow-up, the patient remained asymptomatic, with no recurrence of symptoms. However, due to the complexity of the vascular and biliary anomalies, close monitoring was decided for this patient to prevent any future complications.
Discussion
DCBD is an extremely rare congenital anomaly of the biliary system. First described by Boyden in 1932, it involves complex morphological variations in which an accessory bile duct may open in a region extending from the upper gastric minor curvature to the major duodenal papilla [3, 4]. These accessory ducts may or may not be connected to the draining system via the main papilla, complicating anatomical understanding and the very term “accessory” [5].
The classification of Goor and Ebert (Fig. 3), enriched by Saito et al., has clarified these anomalies according to their morphological characteristics. Type II, or bifurcation of the common bile duct, is one of the most studied variants, although it remains rare; it is also the variant that was present in our patient [6, 7].
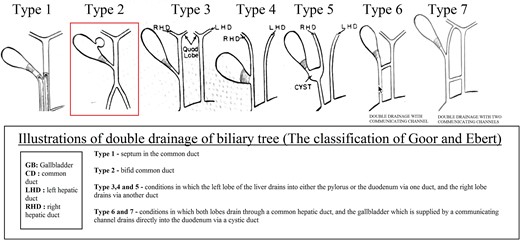
Illustrations of double drainage of biliary tree (the classification of Goor and Ebert).
Clinically, DCBD is often discovered in the context of inflammatory or obstructive complications. Manifestations include pancreatitis (10.6%), cholangitis (10.6%), cholecystitis (4.3%), and liver abscesses (2.1%). In addition, associated conditions such as biliary lithiasis (27.7%), choledocholith cysts (10.6%), pancreaticobiliary anomaly (PBM) (29.8%), and cancer (25.5%) add to the diagnostic and therapeutic complexity [8].
Biliary tract anomalies, although occasional, have been reported in cases of agenesis of the dorsal pancreas. However, the coexistence of a biliary duplication with this congenital anomaly is exceptional and deserves special attention, as it directly influences therapeutic strategy [2].
Diagnosis of DCBD and associated anomalies relies on advanced imaging modalities, such as ultrasonography, computed tomography, and magnetic resonance cholangiopancreatography. ERCP remains the gold standard for accurate assessment of these anomalies, although emerging techniques such as endoscopic ultrasound have recently shown great utility in differentiating complex congenital anomalies [9].
In the presence of DCBD, surgical management is often preferred to avoid long-term complications. Komi et al. reported a biliary carcinoma rate of 15.6% in adult cases, linked to chronic reflux of pancreatic juice into the bile ducts, justifying resection of the accessory bile duct as the treatment of choice. However, each case must be evaluated individually, especially in the presence of complex vascular or anatomical anomalies that may make surgery risky [10].
Conclusion
DCBD, although rare, presents significant diagnostic and therapeutic challenges, often necessitating surgical intervention to prevent severe complications. While endoscopic approaches may be effective in selected cases, surgery remains the gold standard for long-term management. Further research is essential to better define optimal treatment strategies and enhance clinical outcomes.
Conflict of interest statement
None declared.
Funding
This research received no external funding.
Data availability
The datasets and materials used in this study are available upon request.
Ethical approval
This study did not involve human or animal subjects and, therefore, ethical approval was not required.



