-
PDF
- Split View
-
Views
-
Cite
Cite
Pratiksha Paudel, Srikant Agrawal, Bidur Khatiwada, Prahasan Rai, Sijan Karki, Pedicled falciform ligament flap use as an alternative surgical technique in peptic ulcer perforation repair: a case report and review of literature, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae502, https://doi.org/10.1093/jscr/rjae502
Close - Share Icon Share
Abstract
Peptic ulcer disease (PUD) affects ~4 million people globally. Peptic ulcer perforation (PUP) is a serious complication of PUD associated with high mortality and morbidity. Hence, a high index of clinical suspicion is crucial in diagnosing such cases. Here, we present a case of a 19-year-old male who presented with 4 days of severe abdominal pain, fever, and vomiting. On examination, signs of acute abdomen were evident, and an erect chest X-ray confirmed free air under the diaphragm. The patient underwent an emergency midline laparotomy, during which 1000 ml of purulent fluid was evacuated. A perforation measuring 8 × 8 mm2 was repaired using the falciform ligament due to the unavailability of adequate healthy omentum. His postoperative recovery was uneventful. This case report underscores the importance of considering the falciform ligament as a viable and effective alternative for the closure of PUP when the omentum is unavailable.
Introduction
Peptic ulcer perforation (PUP) is a life-threatening complication of peptic ulcer disease (PUD), with a mortality rate ranging from 10 to 40% [1, 2]. The hallmark of PUP is the classic triad of sudden onset abdominal pain, tachycardia, and abdominal rigidity. The presence of free air under the diaphragm on an erect chest X-ray strongly suggests a diagnosis of PUP [1, 2]. The treatment of choice for PUP remains surgery, with the most commonly preferred approach being simple closure of the perforation using an omental patch [3]. In cases where the omentum is unavailable, a PUP can be closed using a falciform ligament pedicle flap [4]. In this case report, we utilized the falciform ligament as an alternative technique for effective patch closure of a PUP.
Case report
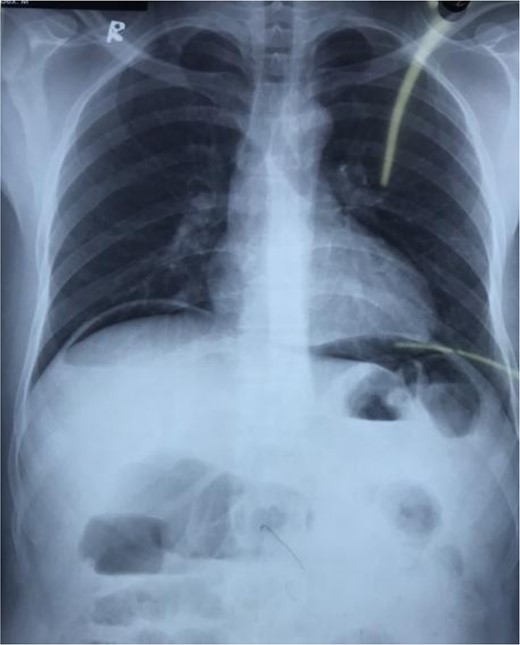
A 19-year-old thin male without known medical conditions presented to our emergency room with a 4-day history of increasingly severe abdominal pain with 3 days of fever, and repeated episodes of vomiting. He had no history of previous abdominal surgery, per-rectal bleeding, or any similar episodes. He is a smoker and consumes alcohol. He was normotensive (BP: 120/80 mmHg) and febrile (temperature: 101 F) with tachycardia (pulse: 111 bpm). On physical examination, his abdomen was distended with generalized tenderness, rebound tenderness, guarding, and rigidity. His total leukocyte count was 26 260/cu. mm, but all other hematological and biochemical parameters were normal. An erect chest X-ray revealed free air under the diaphragm (Fig. 1). An abdominal ultrasound showed moderate ascites with internal septations and moving debris.
A clinical diagnosis of hollow viscus perforation was made. The patient was resuscitated with intravenous fluids and antibiotics before undergoing emergent exploratory laparotomy via midline incision. After draining 1000 ml of purulent fluid, an 8 × 8 mm2 perforation was observed in the anterior wall of the first part of the duodenum. There were inter-bowel adhesions with flakes, and the omentum appeared thin, translucent, and short, extending only ~2–3 cm beyond the greater curvature of the stomach.
Due to inadequate healthy omentum for graft purposes, the falciform ligament was freed from the anterior abdominal wall and its free end was utilized as a graft to repair the perforation site with polyglactin 3–0 sutures (Fig. 2). Confirmation of no leakage was done by pushing air from nasogastric (NG) tube. The wound was closed after thorough peritoneal lavage with a drain placed in Morrison’s pouch. His postoperative course was uneventful. NG tube and abdominal drain were removed on the third and seventh postoperative day, respectively. He was discharged with triple therapy and 1 month of proton pump inhibitor. At a follow-up in the Outpatient department after a month, he was doing well with no complications.
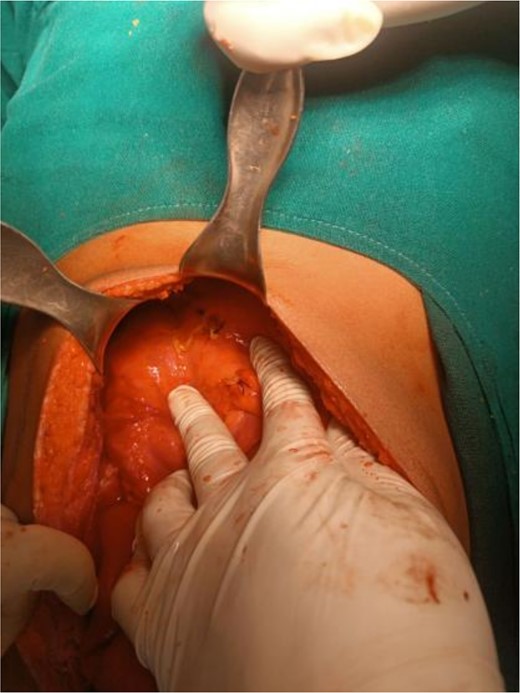
Falciform ligament used as a graft to repair the perforation site using polyglactin 3-0 sutures.
Discussion
PUD arises from an imbalance between stomach acid-pepsin levels and mucosal defenses [1]. Annually, PUD affects ~4 million people worldwide. Major complications include bleeding, perforation, penetration, and obstruction, occurring in ~10–20% of cases [2, 5]. Perforation, seen in 2–14% of cases of PUD, is a surgical emergency with a mortality rate of 10–40% [2]. The primary risk factors of PUP are Helicobacter pylori infection and NSAID use. Additional risks include stress, smoking, corticosteroid use, and a history of PUP [1]. Here, we present a case of a 19-year-old boy with a history of smoking and alcohol consumption.
PUP usually presents with sudden onset abdominal pain, tachycardia, and abdominal rigidity. Other manifestations include tachycardia, cool extremities, abdominal rigidity with right lower quadrant tenderness, pyrexia, and hypotension, often leading to acute circulatory collapse [1]. Early detection of PUP relies on a high degree of clinical suspicion. Our patient presented with worsening abdominal pain for 4 days, accompanied by fever and multiple episodes of vomiting. On examination, he was febrile with tachycardia and exhibited features of peritonitis.
An upright chest or abdominal X-ray is the initial imaging choice for suspected PUP and detection of free air under the diaphragm is highly suggestive and often confirms the diagnosis [2]. If X-ray results are inconclusive, an abdominal computed tomography scan is recommended for its superior sensitivity in detecting intra-abdominal free air. In our case, the erect chest X-ray of our symptomatic patient revealed free air under the diaphragm confirming the diagnosis of PUP.
Initiating prompt treatment is crucial to reduce the mortality and morbidity associated with PUP. Emergency surgical repair is the treatment modality of choice for PUP. Small ulcers are treated with laparoscopy, whereas large pyloric perforations often require open surgery [6]. The most commonly used techniques include primary closure with interrupted sutures, closure with interrupted sutures covered by a pedicled omentum, and plugging the perforation with a free omental plug (Graham patch) [7].
However, an alternative method is necessary in cases when the omentum may not be technically feasible for use or maybe absent sometimes due to previous abdominal surgeries. In such cases, the falciform ligament should be used as it is an easy and efficient alternative technique in the management of PUP [6]. The use of a falciform ligament patch as an alternative method for the management of perforated PUP was first reported by Fry et al. in 1987 [6, 8]. The falciform ligament is a broad, sickle-shaped fold of the peritoneum that extends from the umbilicus rostrally over the anterior superior hepatic surface [9]. It is well-vascularized, similar to the hypervascular omentum, making it suitable for use as a flap. It lies across the duodenum and can be sutured to an ulcer without tension or mobilization enhancing strength and nourishment [6]. Preoperative shock, open surgery, and prolonged operating time are major risk factors for higher postoperative risks, including suture leaks, intra-abdominal abscesses, and increased reoperation rates [6, 10]. Our patient underwent emergency midline laparotomy with evacuation of purulent fluid and pedicled falciform ligament was used to successfully repair the perforation site as the omentum was technically unusable. His perioperative and postoperative recovery was uncomplicated.
Conclusion
In conclusion, when omentum cannot be utilized as a graft for PUP repair, a falciform ligament patch can be used as a feasible and effective alternative surgical technique. This case highlights the importance of prompt diagnosis and selection of appropriate alternative surgical techniques in achieving successful patient outcomes in similar clinical scenarios. Nonetheless, comparative studies are further needed for the validation of the outcomes with a larger sample size.
Conflict of interest statement
None declared.
Funding
None declared.



