-
PDF
- Split View
-
Views
-
Cite
Cite
Shunhua Tian, Feng Wu, Fan Yang, Guilin Min, Hongliu Chen, Laparoscopic surgery for synchronous double colorectal cancer with obstruction, plus small B cell lymphoma: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae830, https://doi.org/10.1093/jscr/rjae830
Close - Share Icon Share
Abstract
Synchronous colorectal cancer is a rare disease. It remains challenging for diagnosis and treatment. This paper reports a case of a 75-year-old Chinese male patient presenting with intestinal obstruction, alongside primary thrombocytopenia and a diagnosis of small B-cell lymphoma. Computed tomography scans revealed space-occupying lesions in both the sigmoid colon and ascending colon. The patient initially underwent a transverse colostomy procedure to alleviate the intestinal obstruction and then underwent laparoscopic radical tumor resection. The patient exhibited favorable prognosis and maintained satisfactory bowel function at the nearly 8 months’ postoperative follow-up. Multiple colonoscopies are crucial in the management of synchronous colorectal cancer, and radical surgical resection remains the sole curative option when surgical intervention is deemed tolerable. A thorough preoperative examination and evaluation are crucial for successful surgery. The selection of surgical procedures for synchronous colorectal cancer should be based on the patient’s medical condition.
Introduction
Synchronous colorectal cancer (sCRC) is diagnosed when two or more primary colorectal lesions are identified simultaneously or within 6 months of the initial diagnosis [1].Although colorectal cancer is one of the most common malignancies worldwide, sCRC is not common, with an incidence rate of about 1%–8% [2–4]. In recent years, advancements in imaging and diagnostic tools have led to a more nuanced understanding of sCRC. Risk factors for sCRC include advanced age, being male, hypertension, cirrhosis, genetic susceptibility to familial adenomatous polyposis (FAP), hereditary non-polyposis colorectal cancer (HNPCC), and ulcerative colitis [1, 5, 6].
Radical surgical resection remains the cornerstone of treatment for sCRC. However, the optimal surgical approach remains a continuing controversy [7]. This study presents the case of a 75-year-old male patient diagnosed with tumors in both the sigmoid and ascending colon, accompanied by primary thrombocytopenia and small B-cell lymphoma. Due to partial obstruction caused by a malignant tumor in the sigmoid colon, the patient was admitted to the hospital and underwent an emergency colonoscopy examination. Unfortunately, intestinal stenting failed due to complete obstruction of the sigmoid colon. Following this, the patient underwent an emergency transverse colostomy. Subsequently, a laparoscopic sigmoid tumor resection and right hemicolectomy were performed. The report adhered to the guidelines of the surgical case report (SCARE) 2020 [8].
Case report
A 75-year-old male patient was admitted to the Department of Hematology due to small B-cell lymphoma. The patient had been experiencing incomplete intestinal obstruction for nearly 1 year and had been self-medicating with diarrhea-inducing medication obtained outside the hospital. During hospitalization, the patient exhibited a marked decline in appetite, accompanied by cessation of bowel movements, nausea, and vomiting. The patient weighed 85 kg, stood at 1.68 m tall, and had a body mass index of 30.12 kg/m2. He had no history of smoking, alcohol consumption, or surgery. Physical examination: the patient’s body temperature, heart rate, and blood pressure were normal, with abdominal distension, scattered abdominal tenderness without obvious rebound pain, and drumming sound on abdominal percussion. Laboratory tests: platelets, tumor markers CEA, the rest showed no abnormality. Chest computed tomography (CT) showed a few infection foci in the lungs, with no metastatic foci observed. Enhanced CT scanning of the abdomen revealed tumors in the sigmoid and ascending colon, with significant thickening observed in the proximal sigmoid colon tumor (Fig. 1). Colonoscopy revealed complete obstruction of the sigmoid colon (Fig. 2).
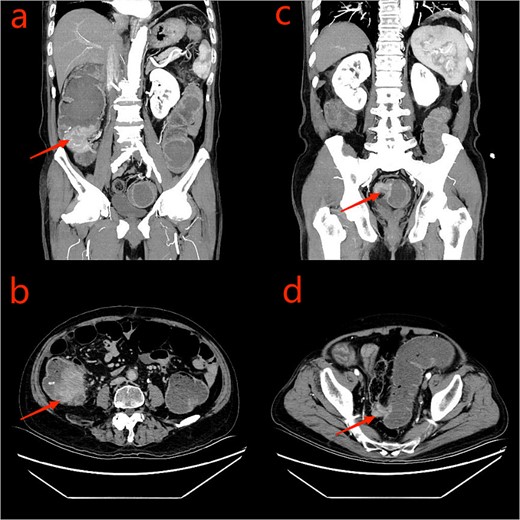
CT scan of the abdomen and pelvis: a: ascending colon tumor (coronal scan); b: cecum tumor (axial scan); c: sigmoid tumor (coronal scan); d: sigmoid tumor (axial scan).
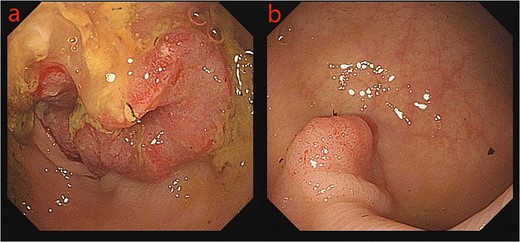
The patient was referred to the Department of Gastrointestinal Surgery. After electronic colonoscopy showed a neoplasm located 65 cm from the anus, biopsy confirmed it as adenocarcinoma. Placement of a tumor stent was unsuccessful due to complete bowel obstruction. Given the patient’s comorbid small B-cell lymphoma and our inability to ascertain the nature of the ascending colon tumor, emergency surgery was performed, specifically, a transverse colostomy was executed.
Given the patient’s unsuitability for immediate radical surgical resection, the patient was administered monotherapy with capecitabine to control tumor progression. During an outpatient follow-up, a slight enlargement of the tumor was observed in the ascending colon region. To further understand the patient’s condition, he was readmitted to the hospital, to undergo laboratory tests, serum CEA: 26.10 ng/ml, uric acid: 447 umol/L, and platelet levels were normal. Repeated enhanced CT scanning of the abdomen revealed complete recovery from the obstruction (Fig. 3). To ascertain the nature of the ascending colon tumor,a repeat colonoscopy examination through colostomy showed the sigmoid and ascending colon tumor. The biopsy of the ascending colon tumor revealed an adenocarcinoma (Fig. 4). Given the patient’s concomitant small B-cell lymphoma and primary thrombocytopenia, surgical treatment was decided after a multi-disciplinary team discussion.
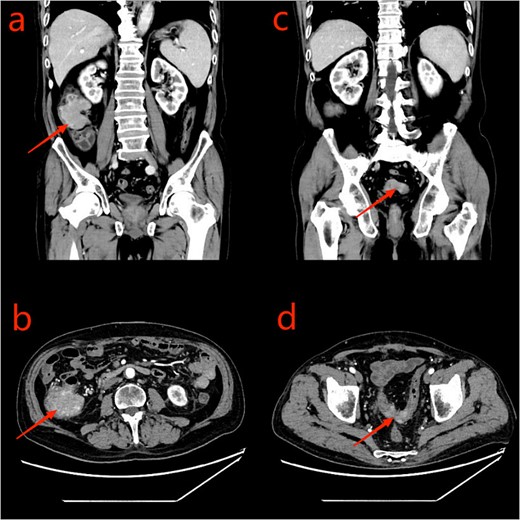
CT scan of the abdomen and pelvis: a and b: ascending colon tumor; c and d: sigmoid tumor.
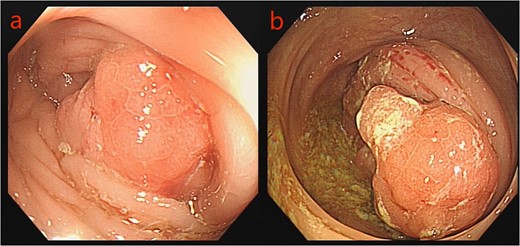
Colonoscopy images: a: sigmoid tumor; b: ascending colon tumor.
The patient underwent laparoscopic surgery. Firstly, we closed the transverse colostomy and inserted a single-port laparoscopic instrument in the stoma. Exploration revealed a tumor in the ascending colon region, ~5 cm in size. Additionally, the sigmoid colon tumor descended into the pelvis due to sigmoid colon redundancy and formed adhesions with the surrounding tissues. No metastatic tumors were found in the liver or abdominal cavity. Subsequently, laparoscopic radical sigmoidectomy and radical right hemicolectomy for sigmoid colon cancer were performed (Fig. 5). Side-to-side anastomosis was performed for the sigmoid colon and side-to-end anastomosis was performed for the ileum. Surgical duration was 420 min, with intraoperative bleeding was about 150 ml. Postoperative pathology was confirmed of adenocarcinoma in all cases: tumor size (sigmoid tumor: 2.8 × 2.5 × 1.5 cm, ascending colon tumor: 6.0 × 5.0 × 3.5 cm); pathological stage (sigmoid tumor: T3, ascending colon tumor: T3). A total of 24 lymph nodes (sigmoid tumor: 8, ascending colon tumor: 16) were detected, and no lymph node metastasis was found. The tumors were also microsatellite stability tumors. KRAS mutations were also not detected. Finally, there were no known genetic predispositions to colon cancer, including FAP or HNPCC. The patient experienced anal exhaustion on the third postoperative day. The patient was able to tolerate a liquid diet starting from the seventh day postoperatively. After satisfactory recovery, the patient was discharged from the hospital on the 22nd postoperative day.
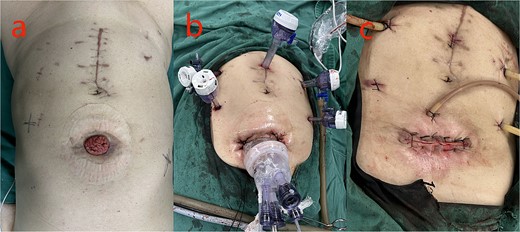
Pictures of the surgery: a: preoperative; b: intraoperative; c: postoperative.
Discussion
As a rare disease, the diagnosis and treatment of sCRC is still challenging. Preoperative diagnosis will directly affect the choice of surgical approach and other treatment decisions, and any missed diagnosis will probably lead to secondary surgery and tumor progression and metastasis. In this case, the patient had a combination of intestinal obstruction and small B-cell lymphoma at the initial consultation. Cases of synchronous colorectal adenocarcinoma and intestinal lymphoma have been previously reported in the literature [9, 10]. We could not clarify the tumor pathology in the ascending colon tumor region at the time of initial treatment, so we chose a transverse colostomy to relieve the obstruction, and radical tumor surgery in the second stage. Concerning the extent of surgical resection, some scholars believe that a total or subtotal colonic resection is recommended so that any underlying tumor or adenoma can be removed, whereas a multi-segmental resection anastomosis will inevitably lead to an increased chance of an anastomotic fistula [11, 12]. Other scholars have suggested that regional resection is recommended because extensive resection will likely result in increased bowel movements after surgery, and preservation of the normal colon is important for the patient’s postoperative quality of life [13]. Although some studies have pointed out that the intestinal mucosa of sCRC patients is unstable, and the residual intestinal tubes or adenomas may recur after surgery, the process of adenomas developing into adenocarcinomas takes several years [14]. During this process, we can clarify the diagnosis and treatment through follow-up and colonoscopy. In this case, our team chose the right hemicolectomy plus sigmoid resection. At a recent follow-up, the patient had about one bowel movement 1 day. In patients with sCRC without genetic predisposition, surgeons should comprehensively evaluate the patient’s general condition, the location and number of tumors, the presence or absence of other colorectal diseases, and the adequacy of the preoperative examination when choosing the surgical method [11, 15].
sCRC has a higher mortality rate than isolated tumors, and the combination of obstructive symptoms tends to complicate the diagnosis [16]. Therefore, adequate preoperative diagnosis is the basis for the treatment of sCRC. For sCRC patients with concurrent lymphoma, it is crucial to devise a precise and individualized treatment plan through detailed preoperative evaluations and multidisciplinary consultations.
Author contributions
Dr. Shunhua Tian: the conception and design of the study, analysis and interpretation of data, drafting the article, and final approval of the version to be submitted.
Mr. Feng Wu: critical revision for important intellectual content, and final approval of the version to be submitted.
Dr. Fan Yang: critical revision for important intellectual content, and final approval of the version to be submitted.
Dr. Guilin Min: critical revision for important intellectual content, and final approval of the version to be submitted.
Dr. Hongliu Chen: critical revision for important intellectual content, and final approval of the version to be submitted.
Dr. Shunhua Tian, Mr. Feng Wu, Dr. Guilin Min (assistants), and Dr. Hongliu Chen (surgeon) performed the laparoscopic surgery.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Funding
This research received no external funding.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during this study.
Ethical approval
Ethical approval is exempt/waived at the ethical committee team in Minda Hospital of Hubei Minzu University, Enshi, China, because this study reported only one patient.
Patient consent statement
The patient signed the informed consent statement for research and publication at Minda Hospital of Hubei Minzu University.
References
Author notes
Shunhua Tian and Feng Wu contributed equally to this work.



