-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmed Salawu, Maan Sarsam, Katrina Butcher, A case report and literature review of De Garengeot hernia, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae673, https://doi.org/10.1093/jscr/rjae673
Close - Share Icon Share
Abstract
The presence of an appendix in the femoral hernia, known as De Garengeot hernia, was first described by a French surgeon named Rene Jacques Croissant de Garengeot in 1731. It is a rare surgical entity occurring in only 0.5–5% of all femoral hernias. It presents typically as an irreducible lump in the groin which may be difficult to differentiate from incarcerated inguinal hernia. The risk of incarceration is high due to the narrow femoral defect which can result in extraluminal compression of the appendix causing acute appendicitis. We have presented a 71-year-old woman with a 24 hour history of incarcerated De Garengeot hernia who underwent successful open femoral hernia repair with laparoscopic appendicectomy. While open femoral hernia repair with open appendicectomy is regarded as the commonly used surgical approach, we have highlighted the importance of pre-operative and intra-operative findings in predicting definitive surgical management.
Introduction
The presence of an appendix in the femoral hernia, first described by the French surgeon Rene Jacques Croissant De Garengeot in 1731, is known as De Garengeot hernia [1]. It is a rare surgical condition with just over 400 cases described in the literature till date [2].
Femoral hernias account for 3% of all groin hernias and commonly occur in females [3]. The incidence of De Garengeot hernia is thought to be 0.5–5% of all femoral hernias [2].
Despite being aware of this condition since the 18th century, there is no agreed guidelines on the surgical management. Open femoral repair with open appendicectomy is the commonly used approach [2]. We have presented our institutional experience combining open with laparoscopy, emphasizing intra-operative findings as a key factor in determining definitive surgical treatment.
Case report
We report a 71-year-old previously fit and well female who presented to the emergency department with a 24 hour history of a painful right groin swelling. There was associated lower abdominal pain, vomiting, and passage of loose stools. She denied any abdominal distension nor fever.
She is normally independent, does not smoke, has no chronic medical conditions and no previous surgery.
Her observations were within normal range. On physical examination, there was a hard, tender, non-reducible lump in the right groin below the pubic tubercle with no overlying skin changes. Laboratory work-up were normal.
With a clinical suspicion of incarcerated femoral hernia, we requested an urgent CT scan, which showed incarcerated femoral hernia containing fluid, fat, and distal half of the appendix (Fig. 1).
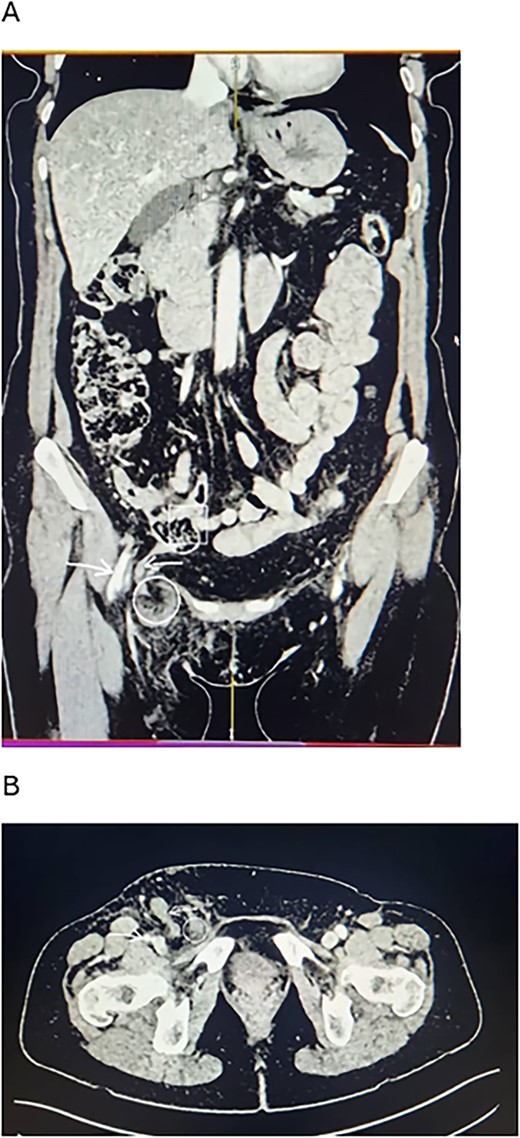
CT scan findings of the patient. (A) Coronal view. (B) Axial view. Note the long appendix (reverse arrow) extending from the ileocecal junction (squared area) into the femoral sac (circled area). There is stranding around the sac in the femoral canal. The femoral vessels (forward arrow) run beside the canal.
She was counselled for open femoral hernia repair plus proceed. Intra-operatively, a Lockwood infra-inguinal incision was made and deepened via careful dissection to enter the femoral canal. A large, dusky, and empty femoral sac containing dark exudates was isolated. The content of the sac had reduced spontaneously, presumably due to the relaxation of the abdominal muscles following general anaesthesia and the supine positioning of the patient. The sac was excised and transfixed with vicryl suture. The defect was then repaired with interrupted nylon suture using McVay technique and haemostasis secured. Decision was made to put a drain before closing the wound.
Due to the pre-operative CT scan findings of a sac containing appendix, we decided to perform a laparoscopy. At laparoscopy, a gangrenous distal half of the appendix and mesoappendix was encountered (Fig. 2). Appendicectomy was done laparoscopically and the abdominal cavity lavaged with saline. Postoperatively, she was started on soft diet. She recovered well and was discharged after 24 hours of postoperative monitoring. Histology showed a fibrotic appendix.
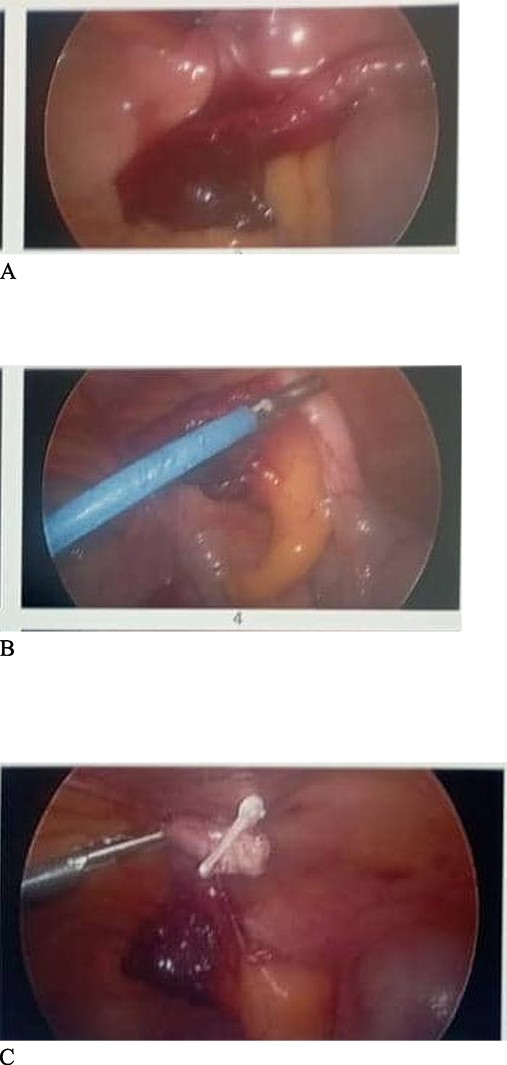
Findings at laparoscopy. (A) Distal end of the appendix herniating through the abdominal wall into the canal. (B) Appendix being pulled out of the abdominal wall defect. (C) Appendicectomy done after dissecting the mesoappendix and clipping the base of appendix with haemolock clips.
Discussion
De Garengeot hernia, defined as the protrusion of the appendix into the femoral canal is a rare surgical condition. Due to the narrow neck of the femoral canal, most cases of femoral hernia present as a surgical emergency with incarceration, obstruction, or strangulation. In De Garengeot hernia, this can be complicated with concurrent acute appendicitis [4].
The pathophysiology of De Garengeot hernia is thought to be due to a defect in the abdominal wall which results in the appendix herniating into the femoral canal. There are several anatomical variations that have been suggested to be responsible for this. Some of these include a low lying caecum, a mobile caecum, or a long appendix [2, 5]. These variations are thought to bring the appendix close to the femoral canal resulting in herniation.
De Garengeot hernia presents as a lump in the groin. The risk of incarceration is high due to the narrow femoral defect which can result in extraluminal compression of the appendix causing acute appendicitis. This possibly explains the presentation and the intra-operative findings in our index case (Fig. 2). One meta-analysis involving 90 cases reported the incidence of appendicitis in the sac to be 84% [5]. While patients may present with localized abscess and toxicity, generalized peritonitis is however rare presumably due to the narrow neck limiting the inflammatory process to the femoral canal [6].
The differential diagnosis will include any cause of groin swelling. The finding of a painful irreducible, infra-inguinal lump inferior to the pubic tubercle with negative cough impulse increases the likelihood of a De Garengeot hernia. This can be confirmed by bedside ultrasound in the emergency department, although contrast CT scan remains the gold standard with variable sensitivity and specificity [7].
Treatment of De Garengeot hernia is surgical. Although the first case was reported about 300 years ago, there has been no consensus on the surgical approach [5, 7]. Surgery can be open or laparoscopic. The choice of surgical approach depends on the presentation, pre-operative and intra-operative diagnosis and surgeon’s preference.
Open femoral hernia repair with open appendicectomy has been reported to be the commonest approach as documented in two systematic reviews [2, 5]. However, in our case, only an empty sac was encountered during the dissection, the appendix had reduced spontaneously. With a high index of suspicion, we decided to perform a diagnostic laparoscopy which then revealed a gangrenous appendix (Fig. 2).
Although regarded as the preferred method, there are aspects of the open repair that are still subjects of discussion. The type of incision for access is one of such. Some surgeons prefer the high McEvedy approach given that most De Garengeot hernias present as a surgical emergency with incarceration or strangulation and diagnosis is only made intra-operatively [7]. This incision gives a better exposure and is also useful if potential conversion to laparotomy is anticipated. Alternatively, when the clinical and radiological diagnosis is not specific for inguinal or femoral hernia, or when there is concomitant ipsilateral inguinal hernia, a Lotheissen trans-inguinal incision can be employed.
In our case, a Lockwood infra-inguinal incision was used given the short duration of symptoms and the CT scan findings of only an appendix in the sac.
The use of a surgical mesh is another aspect of surgical repair that is still not universally accepted among surgeons. We opted against using a mesh due to the dusky appearance of the sac containing foul smelling exudates. In general, the use of mesh is not advisable when there is evidence of inflammation, perforation, gangrene, or abscess.
Conflict of interest statement
None declared.
Funding
None declared.
Consent and ethical declaration
Informed consent was sought and obtained from the patient with assurance of anonymization of data. The Oxford University Press Patient Consent Form was used for this purpose.
Case report was conducted in conformity with the ethical standard of reporting case reports.
References
De Garengeot RJ.
Townsend Jr CM, Beauchamp RD, Evers BM, Mattox KL.



