-
PDF
- Split View
-
Views
-
Cite
Cite
Peter R Bael, Bayan F Alqtishat, Riyad Salahaldeen, Wadee’ Barbarawi, Complete traumatic urethral cut and vesicovaginal fistula in a 3-year-old girl, managed by Mitrofanoff procedure: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjaf004, https://doi.org/10.1093/jscr/rjaf004
Close - Share Icon Share
Abstract
We report a 3-year-old patient with urethral cut injury and iatrogenic vesicovaginal fistula following a pelvic fracture; managed with Mitrofanoff procedure. Our patient presented with straining on urination with continuous colorless discharge on her diaper for the past 4 months. Investigations identified vesicovaginal fistulization making a definitive diagnosis of complete urethral injury. It was managed with the Mitrofanoff procedure to preserve the patient’s urinary continence. Our case is to our knowledge the youngest reported case of a complete traumatic urethral cut in a female; an already rare encounter in this population. This is also the first such case to be managed via the Mitrofanoff procedure. Although the management was delayed, it was successful.
Introduction
Female urethral injuries (UI) rarely sequel pelvic fractures, occurring in 0.15% of females as opposed to 1.54% of males. The isolation in cases in females makes management a true dilemma [1, 2]. Complete urethral cuts (CUC) are the boogie man of UI with only a handful of cases reported [1]. The prognosis is further worsened with concomitant bladder neck blunting and fistulization, which renders urethral catheterization ineffective [2–4].
Vesicovaginal fistulas (VVFs) are abnormal communications between the bladder and vagina. They seldom occur in children, especially in the context of trauma, comprising 6% of cases. VVFs usually present with continuous urine leakage, and involve a variety of locations in the bladder. The Mitrofanoff procedure or appendicovesicotomy is a surgical procedure that reconstitutes continence through catheterizing a stoma in the umbilicus [5–8].
In this case, we report a female pediatric patient with a traumatic CUC causing a blind-ended bladder neck injury complicated by an iatrogenic VVF, managed through the Mitrofanoff procedure. This case was reported in accordance with the SCARE checklist [9].
Case report/case presentation
A 3-year-old girl was referred to our center with her parents reporting straining on urination with continuous colorless discharge from the vagina for the past 4 months.
The patient’s history started when she sustained a pelvic fracture after falling down from the sofa while playing. She was promptly admitted to a local hospital for evaluation and management. Her parents reported that since the fall she hadn’t urinated and they had seen blood in her diaper. Under high suspicion of UI, she was catheterized suprapubically and underwent exploratory cystoscopy confirming the UI. Primary realignment was done via a urethral catheter, and the patient was discharged.
The urethral catheter was removed 2 months later following which she could no longer void. Hence, a catheter line was re-established.
Subsequently, the patient was referred to our hospital for higher-level management. All her admissions were further complicated by recurrent urinary tract infections (UTI), which were managed with IV antibiotics.
Her first admission was following her referral as a case of UI. She had no significant findings on examination, nor her growth, developmental and family histories. She has no known drug allergies and takes no regular medications.
After initial pain management, the patient underwent several assessments while in a supine position.
A renal ultrasound was unremarkable. A cystogram showed no fistulization, extravasation of contrast, nor leakage into the urethra.
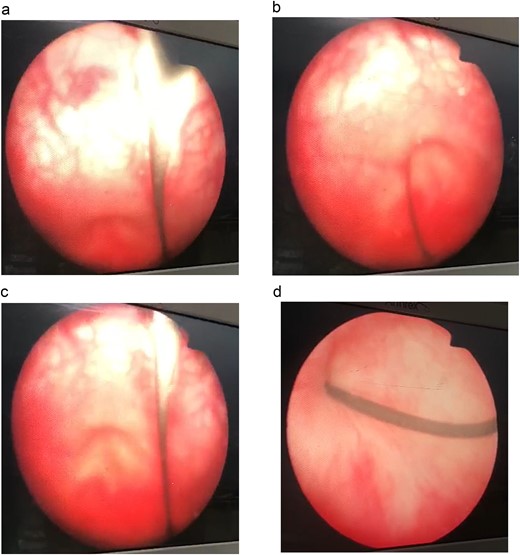
Antegrade and retrograde cystoscopy revealed a damaged urethra and cystitis (Fig. 1). The cystoscope passed smoothly through the suprapubic site, though it was difficult to navigate the urethra.
Before discharge, the patient’s suprapubic catheter was clamped and her urethral catheter was removed. She seemed to void normally. After 1 day of observation, the patient was discharged.
A total of 2 days after initial discharge, the patient no longer voided normally, the suprapubic catheter was unclamped and a urethral catheter was reinserted.
The patient was readmitted for re-evaluation and management. On physical examination, there was vaginal discharge, presumably urine leakage. Flexible antegrade cystoscopy via the suprapubic catheter, in lithotomy position, initially failed to pass to the urethra. Thus a guide wire was inserted through the bladder open passage and was followed into the vagina through a false patent tract; confirming the diagnosis of a VVF with a blind-ended bladder. The fistula was seen to spontaneously divert, convincing us against fistula closure.
We decided to manage her with a Mitrofanoff procedure.
She was readmitted in to undergo an appendicovesicostomy via the Mitrofanoff procedure. After the routine admission workup, she was prepared for surgery.
The patient underwent surgery under general anesthesia in a supine position. A midline incision was made from below the umbilicus to the symphysis pubis. Subcutaneous tissue was incised, exposing the rectus abdominis aponeurosis. An incision was made at the linea alba, and the rectus abdominis muscles were retracted laterally. The cecum was identified in the right lower quadrant and carefully dissected to reveal the appendix. It was extracted with a cecum cuff while preserving the appendiceal mesentery.
The bladder was opened anteriorly, and a submucosal tunnel was made to implant the distal end of the appendix and its mesentery, while expanding the bladder. The cecal end of the appendix was sewn to a point below the umbilicus as a catheterizable stoma. At this point, a suprapubic catheter was inserted. Prior to closure, we irrigated theedges to ensure watertight repair. The skin was then repaired and the operational site was dressed.
Her post-operative course was unremarkable. An evaluatory X-ray 3 days post-op revealed good outcomes (Fig. 2).

Following the procedure, the patient was healthy. Her parents were instructed on how to maintain the cleanliness of the stoma and how to insert a catheter to allow the patient to void through it via clean intermittent catheterization. She was continent and her urine was clear. She was discharged a week following the procedure. The patient’s parents reported no complaints on follow-up. The patient seemed healthy and prosperous.
Discussion
The predominance of male-UI is attributed to the shorter female urethra and its lack of ligamentous connections to the pelvis, necessitating more severe injury to damage the urethra [1–4]. On the other hand, UI is more likely in children after falls, possibly due to the elevated placement of the bladder [1, 2]. Ultimately, UI remains rarer and more severe in females, regardless of age, while endangering continence [4].
Though immediate and delayed repairs are deemed equally more effective than primary alignment, delayed repair carries higher risks, notably incontinence. It is also more complex in females due to anatomical differences [1, 2].
The most likely factors behind delayed repair are late presentation or delayed diagnosis. Unfortunately, in these cases—which comprise around half of all reported cases—this approach carries the risks of vaginal stenosis, dense scarring, and further fistulization which complicates management and morbidifies outcomes. A delayed urethral repair can prompt or be required by concomitant VVF possibly due to pelvic fractures [1–3].
Beyond her late presentation with a CUC and a VVF, she’s also the youngest reported case for either presentation [1–3, 5, 6].
The Mitrofanoff procedure was preferred over delayed repair to avoid the associated debilitating complications. The Mitrofanoff procedure also offered direct insurance of continence, our main therapeutic goal [1–3, 5–8].
Author contributions
Study concept and design: All authors, Data acquisition: RS, WB, Data analysis: All authors, Drafting of manuscript: PB, BA. Critical revision of the manuscript: All authors.
Conflict of interest statement
We declare no competing interest.
Funding
The authors didn’t receive any external funding.
Data availability
Not applicable.
Declarations
Ethics approval and consent to participate: Our ethics committee doesn’t require ethical approval for case reports, except for written consent of the patient, which was taken.
Consent for publication
The patient’s parents consented to the publication of this manuscript.



