-
PDF
- Split View
-
Views
-
Cite
Cite
Liman Zhang, Jie Yang, Lili Wang, Tianpeng Zhang, Fei Ju, Yanjang Wu, Perianal abscess complicated by histiocytic necrotizing lymphadenitis postoperatively: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjaf007, https://doi.org/10.1093/jscr/rjaf007
Close - Share Icon Share
Abstract
Histiocytic necrotizing lymphadenitis (HNL) is a rare condition presenting with lymphadenopathy and fever. We report a case of a 61-year-old male with a history of perianal abscess surgery who developed HNL postoperatively. The patient was treated with corticosteroids, leading to resolution of fever and alleviation of symptoms. This case emphasizes the need for clinical vigilance for HNL in patients with a history of perianal abscess surgery and postoperative fever with lymph node enlargement.
Introduction
Histiocytic necrotizing lymphadenitis (HNL), also referred to as Kikuchi-Fujimoto’s disease, is a rare, benign, and self-limiting condition [1]. HNL often linked to viral infections like Epstein-Barr virus (EBV) and influenced by genetic and immune factors [2, 3]. Perianal abscess is an infection that affects the perianal and rectal spaces and typically results from bacterial pathogens. Surgical intervention is the primary modality for managing perianal abscesses. It carrying a risk of postoperative infection spread to inguinal lymph nodes, possibly leading to bacterial lymphadenitis and, in rare cases, necrotizing lymphadenitis. This case report describes a patient developing HNL post-perianal abscess surgery, highlighting the need for awareness in diagnosing and managing such complications.
Case report
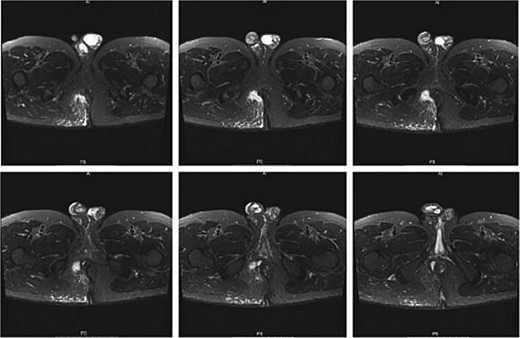
A 61-year-old male presented to our facility with a chief complaint of ‘perianal protruding mass and pain for 6 days.’ His medical history was unremarkable for hypertension, diabetes mellitus, and hematological disorders. Notably, the patient had a history of perianal abscess surgery 2 years prior to presentation. Perianal magnetic resonance imaging (MRI) findings indicated a high perianal abscess involving the right anal space, right ischiorectal fossa, and right gluteal flap, which was considered a new development. An old sinus tract in the posterior perianal space with fibrous tissue formation on the posterior wall of the anal canal was also observed, suggesting a correlation with the patient’s medical history (Fig. 1). Comprehensive laboratory assessments, including complete blood counts, liver function tests, renal function tests, coagulation profiles, electrolyte panels, infectious disease screenings, and electrocardiograms, were all within normal limits.
After confirming no surgical or anesthetic contraindications, the patient underwent incision and drainage for a complex perianal abscess surgery. Postoperatively, intravenous ampicillin sodium was administered. On the fifth day post-surgery, laboratory tests revealed: white blood cell (WBC) 9.8 × 109/L, neutrophils 68.4%, red blood cell (RBC) 4.98 × 1012/L, hemoglobin 152 g/L, platelets 186 × 109/L, and C-reactive protein (CRP) 10.4 mg/L. The wound showed signs of healing with patent drainage and granulation tissue, leading to the discontinuation of IV antibiotics in favor of standard wound care. On postoperative Day 13, the patient presented with fever (max 38.3°C), myalgia, malaise, and bilateral knee pain without respiratory or abdominal symptoms. A tender, 1 × 1.5 cm inguinal lymph node was noted. Labs showed: WBC 8.37 × 109/L, neutrophils 74.5%, lymphocytes 15.2%, RBC 4.53 × 1012/L, Hb 139 g/L, plts 162 × 109/L, CRP 16.3 mg/L. The anal wound was healing well. An external cold was suspected, and ibuprofen was given with a temporary fever reduction. On Day 14, the patient’s temperature was 37.1°C with improved myalgia but worsening knee pain, fatigue, oral ulcers, and abdominal papules with pustules (Fig. 2).

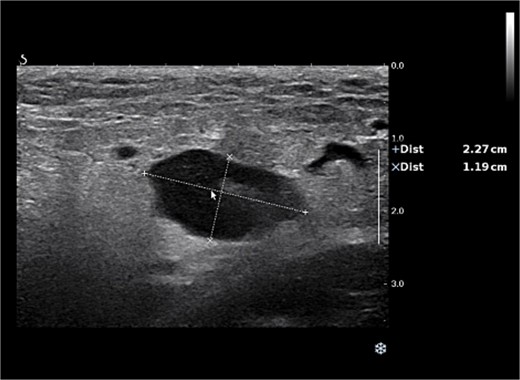
Examination revealed significant enlargement and tenderness of the right inguinal lymph node compared with previous assessments, while no other enlarged lymph nodes were palpated in regions such as behind the ear, under the jaw, under the clavicle, or in the left inguinal area. Measuring 23 × 12 mm on ultrasound, without abnormal blood flow on Color Doppler Flow Imaging (Fig. 3).
Empiric treatment with IV ampicillin and blood culture was initiated due to suspected lymph node inflammation. On Day 15, the patient’s symptoms worsened, with increased lymph node size to 2 × 4 cm, oral ulcers, and abdominal lesions. Labs showed leukocytosis with neutrophilia (white blood cells 10.74 × 109/L, neutrophil percentage 85.4%,) and elevated CRP (123.2 mg/L). Computed tomography (CT) scans revealed: (i) Local fibrous cord in the lower lobes of both lungs. (ii) Multiple small nodules in both lungs. (iii) Splenic enlargement. (iv) Possible inflammatory changes in the right pelvic and inguinal regions with multiple enlarged lymph nodes (Fig. 4).
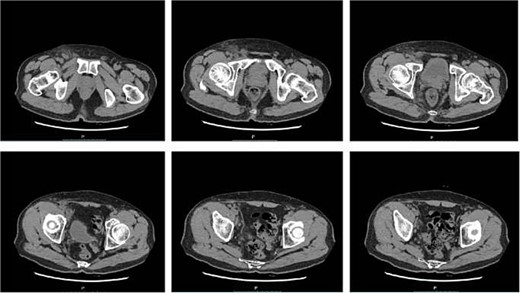
CT scans revealed inflammatory changes and enlarged lymph nodes in the right pelvic and inguinal regions, leading to a diagnosis of fever due to inguinal lymphadenitis. The antibiotic treatment was intensified to include IV cefoperazone sodium, sulbactam sodium, and metronidazole.On postoperative Day 16, the patient had persistent fever (37.3°C–38.7°C) and symptoms, with normal rheumatoid factor and immune panel but elevated erythrocyte sedimentation rate (ESR) (53 mm/H), IL-6 (164.95 pg/ml), and CRP (153.2 mg/L),and white blood cells, procalcitonin (PCT) were normal. Despite IV sulbactam sodium and metronidazole, fever persisted on day 20 (37.3°C–39.2°C), with worsening symptoms. Blood cultures were negative. On the 22nd postoperative day, the pathological report indicated destruction of the lymph node structure with visible coagulative necrotic foci and focal necrosis of histiocytes, which was consistent with necrotizing lymphadenitis. The patient was started on oral prednisone acetate (15 mg three times a day). After 5 days of treatment, the patient’s body temperature gradually returned to normal, the pain in the right inguinal lymph node subsided, its size decreased to 2 × 2 cm, the oral ulcers began to heal, and the abdominal papules and pustules resolved (Fig. 5).

The abdominal papules and pustules had disappeared on the 27th day following surgery.
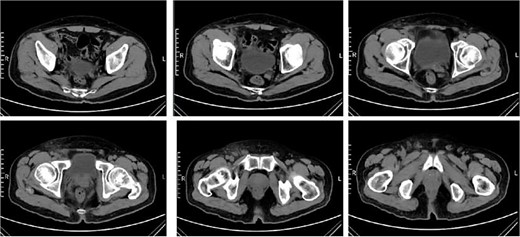
A follow-up complete blood count was normal and C-reactive protein 21.8 mg/L, PCT 0.09 ng/ml. CT re-examination indicated that the right inguinal lymph nodes had decreased in size (Fig. 6). Subsequently, the prednisone dosage was reduced by 5 mg every 7 days until discontinuation, with no further fever symptoms reported.
Discussion
HNL is predominantly observed in children and young women and is infrequent in the elderly [4], and is often misdiagnosed as conditions such as malignant lymphoma, lymphadenitis, tuberculous lymphadenitis, or systemic lupus erythematosus [5]. The primary symptom is lymph node enlargement, typically involving the cervical nodes, but it can also affect other regions such as the posterior auricular, inguinal, and mesenteric nodes. Most patients experience unexplained fever, which can be moderate to high, with atypical fever patterns lasting anywhere from one week to two months. Approximately one-third of the patients may develop rashes or papules on areas such as the head, face, chest, back, and limbs. Other symptoms can include fatigue, joint pain, muscle soreness, and splenomegaly. Laboratory findings may show normal or decreased white blood cell counts, an accelerated erythrocyte sedimentation rate, and elevated C-reactive protein levels, with potential manifestations of anemia and thrombocytopenia [6–9]. In the presented case, an elderly male with high fever and right inguinal lymph node enlargement was initially suspected to have an infection causing acute lymphadenitis, following perianal abscess surgery. Negative rheumatoid factor, immune panel, and anti-cyclic citrullinated peptide (anti-CCP) antibody results ruled out rheumatological fever causes. Symptoms, such as joint pain, muscle soreness, general weakness, and oral ulcers, were mistakenly attributed to fever, leading to continued antibiotic treatment.
Diagnosis of HNL is confirmed through lymph node biopsy, which reveals lymph node architecture destruction, coagulative necrosis, and karyorrhexis in histiocytes [10]. Initially misdiagnosed with acute lymphadenitis post-surgery, the patient showed normal PCT levels after ineffective anti-infective treatment, indicating a non-bacterial cause. Thus, we relied on a lymph node biopsy to confirm the diagnosis. In treating HNL, the condition is typically self-limiting, with many cases spontaneously resolving. Therefore, management is primarily
symptomatic and involves antipyretics and analgesics. However, the patient’s laboratory results showed an accelerated erythrocyte sedimentation rate, significantly elevated CRP level, and anemia, indicating a more severe condition [11]. Consequently, glucocorticoids were administered, resulting in the normalization of body temperature, reduction in lymph node size, and significant relief of symptoms.
HNL’s etiology is often linked to viral infections and autoimmune reactions [12]. In this case, HNL onset followed perianal abscess surgery by 10 days, suggesting a possible postoperative infection-related trigger. However, a direct causal link between infection and HNL remains unproven [13].Our findings contribute to the evolving understanding of HNL, which may be secondary to severe infections and excessive cytokine release [14].
This manuscript presents a case of a perianal abscess patient who developed necrotizing lymphadenitis postoperatively, suggesting a potential link between infection and the development of necrotizing lymphadenitis. The delayed early diagnosis due to the rarity of HNL underscores the necessity for heightened clinical vigilance. Close monitoring and timely examination are essential for early diagnosis and treatment in patients presenting with fever and lymph node enlargement following perianal abscess surgery.
Acknowledgements
The authors gratefully acknowledge the invaluable support provided by the Medical Records Department of Shijiazhuang Traditional Chinese Medicine Hospital in supplying case data.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.



