-
PDF
- Split View
-
Views
-
Cite
Cite
Kevin J Fuentes-Calvo, Francisco E Alvarez-Bautista, Oscar Santes, Renata De Nora-Jiménez, Luis F Arias-Ruíz, Noel Salgado-Nesme, Anal melanoma: a clinical challenge without therapeutic consensus, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjaf015, https://doi.org/10.1093/jscr/rjaf015
Close - Share Icon Share
Abstract
Anal melanoma is a rare malignancy, accounting for 0.4% to 1.6% of all melanomas. Its atypical presentation, low incidence, and non-specific symptoms make it a challenging diagnosis, which can lead to delayed treatment with an unfavorable impact on clinical outcomes. Treatment should be multidisciplinary and may include surgical resection with adjuvant therapy, chemotherapy, and radiotherapy. We present the case of a male patient who presented to the emergency department due to foreign body sensation and transanal bleeding. The patient underwent an anal exploration under anesthesia, where a hyperpigmented canal-dependent tumor lesion with extension into the perianal skin was found. After a wide local excision, histopathological study confirmed the diagnosis of invasive nodular melanoma. The patient was discharged without complications for follow-up and management in the outpatient medical oncology clinic.
Introduction
Anal melanoma, also known as anorectal melanoma, is a rare malignant neoplasm arising from the anorectal mucosa that accounts for ~0.4% to 1.6% of all malignant melanomas [1, 2]. The diagnosis of anal melanoma is often delayed, and the disease exhibits aggressive biological behavior, resulting in an unfavorable prognosis [3].
Case report
A 83-year-old man with a history of systemic arterial hypertension presented to the emergency department with transanal bleeding, foreign body sensation in the anal region, and unintentional weight loss of 5 kg in 3 months. The physical examination revealed a hyperpigmented and prolapsed lesion within the anal canal, accompanied by residual bleeding and hyperpigmentation extending to the anterior quadrants of the perianal skin. Considering the macroscopic characteristics of the lesion, a multidisciplinary team, comprising a colorectal surgeon, oncologist, and radiologist, was assembled for comprehensive evaluation and management.
A positron emission tomography (PET-CT) scan demonstrated heightened metabolic activity at the level of the anal canal, without evidence of suspicious lymph nodes or distant metastases (Fig. 1). Surgical exploration of the anal canal revealed a hyperpigmented tumor-like lesion originating from the anal canal and involving the anterior quadrants of the perianal skin (Fig. 2). Subsequently, a wide local excision of the lesion was performed (Fig. 3). Histopathological examination confirmed the diagnosis of a poorly differentiated invasive nodular melanoma, measuring 3.3 × 2.8 cm, with a Clark level of IV and a Breslow depth of 6 mm (Fig. 4). The patient experienced an uneventful postoperative course and was discharged for follow-up and immunotherapy management in the outpatient medical oncology clinic.
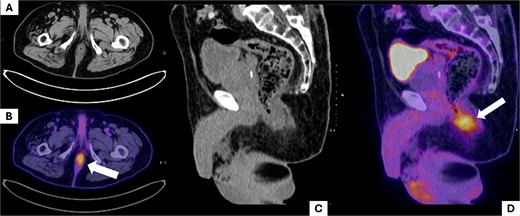
Positron emission tomography (PET-CT) scan. The images show the region corresponding to the anal canal. A and B show the affected anatomical region in axial slices. (A) Shows the anal canal with slight asymmetrical thickening predominantly on the left side, with no suspicious adenopathies; (B) shows uptake corresponding to the increase in local metabolism secondary to the tumor lesion (white arrow). C and D show sagittal slices of the pelvic region, where uptake is observed at the level of the anal canal (white arrow).
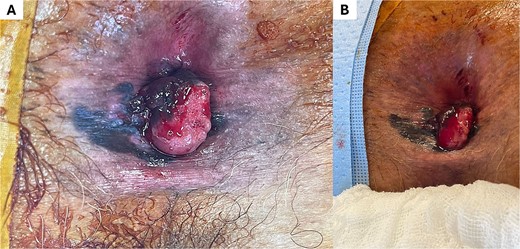
Lesion corresponding to anorectal melanoma. Observe in (A) and (B) the lesion with left lateral predominance, ulcerated surface, and irregular hyperpigmented borders.
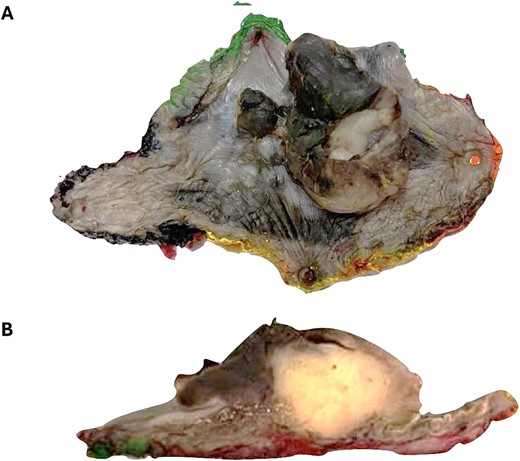
Wide local excision surgical specimen. (A) There is an exophytic tumor with irregular borders. (B) Nodular, submucosal, poorly demarcated tumor.
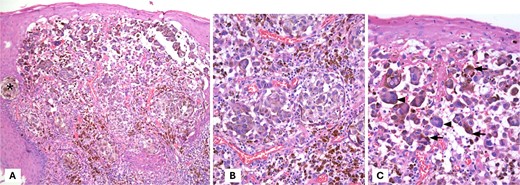
Hematoxylin and eosin staining. (A) Display of malignant neoplasm with solid growth pattern and forming nests (*). (B, C) At higher magnification, pleomorphic, polygonal cells with vesicular nuclei, prominent nucleolus, and abundant cytoplasm are observed. Note the pigment in the cytoplasm of the cells, which corresponds to melanin.
Discussion
Anorectal melanoma (AM) is a rare and aggressive mucosal melanocytic neoplasm that accounts for 1% of colorectal malignancies, < 0.5% of anal canal malignancies, and < 2% of melanomas. It represents the second most frequent subtype of mucosal melanoma after sinonasal melanoma [3, 4].
Anorectal melanoma predominantly affects individuals in the sixth to eighth decades of life, with a higher prevalence in women. The 5-year overall survival rates range from 14% to 30%, and the median overall survival is estimated to be between 9 and 19 months [5, 6]. Melanomas arise from melanocytes, which are found in the anal squamous zone and occasionally in the transition zone of the anorectal region. Malignant transformation of melanocytes in the anorectal mucosa is supposed to be associated with immunosuppression and oxidative stress [7].
Clinical presentation is often nonspecific, with symptoms such as transanal bleeding (84.9%), anal pain (68.7%), changes in bowel habits (28.5%), tenesmus (16.9%), and mucus secretion (6%) [3]. This nonspecific presentation can contribute to delayed diagnosis and increased potential for disease dissemination, accounting for the higher proportion of patients with regional or distant metastases at the time of diagnosis, compared to 11% observed in those with cutaneous melanomas [6]. Consequently, 7% to 20% of patients present with inguinal lymph node involvement at the time of anal melanoma diagnosis [4].
Surgery remains the cornerstone of treatment, with abdominoperineal resection (APR) and wide local excision (WLE) being the most commonly performed surgical interventions. In a recent meta-analysis of 303 patients, the 5-year overall survival rate was 23% for those undergoing APR and 32% for those undergoing WLE, with no statistically significant difference between the two groups. APR was associated with a local recurrence rate of 20.82%, while the recurrence rate after WLE was 47.04%. APR was associated with a significant reduction in local recurrence (OR 0.15, 95% CI 0.08–0.28, P < 0.00001) [8]. However, the patient’s general condition and disease stage should be considered when selecting the surgical approach, as APR carries a higher risk of morbidity. WLE may be considered for curative intent, as well as for palliation and improving the quality of life in cases where APR is not suitable [9, 10].
Currently, the role of adjuvant therapies, such as radiotherapy (including iliac and inguinal lymph node chains), chemotherapy, and immunotherapy, remains a subject of ongoing discussion. While these therapies may prolong disease-free survival, their impact on overall survival has not been definitively established [11, 12].
A multidisciplinary approach facilitates individualized treatment strategies based on the patient’s specific needs and clinical presentation. Further research is necessary to determine the true efficacy of emerging pharmacological therapies and their impact on survival, while carefully considering the potential for associated morbidity.
Conclusion
Anal melanoma is a rare and aggressive malignancy characterized by delayed diagnosis due to nonspecific symptoms and late presentation, resulting in advanced-stage detection and a poor prognosis. Surgical intervention remains the mainstay of anal melanoma management, and may be complemented by adjuvant therapies. Further research is warranted to evaluate the efficacy and impact of these novel therapies on survival outcomes.
Conflict of interest statement
None declared.
Funding
None declared.



