-
PDF
- Split View
-
Views
-
Cite
Cite
Yu Kagaya, Taichi Takada, Kenichiro Akagi, Mine Ozaki, Norihiko Ohura, Bidirectional pressure-induced penetrating necrotizing compartment syndrome in the forearm and surgical reconstruction using a two-lobed latissimus dorsi musculocutaneous flap in nonfunctional hand scenarios: a report of two cases, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae582, https://doi.org/10.1093/jscr/rjae582
Close - Share Icon Share
Abstract
This report describes two similar cases in which the distal forearm was compressed between the rib cage and floor for a prolonged period owing to immobility, resulting in severe compartment syndrome and extensive penetrating necrosis in the forearm. The cases were a 59-year-old man with cervical spondylolisthesis and a 65-year-old man suspected of having Parkinson's disease. A distinctive necrotic pattern characterized by necrosis in the volar and dorsal compartments, preservation of the lateral compartment, and retention of the radial artery was commonly observed in both cases. Despite the anticipated nonfunctional outcome of the salvaged limb, a two-lobed free latissimus dorsi musculocutaneous flap transfer with interposition of the thoracodorsal nerve in the median nerve defect was performed in both cases. Although the salvaged limbs were nonfunctional, the patients were able to use it for activities such as getting up and other daily tasks.
Introduction
Forearm compartment syndrome is the most common type of acute compartment syndrome in the upper extremities, typically resulting from fractures, soft tissue injuries, or vascular injuries [1, 2]. Immediate fasciotomy is required to decompress the affected compartment after the diagnosis of compartment syndrome. If not treated appropriately, it can lead to severe consequences such as nerve damage, gangrene, Volkmann’s contracture, and rhabdomyolysis, causing functional loss in the forearm and hand [1, 2]. When the forearm and hand tissues are severely damaged and cannot be functionally salvaged, the decision between amputation and pursuing wound healing becomes challenging [3].
This report describes two similar cases in which the distal forearm was compressed between the rib cage and floor for a prolonged period owing to immobility, resulting in a pressure ulcer, compartment syndrome, and penetrating necrosis in the forearm. Despite the anticipated nonfunctional outcome of the salvaged limb, a two-lobed free latissimus dorsi musculocutaneous (LDMC) flap transfer with nerve reconstruction was performed to salvage the arm. Although nonfunctional, the preserved limb still played a certain role in the patients’ life.
Both patients provided written informed consent for the report of their cases.
Case reports
Case 1
A 59-year-old man with cervical spondylolisthesis exhibited slow movements in the lower body. He lived alone at home. A home care nurse discovered that he had fallen out of his wheelchair at home, leaving him immobilized in the lower left lateral position. He was subsequently brought to the emergency room. Upon medical examination, the patient was found to have pressure sores on his left distal forearm, thorax, femur, greater trochanter, and left knee. The left distal forearm, which was trapped between the rib cage on the left lateral chest and floor, was the most severely injured. Almost all the muscles, tendons, and nerves located in the volar and dorsal compartments of the distal forearm were necrotic, and a penetrating defect with bone exposure was observed (Fig. 1). The hand was completely nonfunctional, and all lesions showed a loss of protective sensation (6.65) in the Semmes-Weinstein monofilament test [4] (Fig. 1). Wound bed preparation with debridement and negative-pressure wound therapy was performed. During the course, the ulnar artery spontaneously collapsed and caused major bleeding because of the damaged and fragile vascular wall, and it was subsequently ligated. Despite the anticipated nonfunctional outcome of the salvaged limb, the left hand was determined to be necessary for the patient’s mobility, particularly when trying to get up from a wheelchair. Therefore, a decision was made not to amputate but to proceed with limb reconstruction using a free LDMC flap.
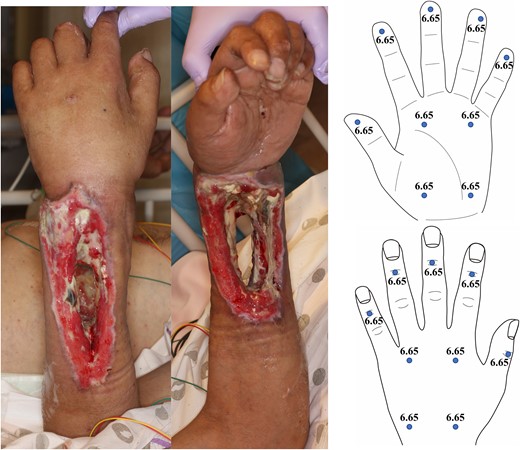
Pre-reconstructive surgery findings (including photographs and Semmes-Weinstein monofilament test) for Case 1.
A boomerang-shaped two-lobed LDMC flap was elevated from the left dorsal region (Fig. 2). The proximal stump of the ligated ulnar artery was used as the recipient vessel, and anastomoses were made from the thoracodorsal artery to the ulnar artery (end-to-end) and thoracodorsal vein to the radial cutaneous vein (end-to-end). The thoracodorsal nerve was harvested, split in half, extended, and interposed with the median nerve defect (Fig. 3). Two skin paddles were placed on the palmar and dorsal sides of the forearm skin defect (Fig. 3).

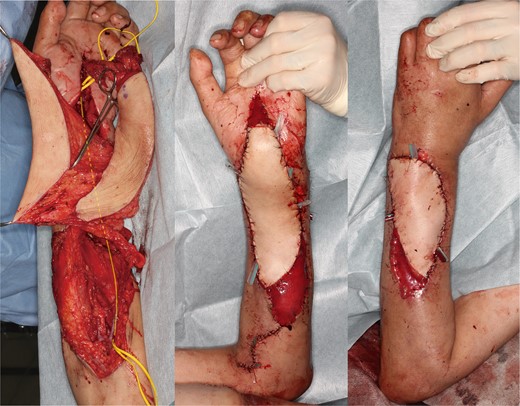
Intraoperative findings of the reconstructed area in Case 1 (The line indicates the split and interposed thoracodorsal nerve for median nerve defect).
The postoperative course was uneventful, with excellent contour and complete wound healing being maintained at 11 months postoperatively (Fig. 4). The wrist was nonfunctional in mild dorsiflexion, and the fingers were fixed in palmar flexion, with the hand being nonfunctional. However, the median nerve area of the palm showed the best sensation recovery (3.22–3.61; diminished light touch in the Semmes-Weinstein monofilament test [4]) among the hands (Fig. 4). The reconstructed left upper limb was useful for getting up from the wheelchair using the hand as a grab stick to push the armrest (Fig. 5) and holding on the handrailing to walk. The moderate sensation recovery in the palm appeared to be useful when using the hand. The home nursing system was strengthened, and he resumed living alone.
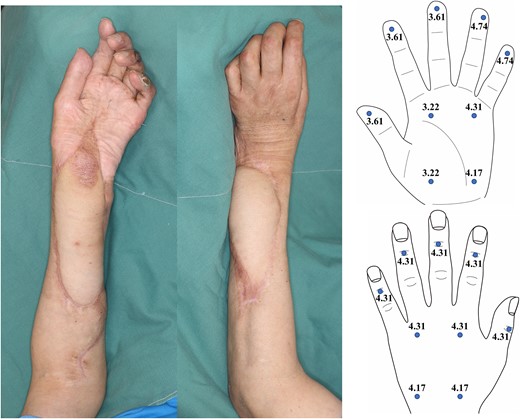
Photographs of the reconstructed area and results of Semmes-Weinstein monofilament test at 11 months postoperatively of Case 1.

Photographs of the patient standing up from a wheelchair and the donor site of Case 1.
Case 2
A 65-year-old man, suspected of having Parkinson's disease but without confirmed diagnosis, lived alone and had a history of difficulty moving after falling on several occasions. His sister found him immobilized in a slightly lower right-prone position after a fall at home and rushed him to the emergency room. Pressure sores were observed on the right distal forearm and hand, anterior chest and cheek, knees, and the dorsal surface of the toes. The right distal forearm, trapped between the rib cage on the right anterior chest and the floor, was the most severely injured. The study authors decided to salvage the right forearm with one-stage debridement and free LDMC flap transfer, aiming to preserve as many nerves and muscles as possible.
After necrotic tissue debridement, almost all muscles, tendons, and nerves in the volar and dorsal compartments of the distal forearm were removed (Fig. 6). The poorly preserved median nerve was dry and almost necrotic. The radial artery was intact, and although the ulnar artery appeared to be maintained as a structure, the blood flow was disrupted. A vertical, two-lobed LDMC flap was elevated from the left side of the back (Fig. 6). The thoracodorsal artery was anastomosed in a flow-through manner to the radial artery, using the subscapular artery for the proximal anastomosis, and the circumflex scapular artery for the distal anastomosis. The thoracodorsal vein was anastomosed end-to-end to the radial vein. The necrotic portion of the median nerve was removed and interposed with the thoracodorsal nerve. Two skin paddles were placed on the palmar and dorsal skin defects through the interosseous regions.
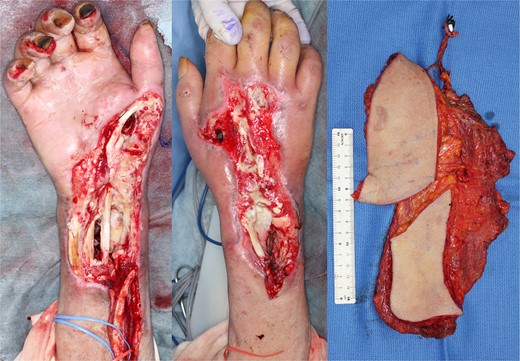
Intraoperative findings of Case 2 (after debridement and elevated flap).
The postoperative course was uneventful. At 4 months postoperatively, the patient was transferred to a long-term care facility with no follow-up. At this point, the flap was still bulky; however, the wound had healed completely (Fig. 7). At that time, there had been no sensation recovery in the hand, which remained nonfunctional with mild dorsiflexion of the wrist and flexion of the fingers. The patient was able to stand up and walk with assistance and was undergoing rehabilitation to use the reconstructed upper limb to push an armrest or bed to stand up.

Photographs of the reconstructed area at 4 months postoperatively of Case 2.
Discussion
We report two similar and unusual cases involving penetrating necrosis in the distal forearm. The unique mechanism in both cases was the patient’s immobility, leading to the forearm being trapped beneath the rib cage. This situation resulted in prolonged ischemia, pressure ulcers, and compartment syndrome. Compartment syndrome in the extremities can result from impaired consciousness owing to an overdose, and very few cases have been reported in the forearm [5, 6]. Although this case was not caused by an overdose, and the patient was conscious but unable to move, it is similar to that in a patient who cannot move independently.
The decision to salvage or amputate a severely damaged upper limb is not a simple one [3]. Every effort should be made to preserve the function of the hand and arm, when possible, as lost tissue cannot be regenerated. However, a painful, immobile, and insensate limb may not be worth preserving. Another aspect is the psychological effects after amputation. In the present cases, the decision was made to salvage the limb, and the median nerve was reconstructed to restore palm sensation, aiming to make the hand as usable as possible. As a result, in Case 1, the reconstruction of the median nerve led to a moderate recovery of palmar sensation (11 months postoperatively) and seemed to contribute to the stability of hand-pushing motion. In Case 2, the palm was still insensate at the 4-month postoperative follow-up, but it is expected to gradually recover later.
As a reconstructive option, a flap that could be divided into two skin paddles with adequate volume and good perfusion was the most suitable for the defect in these cases. In addition to the LDMC flap [7, 8], the rectus abdominis musculocutaneous flap [9, 10] and anterolateral thigh flap [11, 12] were other options. Although each of these flaps may affect the strength of the latissimus dorsi, rectus abdominis, and vastus lateralis muscles to some extent, it is undesirable to compromise the rectus abdominis and vastus lateralis muscles, given the priority of standing, maintaining posture, and walking. The deficit of the latissimus dorsi muscle may influence the adduction and extension of the shoulder joint, but the total work of shoulders 6 months after LDMC flap harvest was reported to be no different from those on the healthy side [13]. Overall, the use of an LDMC flap was considered a reasonable option in these cases. As for whether the flap should be taken from the affected or healthy side, it would be preferable to take the flap from the affected side to keep the healthy upper limb intact. However, in Case 2, a wide pressure ulcer on the anterior chest was expected to affect donor site closure after flap harvest; therefore, the flap was taken from the contralateral side.
Recently, deep tissue injury (DTI) has been proposed as a distinct classification of pressure ulcers [14]. DTI is characterized by deep tissue damage, mainly at bony prominences, leading to deep tissue ischemia and necrosis. Compartment syndrome is a possible mechanism for the occurrence of DTI [15, 16]. Animal studies have reported that pressure is mainly exerted on the bony prominence when the bone is in relatively shallow depth, whereas higher pressure is exerted on the skin or subcutaneous tissue rather than on the bone when the bone is either absent or at a significant depth [17]. In light of the above argument, the pressure might have been mainly applied to the skin and subcutaneous tissue in the interosseous area; however, on the radius and ulna region, the majority of the pressure was exerted on the bone (Fig. 8). The muscles surrounding the bone are more vulnerable to warm ischemia than the skin and subcutaneous tissue [18, 19]. Therefore, prolonged pressure around the bone would have caused muscle ischemia and deep edema, likely inducing compartment syndrome. The deep ischemia and necrosis would have reduced blood supply to the skin, while direct pressure to the skin from the floor or rib cage would also have obstructed blood flow, resulting in this penetrating gangrene.
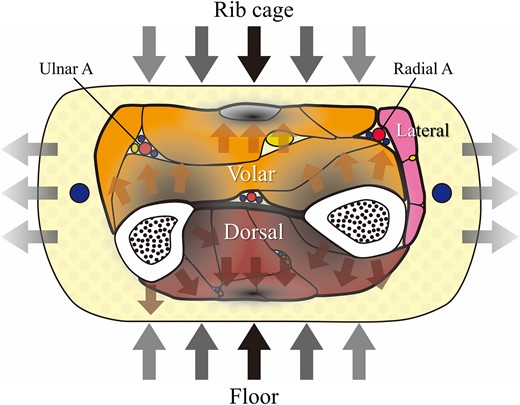
Schematic illustration of the hypothetical dynamic model in the cross-sectional view of the middle-distal third of the forearm (the possible mechanism of penetrating gangrene).
As common features of the two cases, a distinctive necrotic pattern characterized by necrosis in the volar and dorsal compartments, preservation of the lateral compartment, and retention of the radial artery were observed. Within the three compartments of the distal forearm [20], the volar and dorsal compartments are directly subjected to pressure, while the lateral compartment on the outer side of the radius is more likely to be preserved because vertical pressure partially escapes sideways (Fig. 8). In the distal forearm, the radial artery lies between the volar and lateral compartments and is barely protected from the high pressure and retaining blood flow.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Conflict of interest statement
None declared.
Funding
None declared.
References
- parkinson disease
- compartment syndrome
- decubitus ulcer
- limb
- median nerve
- necrosis
- radial artery
- reconstructive surgical procedures
- arm
- forearm
- impaired mobility
- free flap
- latissimus dorsi muscle
- thoracodorsal nerve
- compartment syndrome of forearm
- rib cage
- transfer technique
- cervical spondylolisthesis



