-
PDF
- Split View
-
Views
-
Cite
Cite
Hamid Abdulla Al Wadaani, Sarah Al Omar, Jawaher AlRaihan, Jawad S Alnajjar, Mohamed Elserougi, Hussain Al Jabran, Post laparoscopic sleeve gastrectomy portal vein thrombosis with venous mesenteric ischemia: a case report with literature review, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae462, https://doi.org/10.1093/jscr/rjae462
Close - Share Icon Share
Abstract
Saudi Arabia’s obesity prevalence is 19.2% among men and 21.4% among women. Treatment includes lifestyle modifications, medication, and bariatric surgery. Procedures reach up to 1200 annually in our center. Porto-mesenteric venous thrombosis associated with venous mesenteric ischemia and bowel necrosis is a rare complication that necessitates an early workup and management. A 29-year-old Saudi male underwent laparoscopic sleeve gastrectomy. Post-surgery, he experienced abdominal pain, nausea, and vomiting, exacerbated by eating and smoking. Abdomen computed tomography scans revealed engorged portal veins, congested mesenteric veins, and small bowel thickening. He underwent exploratory laparoscopy shifted to laparotomy with resection of an infarcted omentum and 1 m of jejunal small bowel loop, and was discharged postoperatively after 7 days. Porto-mesenteric venous thrombosis is a rare complication after laparoscopic sleeve gastrectomy, requiring early diagnosis and appropriate treatment. Patients present with non-specific symptoms, necessitating high suspicion for computed tomography recommendations.
Introduction
Obesity is common in Saudi Arabia, which raises the possibility of people developing certain complications [1]. The World Obesity Organization reports that overall obesity prevalence in Saudi Arabia is 19.2% among men and 21.4% among women, in boys; the rates are 3.6%; and in young girls, the rates are 4% [2]. The primary line of treatment for obese and overweight people to reach and maintain a healthy weight through long-term habits is lifestyle modification [3]. For patients who are extremely obese, medication for maintaining weight reduction, intragastric balloons, and bariatric surgery are advised as medical and surgical treatments [4]. In Saudi Arabia, 15 000 bariatric procedures are reportedly performed annually [5]. In our center, the estimated number of cases is up to 1200 annually.
A rare but serious surgical complication that can arise in individuals undergoing laparoscopic sleeve gastrectomy is portomesenteric venous thrombosis (PMVT). Common causes have been proposed to be venous stasis secondary to increased intra-abdominal pressure, operative intervention in the splanchnic vasculature, and hypercoagulable state. Diagnosing PMVT following laparoscopic sleeve gastrectomy requires a high index of suspicion, as patients typically present with unclear signs and symptoms that are challenging to elicit early on [6]. A serious side effect that has been documented in 1.5%–3% of instances following laparoscopic sleeve gastrectomy is gastric leaks, as well as postoperative hemorrhage and the development of an abscess [7].
Case presentation
This is a 29-year-old Saudi male, who presented to our clinic as a case of morbid primary obesity for laparoscopic sleeve gastrectomy. The patient is a smoker but has no chronic illness, he underwent carpal tunnel release as a surgical history; he has no known allergies; and he is psychologically stable. His weight gain started ~10 years ago, weight reduction by the patient was tried using lifestyle modification and exercise with multiple failed attempts. At the time of presentation, the patient’s height was 164 cm, weight was 113 kg, and BMI was 42.5. The patient had a family history of obesity. Upon examination of the patient, he appeared conscious, alert, and oriented to time, place, and person; he was vitally stable.
The patient was also assessed before surgery by anesthesia and cleared for surgery. He underwent elective laparoscopic sleeve gastrectomy under general anesthesia with uneventful events. On Day 1 post-op, the patient was in a good clinical condition, tolerated oral fluids, and ready for discharge. His discharge medications were the following: enoxaparin 40 mg subcutaneous for 2 weeks and acetaminophen for pain management. On his 2-week postoperative visit, the patient presented to our bariatric clinic with the complaints of right upper quadrant abdominal pain. His pain was mainly aggravated by eating and smoking. The patient reported that the pain was associated with nausea and vomiting; however, he denied any history of fever, chilis, or rigors, and there was no history of any change in his bowel habits. Further history-taking revealed that the patient has had dark color urine over the last few days prior to his presentation. His abdomen exam showed tenderness in the right upper quadrant and epigastric region. The surgery team decided to admit the patient for further investigation and management.
Patient was admitted, and his laboratory investigations demonstrated a normal CBC level, electrolytes were also within normal level, total bilirubin: 17.10 μmol/L, direct bilirubin: 8.80 μmol/L, amino transferase alanine: 36.00 u/L, amino transferase aspartate: 19.00 u/L, alkaline phosphatase: 83 0.00 u/L. Abdomen ultrasound demonstrated mild to moderate intraperitoneal fluid collection, noted mainly in the perihepatic, peri splenic region (Fig. 1). Computed tomography (CT) with oral and IV contrast was ordered for further assessment. The CT showed a non-enhancing portal vein and its branches, a superior mesenteric vein and its tributaries, which are engorged and associated with dirty and congested mesentery, as well as a small amount of peritoneal free fluid denoting venous thrombosis along the portal mesenteric axis with no evidence of contrast leak from the gastric sleeve (Fig. 2). Vascular surgery and hematology consultations were immediately done; they assessed the patient and started him on enoxaparin 100 mg along with a serial abdominal exam. On Day 2 of the current admission, the patient had one episode of fresh blood per rectum, around 150 ml of fresh blood, and dark blood-tinged vomiting of minimal quantity around 10 ml. The patient became agitated, and his abdomen was distended with generalized tenderness. He was immediately resuscitated with two unmatched red blood cell pack transfusions, and then shifted to intensive care units. CT scan angiography of the abdomen was done at that time and reported as follows: non-enhancing portal vein and its branches, superior mesenteric vein and its tributaries, which are engorged and associated with dirty and congested mesentery with a slight increase in the amount of peritoneal free fluid denting venous thrombosis along the portal mesenteric axis. Mild diffuse mural wall thickening of the small bowel is likely related to venous congestion. Aorto-iliac arteries: the visualized abdominal aorta and its bifurcation into right and left common iliac arteries appear intact. The common iliac arteries, internal and external iliac arteries appear intact bilaterally. Mesenteric arteries: the main trunk of the superior mesenteric artery appears intact with no obvious segmental arterial stenosis or occlusion. The inferior mesenteric artery and its main divisions appear intact, with no obvious main or branch occlusion. Celiac artery: The celiac artery and its main divisions, including hepatic, gastric, and splenic divisions, appear intact with no obvious main or branch occlusion.

An ultrasound picture showing free fluid (FF) (white arrow) around the liver (L).

CT scan abdomen and pelvis, coronal view showing non enhancement of portal vein and its branches indicating venous thrombosis along the portal mesenteric axis (white arrow).
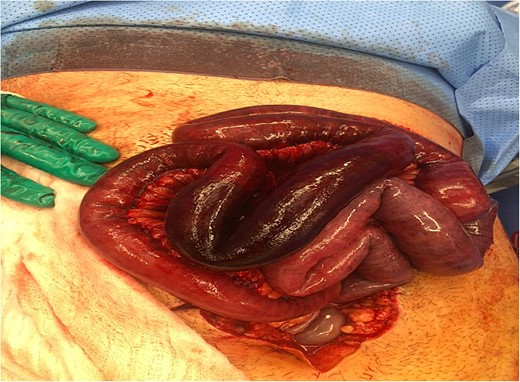
The decision was to take the patient to the operating room for exploratory laparoscopy, which was shifted to laparotomy. Intraoperative findings showed an infarcted omentum with almost 1 m of gangrenous small bowel jejunal loop with no perforation. Resection was done of the infarcted omentum along with the gangrenous jejunal loop (Figs 3 and 4), and the time was given to assess the viability of both small bowel limbs. After confirming that both sides of the bowel were healthy, side-to-side functional end-to-end anastomosis done using a GIA stapler with closure of the mesenteric defect. The rest of small and large bowels were found to be healthy. The abdomen was irrigated with warm saline, and two drains were placed inside the abdomen. The abdomen was closed primarily using PDS sutures. The patient shifted back to the intensive care unit for further management and monitoring. His postoperative course was uneventful, and the patient was discharged on postoperative Day 7. He was followed in the outpatient clinics for almost 6 months with no active complaint.

Intra-operative picture showing congested and infarcted omentum.
Discussion
Over the past seven decades, bariatric surgery has evolved significantly with the development of numerous surgical techniques. Four procedures have gained official recognition from all relevant medical societies: sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), bilio-pancreatic diversion (BPD), and adjustable gastric banding (AGB). While bariatric surgery is usually safe and effective, it carries a risk of serious, sometimes fatal, complications [8]. Complications of bariatric surgery fall into two primary categories: early and late. Early postoperative complications include leaks, stenoses, bleeding, and venous thromboembolic events. Late complications may encompass acute obstruction, megaesophagus or pseudoachalasia, band erosion, gallstone disease, dumping syndrome, ischemia, and even death [9]. Unexpectedly, major complications requiring reoperation within 30 days of gastric bypass surgery or sleeve gastrectomy did not affect long-term outcomes in terms of weight loss or comorbidity remission [10].
A distinctive aspect concerning our patient is the co-occurrence of PMVT and venous ischemia following bariatric surgery. The rate of PMVT after bariatric surgery was found to be 0.50%. Independent predictors of PVT include previous venous thromboembolism, liver disease, sleeve gastrectomy, and major postoperative complications [11]. Since there is no typical clinical or laboratory abnormality, patients may present with a wide range of symptoms, including tachycardia, abdominal pain, bloating, absence of bowel movements, nausea, vomiting, dehydration, fever, back pain, and even intestinal infarction. As a result, the diagnosis is made with a high degree of suspicion [12]. The most common method for confirming the diagnosis of PMVT is a contrast CT abdomen, which has a 90% sensitivity rate [6, 13]. In patients with PMVT and venous mesenteric ischemia, the treatment involves the initiation of anticoagulants and prompt exploration of the abdomen. However, clear guidelines for prophylactic and therapeutic anticoagulation in bariatric surgery patients are lacking [14]. Nonetheless, post-surgery outcomes in the anticoagulated group for preventing PMVT were superior. Despite this, anticoagulation was not the sole factor affecting the incidence of PMVT following LSG in patients with a BMI of 35–45 kg/m2 [15].
Conclusion
After a laparoscopic sleeve gastrectomy, portal and mesenteric venous thrombosis is an uncommon complication that, if not identified and treated appropriately, can have fatal implications. Patients typically appear with nonspecific abdominal symptoms when they have PMVT. Because of this, doctors should have a high degree of suspicion when recommending abdominal CT in order to confirm the diagnosis and initiate appropriate therapy.
Conflict of interest statement
None declared.
Funding
None declared.
References
- obesity
- smoking
- ischemia
- gastrointestinal tract vascular insufficiency
- thrombosis
- abdominal pain
- computed tomography
- venous thrombosis
- intestine, small
- intestines
- laparotomy
- mesenteric vein
- mesentery
- necrosis
- omentum
- portal vein
- surgical procedures, operative
- abdomen
- eating
- jejunum
- lifestyle changes
- nausea and vomiting
- portal vein thrombosis
- bariatric surgery
- sleeve gastrectomy, laparoscopic
- early diagnosis
- symptom aggravating factors
- exploratory laparoscopy



