-
PDF
- Split View
-
Views
-
Cite
Cite
Yohei Kawatani, Azusa Yoshiyama, Takaki Hori, Placing two inferior vena cava filters for the bail-out management of opening failure of an inferior vena cava filter, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae538, https://doi.org/10.1093/jscr/rjae538
Close - Share Icon Share
Abstract
A 93-year-old man with a femoral fracture was admitted to the emergency department. The patient presented with severe hypoxemia and shock. Enhanced computed tomography confirmed deep venous thrombosis in the left leg and pulmonary embolism. Subsequently, an inferior vena cava filter (IVCF) was implanted. Although the IVCF was completely unsheathed for deployment, it remained fully folded and did not open; it was not deployed or retrieved. A new IVCF was successfully placed in the same position. Acute treatment for the deep venous thrombosis and further pulmonary embolism was achieved.
Introduction
Inferior vena cava filter (IVCF) placement is recognized as a relatively safe technique with a low incidence of acute-phase complications [1]. We present the case of an IVCF placement complication and the management technique we applied to overcome it.
Case report
A 93-year-old man was admitted to our emergency clinic with a left femoral fracture. He presented with severe hypoxemia and shock. Treatment included high-density oxygen administration using noninvasive positive pressure ventilation (NPPV), fluid resuscitation, and epinephrine administration. Duplex ultrasonography revealed deep venous thrombosis (Fig. 1a). Computed tomography of the enhanced pulmonary artery and lower extremity veins revealed pulmonary thromboembolism and deep venous thrombosis in the left superficial femoral and popliteal veins (Fig. 1b and c). Echocardiography revealed right ventricular dilation and pulmonary hypertension at 43 mmHg. D-dimer and NT-proBNP levels significantly increased to 48 and 1941 pg/ml, respectively. Immediate heparin administration was contraindicated because the patient was at risk of hemorrhage from the femoral fracture. IVCF implantation was recommended.
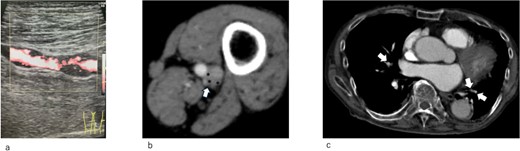
(a) Duplex ultrasonography image of the left superficial vein on admission. A thrombus is observed in the vein. (b) Enhanced computed tomography on admission. Left popliteal venous aneurysm (arrow). A thrombus is observed in the aneurysm (*). (c) Enhanced computed tomography on admission. A pulmonary embolism is observed (arrow)
An IVCF was inserted into the inferior vena cava (IVC) using the right internal jugular venous approach. After performing IVC venography (Fig. 2a) using a driver sheath, the IVCF was attempted to deployed. However, the IVCF did not open (Fig. 2b). To retrieve the unopened filter, a plunger was pulled; however, the IVCF and plunger detached (Fig. 2c). We attempted to remove the IVCF via a right femoral venous approach using a snare. However, the snare did not pass through the IVCF because the tip of the leg was attached to the IVC wall or gonadal vein ostium. The hemodynamics of the patient worsened during the procedure. Therefore, we decided to quit additional endovascular retrieval and place a new IVCF. A new IVCF was placed to hold the unopened IVCF at the proximal (head) portion of the unopened IVCF through a right jugular approach (Fig. 2d). An unopened IVCF was placed with pulling the delivery sheath (Fig. 3).
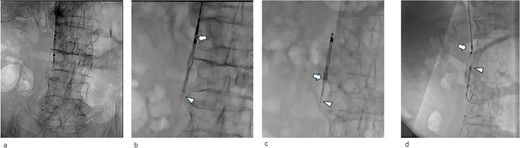
Intraoperative radiographic fluorescence imaging. (a) Pre-deployment venogram of the inferior vena cava (IVC) demonstrating appropriate positioning of the delivery sheath within the IVC prior to inferior vena cava filter (IVCF) placement. (b) The IVCF is not open, and the legs of the IVCF are folded. The IVCF is hung on a plunger. The arrow indicates the tip of the sheath. The arrowheads indicate the folded IVCF legs. (c) The IVCF could not be retrieved because it is detached from the plunger. The arrow indicates the tip of the sheath. The arrowheads indicate the folded IVCF legs. (d) The new IVCF is deployed proximal to the old IVCF.

Abdominal X-ray image after the surgery. Two inferior vena cava filters are placed.
After confirming the absence of progressive anemia because of the hemorrhage from the femoral fracture, heparin was administered systemically. Following improved arterial blood oxygenation, NPPV was discontinued on hospital Day 3, and oxygen administration was discontinued on hospital Day 10. The patient was discharged on Day 15 of hospitalization. Enhanced computed tomography revealed that the IVCF did not move (Fig. 4a–c) and the pulmonary embolism improved; however, the thrombus remained in the left femoral and popliteal veins.
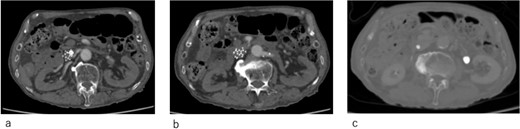
Computed tomography images 14 days after surgery. (a,b) The IVCF is still folded and not open. (c) Legs of IVCF are still folded.
Discussion
IVCF is generally considered safe, with a low incidence of acute complications. In addition, instances of IVCF opening failure are very rare. Ganesh et al. reported that IVCF ‘failed to open’ only in 27 (0.18%) out of 14 784 cases [2]. The etiology of IVCF opening failure has been attributed to entanglement of the IVCF legs [3], misplacement into the gonadal or femoral veins [3, 4], or thrombus formation in the delivery sheath during deployment [5, 6]. In our case, the etiology was assumed to be entanglement of the IVCF legs or misplacement of the IVCF tip into the left gonadal vein based on the shape of the failed ICVF (Figs 2a and 4c).
Sohail et al. reported cases of failure to open a Vena Tech LP filter (B Braun, Evanston, Illinois, USA), which can be critical if persistent, potentially leading to complications such as migration to the heart or pulmonary artery [7]. Therefore, avoiding its migration is crucial when an IVCF fails to open. We assume that removing an IVCF that failed to open is the simplest and the best approach. However, this was not feasible in the present case. The IVCF could not be retrieved from the delivery sheath because it was detached from the plunger. In addition, the IVCF could not be retrieved using the snare because its tip was engaged with the wall of the IVC or gonadal vein ostium. The sling technique or loop snare technique [8] was also not applicable in our case as we attempted to implant the IVCF promptly to prevent the patient’s hemodynamics from further worsening because of the additional pulmonary embolism. Therefore, we decided to use a new IVCF. The new IVCF was placed on the proximal (head) portion of the unopened IVCF to trap it and avoid migration. Ultimately, the IVCF did not migrate to the heart, and acute-phase treatment for deep venous thrombosis and pulmonary embolism was achieved.
Retrieval of the unopened IVCF from the jugular vein after placement of the new IVCF could have been an option, with a possibly higher success rate than retrieval from the femoral approach. However, in this approach, wires and sheaths for retrieval should go through the new IVCF, which could interfere with, deform, or migrate it. Therefore, we decided not to retrieve the unopened IVCF and placed two IVCFs instead.
Despite being effective in avoiding the migration of the unopened IVCF and treatment of the acute pulmonary thromboembolism, our approach remained of concern. IVCFs have been reported to cause chronic perforation to the IVC wall, even with appropriate deployment [9]. In this patient, the tip of the unopened IVCF was folded (Figs 3 and 4c); thus, the risk of perforation increased because of the stiffness of the folded IVCF legs. Therefore, close monitoring is required.
Placing a new IVCF and ending up with two IVCFs was an effective bail-out management for the IVCF that failed to open, and acute treatment for deep venous thrombosis and pulmonary embolism was achieved.
Acknowledgements
The local ethics committee approved this study (approval number: KGHEC24-004).
Conflict of interest statement
None declared.
Funding
Self-funded.
Consent for participation and publication
Consent to participate and consent for publication were obtained from the patient.



