-
PDF
- Split View
-
Views
-
Cite
Cite
Gu Yangjun, Fang Qingqing, Chen Zhitao, Li Qiyong, A case of rare obstructive jaundice induced by concealed displacement of T-tube, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae587, https://doi.org/10.1093/jscr/rjae587
Close - Share Icon Share
Abstract
We present the case of a 32-year-old woman who was ultimately diagnosed with obstructive jaundice. She exhibited persist jaundice, liver dysfunction with normal drainage of T-tube (400–500 ml per day), and normal stools. Prior to her admission to our department, she had undergone a cholecystectomy and T-tube placement following common bile duct exploration for cholelithiasis. Although her serum bilirubin levels initially decreased post-surgery, it rose sharply after T-tube cholangiography. The diagnosis remained unclear until we performed endoscopic retrograde cholangiopancreatography (ERCP), which revealed that the obstructive jaundice was induced by improper T-tube placement. There were few such presentations reported before, and it’s particularly unusual to encounter jaundice following T-tube placement. Moreover, diagnosing and treating this condition can be challenging when T-tube drainage appears normal. Thus, our case report provides a unique contribution to the literature on obstructive jaundice.
Introduction
Jaundice is a common clinical finding in the practice of hepatologists, which could be divided into prehepatic, hepatic, and posthepatic based on its etiology [1]. Its diagnosis primarily relies on clinical presentation, laboratory evaluation, including hepatic and cholestatic enzymes, and imaging studies [2].
Cholelithiasis is the most common cause of posthepatic jaundice. Laparoscopic cholecystectomy + laparoscopic common bile duct exploration (LC + LCBDE) was recommended for patients with gallstones and choledocholithiasis. In such cases, a T-tube would be placed to prevent postoperative complications. Monitoring of T-tube drainage involves assessing the volume, color, and consistency of bile, as well as the complaints of patients like discomfort or swelling around the T-tube site, and the characteristics of stool. Given its role as a pressure-free drainage system, it is uncommon to encounter jaundice following LCBDE and T-tube placement. However, in recent years, for the management of choledocholithiasis and cholangitis, endoscopic retrograde cholangiopancreatography (ERCP) has become the standard of care [3, 4].
Case report
A 32-year-old woman was admitted to our department with persistent jaundice. Three months ago, she presented to the local hospital with sudden onset of upper abdominal pain. The CT scan suggested cholelithiasis with cholecystitis. She has had a history of hemolytic anemia for more than 10 years.
Though there was no significant obstruction manifestation in the CT scan, the markable elevated total bilirubin and gallstone necessitated an emergency operation (LC + LCBDE). Postoperatively, her bilirubin levels gradually decreased to around 100 μmol/L, with a T-tube output of ~800 ml per day and normal stools.
One month ago, she went to the hospital due to acute pain around the drain orifice for 3 days. The T-tube cholangiography was performed. However, during the procedure, the patient suffered sharp burning pain at right upper quadrant, chills, and hyperpyrexia. Although the cholangiography showed no obstruction of the bile duct, her symptoms suggested acute cholangitis. And her serum bilirubin increased sharply after cholangiography. Despite antibiotic therapy and T-tube drainage, her serum bilirubin exceeded 700 μmol/L, necessitating two sessions of plasma exchange. Glucocorticoid shock therapy was also taken to stabilize the liver cell membrane and reduce inflammation.
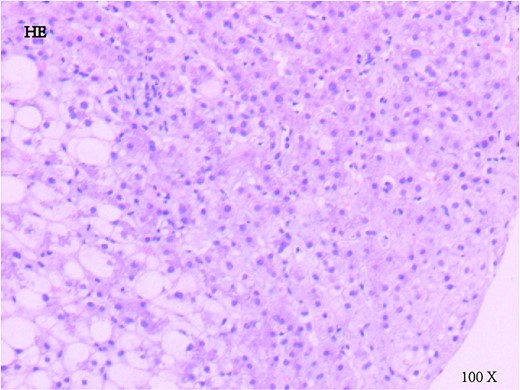
When she was admitted to our hospital, she was taking 20 mg methylprednisolone per day and complained of stomach discomfort with increased serum bilirubin for 322 μmol/L [238 for direct and 84 for indirect; normal ranges are 0–23(TB), 0–7(DB), and 3–14(IB)]. Tests for ceruloplasmin, immunoglobulin subtype 4 were negative. Although her reticulocyte count was elevated to 16.8%, there was no typical manifestation of hemolytic anemia, and her serum hemoglobin was stable; peripheral blood smears and urobilinogen were negative. A liver biopsy was performed when these non-invasive tests were inconclusive (Fig. 1). It revealed moderate cholestatic hepatitis according to cell morphology and immunostaining.
Despite the absence of obstruction on the T-tube cholangiography performed at the local hospital, we recommended ERCP. The biliary tract contrast during the operation revealed a slight distortion of the common bile duct (shown in Fig. 2), and a plastic biliary stent was placed to mitigate the distortion. The T-tube was subsequently removed, as her jaundice resolved rapidly following the procedure (bilirubin levels dropped from 382 to 159 μmol/L within 4 days).
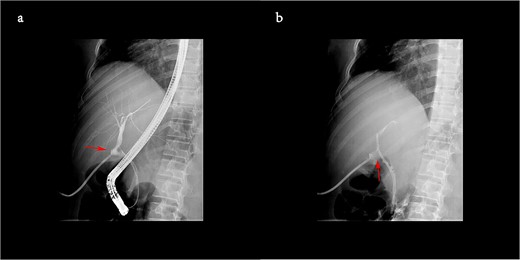
The biliary tract contrast during ERCP showed a slight distortion of duct (a), and one plastic biliary stent was placed to mitigate the distortion (b).
Finally, the patient was diagnosed with obstructive jaundice due to the distortion of the common bile duct (CBD) caused by the T-tube. And the plastic biliary stent was scheduled for removal 3 months later.
Discussion
Jaundice can be induced by various pathogenesis, among which, obstruction was the most common. It can result from choledocholithiasis, benign biliary strictures, pancreaticobiliary malignancies, and metastatic disease [5].
Historically, T-tube was placed in CBD after exploration to provide external bile drainage and internal support. By bypassing the sphincter of Oddi and offering structural support, the T-tube effectively reduces CBD pressure, ensuring satisfactory drainage. However, in some patients after CBD exploration, bile could also drain internally through duodenal papilla, complicating the assessment of normal bile volume via the T-tube. Like this patient showed above, despite a T-tube drainage of ~400 ml/day and normal stool passage, obstructive jaundice persisted.
It’s difficult to measure intrabiliary pressure through a non-invasive method, despite its importance in indicating biliary content reflux into the vascular system [6]. The additional complications of surgical duct exploration about T-tubes are predominantly bile leakage and tube displacement [4]. Migratory T-tube could result in bile duct distortion, leading to recessive stenosis and increasing intrabiliary pressure. During cholangiography through T-tube or ERCP, extra external pressure was often required to inject contrast media, which exceeded the intrabiliary pressure induced by distortion, potentially leading to false-negative results for obstruction.
A meta-analysis by the Cochrane Collaboration found that there is no significant difference in the mortality, morbidity, retained stones, and failure rates between the LCBDE and ERCP [7]. In selected patients, LCBDE for concomitant gallstones and CBD stones might be considered as the preferred approach for its higher rate of complete clearance and lower postoperative hospital stays [8, 9]. ERCP, being less invasive and more widely available, remains a popular choice, particularly for elderly patients (>75-years-old) or in settings where surgical expertise in LCBDE is limited [10, 11].
Conclusion
This case emphasizes that care should be taken when there are signs of T-tube accidental dislodgement, including acute pain, swelling around the T-tube site, and re-elevated jaundice. In addition, this case also highlights the value of ERCP in posthepatic jaundice diagnosis and treatment.
Author contributions
Gu Yangjun wrote the paper; Fang Qingqing, Chen Zhitao, and Li Qiyong performed the edit and review.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.



