-
PDF
- Split View
-
Views
-
Cite
Cite
Nyoman Golden, Steven Awyono, Christopher Lauren, Dicky T Prakoso, Intracranial neurenteric cyst in the cerebellopontine angle: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae840, https://doi.org/10.1093/jscr/rjae840
Close - Share Icon Share
Abstract
Neurenteric cysts, rare benign tumors, are most often found in the cervical or thoracic spinal cord, with intracranial occurrences being extremely uncommon. This case report describes a 52-year-old female with a neurenteric cyst in the cerebellopontine angle, presenting with headaches and balance disturbances. Magnetic resonance imaging (MRI) revealed a cystic lesion causing hydrocephalus, and surgical removal was performed using a retrosigmoid approach. Histopathological analysis confirmed the cyst as Type A neurenteric, characterized by ciliated columnar epithelium and goblet cells. Postoperatively, the patient showed significant improvement with resolved symptoms. Neurenteric cysts can mimic other cystic lesions radiologically, complicating diagnosis. Management typically involves surgical excision, although complete removal is often challenging due to cyst adherence to nearby structures. Recurrence rates remain high, necessitating long-term follow-up. This case highlights the importance of differential diagnosis and careful surgical planning in managing neurenteric cysts to optimize patient outcomes.
Introduction
Neurenteric cysts, first identified by Puusepp in 1934, are benign tumors that can develop along the central neuraxis, with a significantly higher occurrence in the cervical or thoracic spinal cord compared to the rare intracranial cases, which account for only ⁓0.01% of all central nervous system tumors [1–3]. Intracranial neurenteric cysts are most commonly found in the posterior fossa, particularly at the midline in front of the brainstem or near the cerebellopontine angle, with even rarer occurrences on the supratentorial region [4]. The pathophysiology of these cysts remains unclear, though theories suggest origins related to the neurenteric canal or Seesel's pouch during embryonic development [1, 2]. This case report presents an intriguing case of a 52-year-old female patient diagnosed with a neurenteric cyst in the cerebellopontine angle. We provide a detailed discussion of the patient's medical history, physical and auxiliary examinations, surgical procedure, histopathological findings, outcomes, and a literature-based discussion of this case.
Case report
History
A 52-year-old woman presented to the neurosurgery clinic with a complaint of headaches that felt throughout the head, which had persisted for the past three months and worsened significantly over the past week. She had been taking over-the-counter pain medication, which provided only temporary relief. Additionally, she reported a balance disorder that had been present for the past 2 weeks. She denied any loss of consciousness, nausea, vomiting, visual disturbances, hearing loss, swallowing difficulties, weakness on one side of her body, or sensory disturbances. There was no previous history of tumors or similar family history. She had the same complaints 1 year before and underwent tumor removal.
Examination
We found the patient with a visual analog scale of 8/10 on the physical examination. The Romberg test was positive on the left side, while other neurological examinations were within normal limits. A magnetic resonance imaging (MRI) of the head revealed an extra-axial cystic lesion in the left cerebellopontine angle (Fig. 1), compressing the left cerebellar hemisphere posteriorly, displacing the pons to the right, narrowing and displacing the fourth ventricle to the right, causing non-communicating hydrocephalus. We then planned surgery with a retrosigmoid approach to remove the cyst wall and decompress the brainstem.
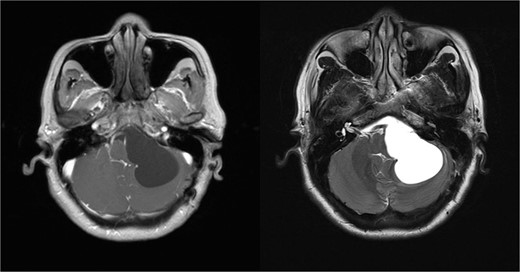
MRI examination reveals an extra-axial cystic lesion appearing dark on T1-weighted images and bright on T2-weighted images.
Operative procedure
The patient lay in a park bench position, and a C-shaped incision was used to expose the retromastoid region. We open the bone flap and perform additional drilling toward the transverse and sigmoid sinus, followed by a dural incision from the inferior segment and cisternostomy on the left lateral medullary cistern. We carefully identified the cystic wall, which is very adherent to surrounding structures (Fig. 2A). First, we encountered severe adherence from the cystic wall on the facial nerve; we removed the cystic wall to decompress the nerve, and further arachnoidal dissection to the deep structure to expose the trigeminal nerve (Fig. 2B). The lower border of the cyst around the lower cranial nerve and the vertebrobasilar complex is identified, and then the wall is carefully dissected to decompress the neural structures (Fig. 2C and D). We intentionally left a piece of the wall attached tightly to the adjacent structures to prevent post-operative complications. After carefully dissecting and removing the wall, we closed the dura using dural synthetic material, and the bone flap was placed back.
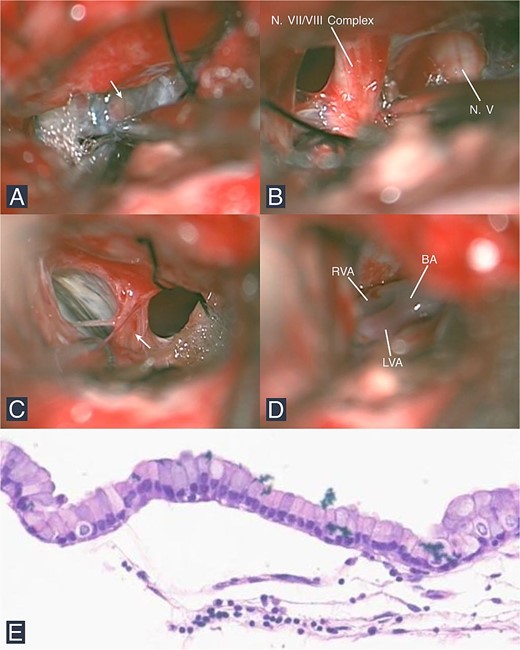
Intraoperative and histopathological findings. (A) The cyst wall is seen adhering to the arachnoid layer in the CPA (arrow). (B) During dissection, the N. VII/VIII complex and N. V are visualized. Structures observed include (C) the lower cranial nerves with the arachnoid and cyst wall (arrow) and (D) the vertebrobasilar junction. (E) Microscopic examination shows a columnar epithelium with goblet cells (HE stain; 100× magnification). (Abbreviations: CPA: Cerebellopontine angle, N: Nerve, V: Trigeminal, VII: Facial, VIII: Vestibulocochlear, RVA: Right vertebral artery, LVA: Left vertebral artery, BA: Basilar artery, HE: Hematoxylin and eosin stain).
Histopathological findings
Examination revealed a thin tumor wall, with microscopic features showing that the cyst wall consisted of fibrous connective tissue lined by a single layer of ciliated columnar epithelium and goblet cells (Fig. 2E). These histopathological features are characteristic of a neurenteric cyst.
Post-operative care and follow-up
The patient was hospitalized for five days, during which her headaches improved, and no neurological deficits were observed. During the third month of the post-operative visit, she had no complaints and could perform daily activities without any issues. Her headache and balance disturbance already resolved without any other neurological deficit. We decided to continue regular follow-up appointments, including MRI scans, every 6 months.
Discussion
Neurenteric cysts, also known as enterogenous cysts, were first identified by Puuseep in 1934 [2]. These benign tumors can develop along the central neuraxis. The predilection for this tumor is three times higher in the cervical or thoracic spinal medulla compared to intracranial findings, which are rare, with a prevalence of only ⁓0.01% of all central nervous system tumors [2, 5]. Intracranial neurenteric cysts are most commonly found in the posterior fossa, typically at the midline in front of the brainstem or around the cerebellopontine angle [4]. Supratentorial occurrences are even rarer.
The pathophysiology of neurenteric cysts remains uncertain. One theory suggests that these cysts develop during notochord development due to the transient presence of the neurenteric canal. Failure of the notochord and foregut to separate during escalation leads to the integration of primitive endodermal cells into the notochord. These displaced digestive tissues eventually form cysts. Another theory posits that Seesel's pouch, an endodermal diverticulum found behind the oropharyngeal membrane, might be the embryological progenitor of midline supratentorial cysts. However, neither theory fully explains the development of cysts [1, 2, 5].
Patients often present with complaints related to focal neurological deficits caused by the mass effect of the cyst on surrounding areas [5–7]. Symptoms can range from cranial nerve deficits to myelopathy and signs of meningitis due to the leakage of cyst contents. In our patient, there was a balance disorder confirmed by a positive Romberg test, along with chronic headaches experienced over the past 3 months. These symptoms are associated with progressively increasing intracranial pressure.
Radiologically, neurenteric cysts typically appear as extra-axial masses on the midline of the posterior fossa. Computed tomography (CT) scans usually show hypodense lesions. On MRI, signal intensity depends on the protein content of the cyst fluid. In cases with high protein content, the cysts appear isointense or slightly hyperintense on T1-weighted images compared to cerebrospinal fluid and are usually very hyperintense on T2-weighted images [1, 5, 8]. Neurenteric lobulated cysts do not enhance with contrast, mostly ˂2 cm without calcification. Hydrocephalus may occur if the cyst obstructs the cerebrospinal fluid outflow on the fourth ventricle level. Due to nonspecific radiological features, the differential diagnosis for neurenteric cysts is very wide, including arachnoid cysts, choroid plexus cysts, colloid cysts, dermoid cysts, epidermoid cysts, primary or metastatic cystic tumors, and Rathke's cleft cysts [1, 9]. In our case, the lesion was suspected to be an arachnoid cyst due to its similar radiological appearance and location in the cerebellopontine angle (CPA) region.
Histopathologically, neurenteric cysts are classified into three types [2]. Type A is characterized by an epithelial lining similar to respiratory or gastrointestinal epithelium, composed of single or pseudostratified cuboidal or columnar cells, with or without cilia. Type B includes additional connective tissue components such as smooth muscle, lymphoid tissue, and occasionally nerve ganglia. Type C is akin to Type B but also contains glial components. Neurenteric cysts are differentiated from neuroepithelial cysts by the presence of a basement membrane, cilia, and goblet cells with secretory glands. The patient we report in this case presented with a neurenteric cyst exhibiting the histopathological features of Type A.
Currently, the management of symptomatic neurenteric cysts involves surgical excision. Total resection is recommended to reduce recurrence rates [2, 10]. However, total resection may be challenging due to the adherence of the cyst walls to surrounding critical structures, leading to partial resection or biopsy in some cases. Recurrence can occur even after total resection, with rates reported between 11.9% and 37% and recurrence times ranging from 4 months to 14 years postoperatively [2, 5]. Given the variable recurrence rates, periodic follow-up for at least 10 years post-surgery is advised.
Conflict of interest statement
None declared.
Funding
None declared.



