-
PDF
- Split View
-
Views
-
Cite
Cite
Fadi Alhalak, Sultaneh Haddad, Gabriel Nasseh, Mira Nasseh, Joud Marroush, Rami Abaza, Aya AlSafadi, Majd Jehad Dakhalalah Bani Hani, George Michael Kabbabe, A cesarean section scar dehiscence during the first trimester of an intrauterine pregnancy: a rare case report and literature review, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae422, https://doi.org/10.1093/jscr/rjae422
Close - Share Icon Share
Abstract
Uterine rupture is specified as a complete laceration of the uterine wall, including its serosa, leading to a connection between the endometrial and peritoneal chambers. It can occur in any stage of pregnancy and is considered a severe and perhaps fatal complication. A 35-year-old woman at 9 weeks of gestation with a medical history of five prior cesarean sections presented with lower abdominal pain that had lasted for 5 hr. We detected small amounts of free fluid in the Douglas pouch using ultrasound. Subsequently, a laparotomy revealed a cesarean scar dehiscence from a non-cesarean scar pregnancy. Patients who experience a uterine rupture may have vague symptoms, severe abdominal discomfort, abnormal uterine bleeding, and severe hemorrhagic shock, depending on their gestational age. Ultrasound imaging can be used to diagnose this fatal condition in addition to laparoscopy to immediately identify and treat the issue in urgent cases.
Introduction
Uterine rupture is defined as a complete laceration of the uterine wall, including its serosa, resulting in a communication between the peritoneal and endometrial chambers, and this can occur at any stage of pregnancy [1]. It is a serious and potentially life-threatening complication [1], carrying a high risk of morbidity and mortality for the mother and the developing fetus [2].
The incidence of rupture in women with a previous cesarean section scar is 0.3% in comparison with an unscarred uterus, which is 1 in 5700 to 1 in 20 000 [3].
In fact, uterine rupture is a rare complication that can occur in the first trimester of pregnancy (3), even when risk factors are present [1].
Patients with a prior cesarean section were more likely to develop uterine rupture when trying a vaginal birth [3]. Short interpregnancy intervals, classical uterine scars, and misoprostol treatment can also raise the chance [3].
However, uterine rupture can occur in women with scarring from myomectomy, profound corneal resection, corneal pregnancy, trauma, and previous cesarean sections [3].
When uterine rupture manifests clinically, it usually involves acute severe abdominal pain and vaginal bleeding. Hemodynamic instability accompanied by tachycardia and hypotension may also be present in the patient [3].
Case presentation
A 35-year-old woman was admitted to the hospital after experiencing lower abdominal pain for 5 hr, with a medical history of five previous cesarean sections (CS). The last cesarean section was 2 years before the administration. There was no medical or allergic history. On physical examinations, a lower abdominal tenderness was noticed. Her vital signs were within normal ranges with a blood pressure (BP) of 110/70 mmHg and a pulse rate (PR) of 86 beats per minute indicating a stable hemodynamic condition.
An ultrasound (US) scan identified an intrauterine gestational sac with cardiac activity, a caudal-rump length (CRL) of 9 weeks, and a gestational Sac Age (GS) of 9 weeks. A small amount of free fluid was noticed in the Douglas diverticulum. Laboratory test results on admission showed a hematocrit of 33.7 g/dl, hemoglobin of 302 cells/μl, and platelets of 9.7 g/L.
Furthermore, hemoglobin levels dropped to 9.7 g/L the following day and further deteriorated to 8.7 g/dl as the patient’s hemodynamic condition worsened, with her pulse accelerating to 120 beats per minute. Ultrasound revealed a moderate amount of free fluid in the pouch of Douglas and Morrison’s Pouch with an eventration in the previous cesarean scar and the gestational sac descending to the level of this scar and starting to form an occlusal line at the upper part of the uterus (Fig. 1).
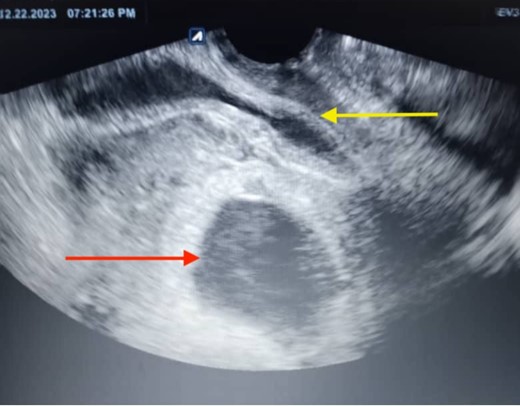
The ultrasonographic imaging conducted the day following the patient’s hospital admission revealed a ruptured gestational sac (the lower arrow), which was apparent outside the uterus. The uterine mass was visible on one side (the upper arrow), and the gestational mass was on the other side.
Given the emergent situation, a surgical procedure was initiated under general anesthesia via a Pfannenstiel skin incision. Then, it was decided to undergo a laparotomy that exposed ~1.5 L of hemorrhagic fluid and clots, followed by isolating the uterus, during which a gestational sac with the placenta, mostly protruding from the Cesarean scar, was removed along with the placental remnants (Fig. 2) (Video 1). The cesarean scar was sutured with absorbable thread, hemostasis was achieved, and the abdominal cavity was cleaned. The abdominal layers were then closed, and a drain was placed in Douglas’ pouch. During these procedures, the patient received transfusions of 3 units of complete blood and 2 units of plasma during surgery. Finally, she was discharged in good general condition 2 days later.

The extracted gestational sac at the end of the surgical procedure.
Discussion
The incidence of uterine rupture among women who have had a previous cesarean section is 3 cases per 1000 deliveries. Our patient had a uterine rupture in the first trimester of her pregnancy, which is extremely rare [4]. About 1 in 500 episodes of uterine rupture end in death, making it a risky condition with a high morbidity and mortality rate [5].
Risk factors for uterine rupture include a history of uterine surgery, such as prior cesarean delivery or myomectomy. While classical incisions during cesarean deliveries are infrequent, accounting for 0.3%–0.4% of deliveries, they pose a notable risk of uterine rupture in subsequent pregnancies, with reported rates ranging from 1% to 12% based on available literature. Our patient’s medical history includes a record of five prior cesarean sections, making her susceptible to uterine rupture [6].
The induction of labor in women with previous cesarean deliveries elevates the chances of uterine rupture when compared to spontaneous labor [7]. Specifically, misoprostol induction of labor heightens the risk of uterine rupture among women who have previously undergone cesarean delivery [8]. Moreover, uterine ruptures are more common in patients having Trial of Labor After Cesarean (TOLAC) than in patients choosing scheduled repeat cesarean delivery [9]. Uterine rupture is more likely in situations where there is a low Bishop score at the time of admission to the labor and delivery unit, dystocia, delayed cervical dilatation in the first stage of labor, and an extended second stage of labor [10–12]. However, our patient did not show any signs of labor or delivery.
Limited evidence supports the association between a history of prior uterine ruptures and an elevated likelihood of subsequent occurrences; however, our patient has no history of uterine ruptures [13].
Additional risk factors include a brief inter-pregnancy interval, prior preterm cesarean delivery, and a previous cesarean delivery complicated by severe postpartum hemorrhage. Our patient’s latest cesarean delivery was 16 months before her uterine rupture [14, 15].
Patients with uterine rupture can present with a broad spectrum of symptoms and signs, ranging from nonspecific symptoms up to acute pelvic pain, metrorrhagia, and severe hemorrhagic shock, depending on their gestational age. Therefore, women in their first trimester usually present with vague symptoms [1], which can lead to a diagnostic delay. Delays in diagnosis can result in fatalities and severe bleeding. Therefore, it’s crucial to have a high index of suspicion, especially when there’s intense stomach discomfort and abnormal vital signs [3]. Particularly the same as our patient, who suffered from lower abdominal pain with a good general health condition that deteriorated several hours later.
Diagnosing uterine rupture can be done by using US imaging, which helps to detect free fluids in the peritoneum, especially in Douglas and Morrison’s pouches [3], exactly where free fluids were found in our patient.
Ultrasound might not be useful in cases of fatal bleeding; therefore, a laparoscopy or other urgent diagnostic procedures may be required to identify and treat the condition right away [3], which was done to the patient after her vital signs began to worsen.
Before now, fewer than 50 spontaneous uterine rupture cases during the first trimester and the gestational sac within the uterus have been reported in the English literature since 1990 (Table 1). With only 14 cases, the gestational age was <10, including ours. The average age was 29 years (range: 19–43 years). The most common symptom that we have detected in nearly all cases, including ours, was abdominal pain.
| . | Author . | Age . | Gestation age . | Gravida/Para/Abortion . | Symptoms . | Risk factors . | Rupture location . | Treatment . | Follow up . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Pridjian et al. 1990 [16] | 23 | 13 | Primigravid | Hypotension, vaginal hemorrhage, abdominal pain | Pelvic irradiation 7 years before | Anterior fundal defect | Supracervical hysterectomy and left salpingo-oophorectomy | N/A |
| 2 | Dibbs et al. 1995 [17] | 29 | 8 | 2/0 | abdominal pain, diarrhea, and lightheadedness | placenta percreta | The fundus | Surgical repair | No complications |
| 3 | Arbab et al. 1996 [18] | 34 | 13 | 8/1/ep5/ab1 | Shock and acute abdominal pain | Placenta percreta, bilateral salpingectomy, left cornual resection | Right-sided uterine cornual rupture | Surgical repair | N/A |
| 4 | Arbab et al. 1996 [18] | 25 | 8 | Ab2/p2 | Hemorrhagic shock | Left cornual resection, bilateral salpingectomy | The fundus | Surgical repair | N/A |
| 5 | Marcuset al. 1999 [19] | 38 | 13 | 4/2-0-1-1 | Spotting and cramping | Two cesarean scars, placenta percreta | The lower uterine segment | Radical hysterectomy | No complications |
| 6 | Hamsho et al. 1999 [20] | 34 | 13 | 4 + 3 | Abdominal pain | Four lower segment cesarean sections | The lower part of its anterior aspect | Surgical repair | No complications |
| 7 | Porcu et al. 2003 [21] | 28 | 12 | 1/0 | Acute abdominal pain | DES | Anterior fundal area | Surgical repair | No complications |
| 8 | deRouxet al. 1999 [22] | 22 | 12 | 9/ | Abdominal pain | 6 curettages, placenta percreta | The fundus | Surgical repair | Died |
| 9 | Matsuoet al. 2004 [23] | 31 | 10 | 3/1 | Little abnormal genital bleeding and mild abdominal pain | Previous cesarean section, dilatation, and curettage | The lower uterine wall | Surgical repair | No complications |
| 10 | Parket al. 2005 [24] | 36 | 10 | *** | Abdominal pain | Without | The upper portion of the left fundus | Surgical repair | N/A |
| 11 | Dabuliset al. 2007 [25] | N/A | 9 | N/A | Abdominal pain, bloating, vomiting, and diarrhea | Three previous cesarean sections | At the site of the prior cesarean section | Hysterectomy | N/A |
| 12 | TANYI et al. 2008 [26] | 32 | 7 | 6/3 | Abdominal pain, vaginal spotting | Right salpingo-oophorectomy Cesarean section curettage, Placenta percreta | 3 cm from the dome of the uterus | Hysterectomy | N/A |
| 13 | Ijaz et al. 2011 [27] | 32 | 8 | 3/1 | Acute abdomen | Manual removal of placenta in a previous pregnancy | The fundus | Surgical repair | No complications |
| 14 | Visariyaet al. 2011 [28] | 26 | 9 | 2/1 | Abdominal pain, giddiness, and shock | Previous cesarean | Lower anterior uterine wall | Surgical repair | No complications |
| 15 | Snigh et al. 2012 [29] | 24 | 10 | Primigravida | Abdominal pain | Bicornuate uterus | Left rudimentary horn | Surgical repair | No complications |
| 16 | Tolaet al. 2014 [30] | 24 | 8 | Multigravida | Vaginal bleeding and generalized abdominal pain | Bicornuate uterus | Left part of the uterus | Left part of the uterus | No complication |
| 17 | Sinha et al. 2014 [31] | 30 | 11 | 6/5 | Syncopal attack, syncopal attack | One cesarian section, history of repair uterine rupture? | Upto the fundus | Surgical repair | No complication |
| 18 | Bandarian et al. 2015 [32] | 30 | 11 | 4/2/ab1 | Shock and acute syncopal attack | D&C, two scars | On the previous scar | Surgical repair | No complication |
| 19 | AKBAŞ et al. 2015 [33] | 36 | 12 | 8/7 | Abdominal pain | Without | At the side of the left uterine vessels extended to the cervix. | Hysterectomy | No complication |
| 20 | Taskin et al. 2015 [34] | 32 | 13 | 2/1 | Pelvic pain | Curettage, one cesarean | Posterior | Surgical repair | No complication |
| 21 | Okada et al. 2015 [35] | 39 | 10 | Primigravida | Abdominal pain and shock | Laparoscopic myomectomy | The fundus | Surgical repair | No complications |
| 22 | Pendy et al. 2015 [36] | 30 | 8 | 3/2 | Acute abdominal pain with hemorrhagic shock | A unicornuate uterus | Rudimentary horn | Surgical repair | No complications |
| 23 | Hefnyet al. 2015 [37] | 24 | 9 | Primigravida | Vomiting and severe epigastric pain | Bicornuate uterus | Superior-lateral region | Surgical repair | No complications |
| 24 | Bechemet al. 2016 [38] | 24 | 11 | 2/1 | Exteriorisation of bowel through the vagina | Manual vacuum aspiration | Fundus | Surgical repair | No complications |
| 25 | Vaezi et al. 2017 [39] | 34 | 12 | 2/1 | Acute abdominal pain | Without | The fundus | Surgical repair | No complications |
| 26 | Miranda et L.2017 [40] | 32 | 13 | 3/2 | Acute abdominal pain | Short pregnancy interval and previous scar | The previous scar | Surgical repair | No complications |
| 27 | Surve et al. 2017 [41] | 25 | 10 | 3/1/ab1 | Shock and acute abdominal pain | One previous scar | The previous scar | Surgical repair | No complications |
| 28 | Mosadet al. 2017 [42] | 19 | 11 | 2/1 + 0 | Sudden abdominal pain, severe vaginal bleeding, syncopal attacks | IUCD | N/A | Surgical repair | No complications |
| 29 | Cho et al. 2017 [43] | 34 | 7 | Primigravida | Abdominal pain | Placenta percreta | Fundus | Surgical repair | No complications |
| 30 | Abbas et al. 2018 [44] | 24 | 10 | 3/2 | Shock and acute abdominal pain | Two previous scars | Posterior wall and fundus | Surgical repair | No complications |
| 31 | Abbas et al. 2018 [44] | 27 | 10 | 3/2 | Severe lower abdominal pain and shock | Two previous scars | Previous scar | Surgical repair | No complications. |
| 32 | Ambrogiet al. 2018 [45] | 36 | 9 | 2/1 | Moderete abdominal pain | One previous scar | The back and the right uterine horn | hysterectomy | No complications |
| 33 | Takashimaet al. 2018 [46] | 43 | 11 | 2/1 | Sudden lower abdominal pain | Abdominal myomectomy and Cesarean section | The uterine fundus and cornea of the Cesarean scar | Hysterectomy | No complications |
| 34 | Amro et al. 2019 [47] | 27 | 12 | 4/2 + 1 | Severe lower abdominal pain | Right salpingectomy for tubal pregnancy? | The fundus | Surgical repair | No complications |
| 35 | Amro et al. 2019 [47] | 34 | 6 | 4/1 + 3 | Severe lower abdominal pain | Left-sided salpingectomy for tubal pregnancy? | The fundus | Surgical repair | No complications |
| 36 | Cecchiniet al. 2020 [48] | 35 | 11 | 5/2 | Abdominal pain, fainting, and shock | Two previous cesarean sections | Lower anterior uterine wall | Surgical repair | No complications |
| 37 | Leeet al. 2020 [49] | 28 | 13 | 2/1 | Pain in the right lower quadrant, nausea, and fever | Placenta percreta | Uterine fundus | Total laparoscopic hysterectomy | No complications |
| 38 | Bruandet al. 2020 [50] | 18 | 12 | 2/0 | Abdominal pain | Abortion by vacuum extraction | Uterine horn in the right side | Surgical repair | No complications |
| 39. | Mutiso et al. 2024 [3] | 39 | 11 | 6/4 + 1 | Severe lower abdominal pain, dizziness | Four previous hysterotomy scars | Anterior uterine rupture | Surgical repair | No complications |
| 40 | Faraj et al. 2022 [1] | 28 | 9 | 2/1 | Abdominal pain and metrorrhagia | Previous cesarean scar | In the anterior uterine wall | Surgical repair | No complications |
| . | Author . | Age . | Gestation age . | Gravida/Para/Abortion . | Symptoms . | Risk factors . | Rupture location . | Treatment . | Follow up . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Pridjian et al. 1990 [16] | 23 | 13 | Primigravid | Hypotension, vaginal hemorrhage, abdominal pain | Pelvic irradiation 7 years before | Anterior fundal defect | Supracervical hysterectomy and left salpingo-oophorectomy | N/A |
| 2 | Dibbs et al. 1995 [17] | 29 | 8 | 2/0 | abdominal pain, diarrhea, and lightheadedness | placenta percreta | The fundus | Surgical repair | No complications |
| 3 | Arbab et al. 1996 [18] | 34 | 13 | 8/1/ep5/ab1 | Shock and acute abdominal pain | Placenta percreta, bilateral salpingectomy, left cornual resection | Right-sided uterine cornual rupture | Surgical repair | N/A |
| 4 | Arbab et al. 1996 [18] | 25 | 8 | Ab2/p2 | Hemorrhagic shock | Left cornual resection, bilateral salpingectomy | The fundus | Surgical repair | N/A |
| 5 | Marcuset al. 1999 [19] | 38 | 13 | 4/2-0-1-1 | Spotting and cramping | Two cesarean scars, placenta percreta | The lower uterine segment | Radical hysterectomy | No complications |
| 6 | Hamsho et al. 1999 [20] | 34 | 13 | 4 + 3 | Abdominal pain | Four lower segment cesarean sections | The lower part of its anterior aspect | Surgical repair | No complications |
| 7 | Porcu et al. 2003 [21] | 28 | 12 | 1/0 | Acute abdominal pain | DES | Anterior fundal area | Surgical repair | No complications |
| 8 | deRouxet al. 1999 [22] | 22 | 12 | 9/ | Abdominal pain | 6 curettages, placenta percreta | The fundus | Surgical repair | Died |
| 9 | Matsuoet al. 2004 [23] | 31 | 10 | 3/1 | Little abnormal genital bleeding and mild abdominal pain | Previous cesarean section, dilatation, and curettage | The lower uterine wall | Surgical repair | No complications |
| 10 | Parket al. 2005 [24] | 36 | 10 | *** | Abdominal pain | Without | The upper portion of the left fundus | Surgical repair | N/A |
| 11 | Dabuliset al. 2007 [25] | N/A | 9 | N/A | Abdominal pain, bloating, vomiting, and diarrhea | Three previous cesarean sections | At the site of the prior cesarean section | Hysterectomy | N/A |
| 12 | TANYI et al. 2008 [26] | 32 | 7 | 6/3 | Abdominal pain, vaginal spotting | Right salpingo-oophorectomy Cesarean section curettage, Placenta percreta | 3 cm from the dome of the uterus | Hysterectomy | N/A |
| 13 | Ijaz et al. 2011 [27] | 32 | 8 | 3/1 | Acute abdomen | Manual removal of placenta in a previous pregnancy | The fundus | Surgical repair | No complications |
| 14 | Visariyaet al. 2011 [28] | 26 | 9 | 2/1 | Abdominal pain, giddiness, and shock | Previous cesarean | Lower anterior uterine wall | Surgical repair | No complications |
| 15 | Snigh et al. 2012 [29] | 24 | 10 | Primigravida | Abdominal pain | Bicornuate uterus | Left rudimentary horn | Surgical repair | No complications |
| 16 | Tolaet al. 2014 [30] | 24 | 8 | Multigravida | Vaginal bleeding and generalized abdominal pain | Bicornuate uterus | Left part of the uterus | Left part of the uterus | No complication |
| 17 | Sinha et al. 2014 [31] | 30 | 11 | 6/5 | Syncopal attack, syncopal attack | One cesarian section, history of repair uterine rupture? | Upto the fundus | Surgical repair | No complication |
| 18 | Bandarian et al. 2015 [32] | 30 | 11 | 4/2/ab1 | Shock and acute syncopal attack | D&C, two scars | On the previous scar | Surgical repair | No complication |
| 19 | AKBAŞ et al. 2015 [33] | 36 | 12 | 8/7 | Abdominal pain | Without | At the side of the left uterine vessels extended to the cervix. | Hysterectomy | No complication |
| 20 | Taskin et al. 2015 [34] | 32 | 13 | 2/1 | Pelvic pain | Curettage, one cesarean | Posterior | Surgical repair | No complication |
| 21 | Okada et al. 2015 [35] | 39 | 10 | Primigravida | Abdominal pain and shock | Laparoscopic myomectomy | The fundus | Surgical repair | No complications |
| 22 | Pendy et al. 2015 [36] | 30 | 8 | 3/2 | Acute abdominal pain with hemorrhagic shock | A unicornuate uterus | Rudimentary horn | Surgical repair | No complications |
| 23 | Hefnyet al. 2015 [37] | 24 | 9 | Primigravida | Vomiting and severe epigastric pain | Bicornuate uterus | Superior-lateral region | Surgical repair | No complications |
| 24 | Bechemet al. 2016 [38] | 24 | 11 | 2/1 | Exteriorisation of bowel through the vagina | Manual vacuum aspiration | Fundus | Surgical repair | No complications |
| 25 | Vaezi et al. 2017 [39] | 34 | 12 | 2/1 | Acute abdominal pain | Without | The fundus | Surgical repair | No complications |
| 26 | Miranda et L.2017 [40] | 32 | 13 | 3/2 | Acute abdominal pain | Short pregnancy interval and previous scar | The previous scar | Surgical repair | No complications |
| 27 | Surve et al. 2017 [41] | 25 | 10 | 3/1/ab1 | Shock and acute abdominal pain | One previous scar | The previous scar | Surgical repair | No complications |
| 28 | Mosadet al. 2017 [42] | 19 | 11 | 2/1 + 0 | Sudden abdominal pain, severe vaginal bleeding, syncopal attacks | IUCD | N/A | Surgical repair | No complications |
| 29 | Cho et al. 2017 [43] | 34 | 7 | Primigravida | Abdominal pain | Placenta percreta | Fundus | Surgical repair | No complications |
| 30 | Abbas et al. 2018 [44] | 24 | 10 | 3/2 | Shock and acute abdominal pain | Two previous scars | Posterior wall and fundus | Surgical repair | No complications |
| 31 | Abbas et al. 2018 [44] | 27 | 10 | 3/2 | Severe lower abdominal pain and shock | Two previous scars | Previous scar | Surgical repair | No complications. |
| 32 | Ambrogiet al. 2018 [45] | 36 | 9 | 2/1 | Moderete abdominal pain | One previous scar | The back and the right uterine horn | hysterectomy | No complications |
| 33 | Takashimaet al. 2018 [46] | 43 | 11 | 2/1 | Sudden lower abdominal pain | Abdominal myomectomy and Cesarean section | The uterine fundus and cornea of the Cesarean scar | Hysterectomy | No complications |
| 34 | Amro et al. 2019 [47] | 27 | 12 | 4/2 + 1 | Severe lower abdominal pain | Right salpingectomy for tubal pregnancy? | The fundus | Surgical repair | No complications |
| 35 | Amro et al. 2019 [47] | 34 | 6 | 4/1 + 3 | Severe lower abdominal pain | Left-sided salpingectomy for tubal pregnancy? | The fundus | Surgical repair | No complications |
| 36 | Cecchiniet al. 2020 [48] | 35 | 11 | 5/2 | Abdominal pain, fainting, and shock | Two previous cesarean sections | Lower anterior uterine wall | Surgical repair | No complications |
| 37 | Leeet al. 2020 [49] | 28 | 13 | 2/1 | Pain in the right lower quadrant, nausea, and fever | Placenta percreta | Uterine fundus | Total laparoscopic hysterectomy | No complications |
| 38 | Bruandet al. 2020 [50] | 18 | 12 | 2/0 | Abdominal pain | Abortion by vacuum extraction | Uterine horn in the right side | Surgical repair | No complications |
| 39. | Mutiso et al. 2024 [3] | 39 | 11 | 6/4 + 1 | Severe lower abdominal pain, dizziness | Four previous hysterotomy scars | Anterior uterine rupture | Surgical repair | No complications |
| 40 | Faraj et al. 2022 [1] | 28 | 9 | 2/1 | Abdominal pain and metrorrhagia | Previous cesarean scar | In the anterior uterine wall | Surgical repair | No complications |
| . | Author . | Age . | Gestation age . | Gravida/Para/Abortion . | Symptoms . | Risk factors . | Rupture location . | Treatment . | Follow up . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Pridjian et al. 1990 [16] | 23 | 13 | Primigravid | Hypotension, vaginal hemorrhage, abdominal pain | Pelvic irradiation 7 years before | Anterior fundal defect | Supracervical hysterectomy and left salpingo-oophorectomy | N/A |
| 2 | Dibbs et al. 1995 [17] | 29 | 8 | 2/0 | abdominal pain, diarrhea, and lightheadedness | placenta percreta | The fundus | Surgical repair | No complications |
| 3 | Arbab et al. 1996 [18] | 34 | 13 | 8/1/ep5/ab1 | Shock and acute abdominal pain | Placenta percreta, bilateral salpingectomy, left cornual resection | Right-sided uterine cornual rupture | Surgical repair | N/A |
| 4 | Arbab et al. 1996 [18] | 25 | 8 | Ab2/p2 | Hemorrhagic shock | Left cornual resection, bilateral salpingectomy | The fundus | Surgical repair | N/A |
| 5 | Marcuset al. 1999 [19] | 38 | 13 | 4/2-0-1-1 | Spotting and cramping | Two cesarean scars, placenta percreta | The lower uterine segment | Radical hysterectomy | No complications |
| 6 | Hamsho et al. 1999 [20] | 34 | 13 | 4 + 3 | Abdominal pain | Four lower segment cesarean sections | The lower part of its anterior aspect | Surgical repair | No complications |
| 7 | Porcu et al. 2003 [21] | 28 | 12 | 1/0 | Acute abdominal pain | DES | Anterior fundal area | Surgical repair | No complications |
| 8 | deRouxet al. 1999 [22] | 22 | 12 | 9/ | Abdominal pain | 6 curettages, placenta percreta | The fundus | Surgical repair | Died |
| 9 | Matsuoet al. 2004 [23] | 31 | 10 | 3/1 | Little abnormal genital bleeding and mild abdominal pain | Previous cesarean section, dilatation, and curettage | The lower uterine wall | Surgical repair | No complications |
| 10 | Parket al. 2005 [24] | 36 | 10 | *** | Abdominal pain | Without | The upper portion of the left fundus | Surgical repair | N/A |
| 11 | Dabuliset al. 2007 [25] | N/A | 9 | N/A | Abdominal pain, bloating, vomiting, and diarrhea | Three previous cesarean sections | At the site of the prior cesarean section | Hysterectomy | N/A |
| 12 | TANYI et al. 2008 [26] | 32 | 7 | 6/3 | Abdominal pain, vaginal spotting | Right salpingo-oophorectomy Cesarean section curettage, Placenta percreta | 3 cm from the dome of the uterus | Hysterectomy | N/A |
| 13 | Ijaz et al. 2011 [27] | 32 | 8 | 3/1 | Acute abdomen | Manual removal of placenta in a previous pregnancy | The fundus | Surgical repair | No complications |
| 14 | Visariyaet al. 2011 [28] | 26 | 9 | 2/1 | Abdominal pain, giddiness, and shock | Previous cesarean | Lower anterior uterine wall | Surgical repair | No complications |
| 15 | Snigh et al. 2012 [29] | 24 | 10 | Primigravida | Abdominal pain | Bicornuate uterus | Left rudimentary horn | Surgical repair | No complications |
| 16 | Tolaet al. 2014 [30] | 24 | 8 | Multigravida | Vaginal bleeding and generalized abdominal pain | Bicornuate uterus | Left part of the uterus | Left part of the uterus | No complication |
| 17 | Sinha et al. 2014 [31] | 30 | 11 | 6/5 | Syncopal attack, syncopal attack | One cesarian section, history of repair uterine rupture? | Upto the fundus | Surgical repair | No complication |
| 18 | Bandarian et al. 2015 [32] | 30 | 11 | 4/2/ab1 | Shock and acute syncopal attack | D&C, two scars | On the previous scar | Surgical repair | No complication |
| 19 | AKBAŞ et al. 2015 [33] | 36 | 12 | 8/7 | Abdominal pain | Without | At the side of the left uterine vessels extended to the cervix. | Hysterectomy | No complication |
| 20 | Taskin et al. 2015 [34] | 32 | 13 | 2/1 | Pelvic pain | Curettage, one cesarean | Posterior | Surgical repair | No complication |
| 21 | Okada et al. 2015 [35] | 39 | 10 | Primigravida | Abdominal pain and shock | Laparoscopic myomectomy | The fundus | Surgical repair | No complications |
| 22 | Pendy et al. 2015 [36] | 30 | 8 | 3/2 | Acute abdominal pain with hemorrhagic shock | A unicornuate uterus | Rudimentary horn | Surgical repair | No complications |
| 23 | Hefnyet al. 2015 [37] | 24 | 9 | Primigravida | Vomiting and severe epigastric pain | Bicornuate uterus | Superior-lateral region | Surgical repair | No complications |
| 24 | Bechemet al. 2016 [38] | 24 | 11 | 2/1 | Exteriorisation of bowel through the vagina | Manual vacuum aspiration | Fundus | Surgical repair | No complications |
| 25 | Vaezi et al. 2017 [39] | 34 | 12 | 2/1 | Acute abdominal pain | Without | The fundus | Surgical repair | No complications |
| 26 | Miranda et L.2017 [40] | 32 | 13 | 3/2 | Acute abdominal pain | Short pregnancy interval and previous scar | The previous scar | Surgical repair | No complications |
| 27 | Surve et al. 2017 [41] | 25 | 10 | 3/1/ab1 | Shock and acute abdominal pain | One previous scar | The previous scar | Surgical repair | No complications |
| 28 | Mosadet al. 2017 [42] | 19 | 11 | 2/1 + 0 | Sudden abdominal pain, severe vaginal bleeding, syncopal attacks | IUCD | N/A | Surgical repair | No complications |
| 29 | Cho et al. 2017 [43] | 34 | 7 | Primigravida | Abdominal pain | Placenta percreta | Fundus | Surgical repair | No complications |
| 30 | Abbas et al. 2018 [44] | 24 | 10 | 3/2 | Shock and acute abdominal pain | Two previous scars | Posterior wall and fundus | Surgical repair | No complications |
| 31 | Abbas et al. 2018 [44] | 27 | 10 | 3/2 | Severe lower abdominal pain and shock | Two previous scars | Previous scar | Surgical repair | No complications. |
| 32 | Ambrogiet al. 2018 [45] | 36 | 9 | 2/1 | Moderete abdominal pain | One previous scar | The back and the right uterine horn | hysterectomy | No complications |
| 33 | Takashimaet al. 2018 [46] | 43 | 11 | 2/1 | Sudden lower abdominal pain | Abdominal myomectomy and Cesarean section | The uterine fundus and cornea of the Cesarean scar | Hysterectomy | No complications |
| 34 | Amro et al. 2019 [47] | 27 | 12 | 4/2 + 1 | Severe lower abdominal pain | Right salpingectomy for tubal pregnancy? | The fundus | Surgical repair | No complications |
| 35 | Amro et al. 2019 [47] | 34 | 6 | 4/1 + 3 | Severe lower abdominal pain | Left-sided salpingectomy for tubal pregnancy? | The fundus | Surgical repair | No complications |
| 36 | Cecchiniet al. 2020 [48] | 35 | 11 | 5/2 | Abdominal pain, fainting, and shock | Two previous cesarean sections | Lower anterior uterine wall | Surgical repair | No complications |
| 37 | Leeet al. 2020 [49] | 28 | 13 | 2/1 | Pain in the right lower quadrant, nausea, and fever | Placenta percreta | Uterine fundus | Total laparoscopic hysterectomy | No complications |
| 38 | Bruandet al. 2020 [50] | 18 | 12 | 2/0 | Abdominal pain | Abortion by vacuum extraction | Uterine horn in the right side | Surgical repair | No complications |
| 39. | Mutiso et al. 2024 [3] | 39 | 11 | 6/4 + 1 | Severe lower abdominal pain, dizziness | Four previous hysterotomy scars | Anterior uterine rupture | Surgical repair | No complications |
| 40 | Faraj et al. 2022 [1] | 28 | 9 | 2/1 | Abdominal pain and metrorrhagia | Previous cesarean scar | In the anterior uterine wall | Surgical repair | No complications |
| . | Author . | Age . | Gestation age . | Gravida/Para/Abortion . | Symptoms . | Risk factors . | Rupture location . | Treatment . | Follow up . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Pridjian et al. 1990 [16] | 23 | 13 | Primigravid | Hypotension, vaginal hemorrhage, abdominal pain | Pelvic irradiation 7 years before | Anterior fundal defect | Supracervical hysterectomy and left salpingo-oophorectomy | N/A |
| 2 | Dibbs et al. 1995 [17] | 29 | 8 | 2/0 | abdominal pain, diarrhea, and lightheadedness | placenta percreta | The fundus | Surgical repair | No complications |
| 3 | Arbab et al. 1996 [18] | 34 | 13 | 8/1/ep5/ab1 | Shock and acute abdominal pain | Placenta percreta, bilateral salpingectomy, left cornual resection | Right-sided uterine cornual rupture | Surgical repair | N/A |
| 4 | Arbab et al. 1996 [18] | 25 | 8 | Ab2/p2 | Hemorrhagic shock | Left cornual resection, bilateral salpingectomy | The fundus | Surgical repair | N/A |
| 5 | Marcuset al. 1999 [19] | 38 | 13 | 4/2-0-1-1 | Spotting and cramping | Two cesarean scars, placenta percreta | The lower uterine segment | Radical hysterectomy | No complications |
| 6 | Hamsho et al. 1999 [20] | 34 | 13 | 4 + 3 | Abdominal pain | Four lower segment cesarean sections | The lower part of its anterior aspect | Surgical repair | No complications |
| 7 | Porcu et al. 2003 [21] | 28 | 12 | 1/0 | Acute abdominal pain | DES | Anterior fundal area | Surgical repair | No complications |
| 8 | deRouxet al. 1999 [22] | 22 | 12 | 9/ | Abdominal pain | 6 curettages, placenta percreta | The fundus | Surgical repair | Died |
| 9 | Matsuoet al. 2004 [23] | 31 | 10 | 3/1 | Little abnormal genital bleeding and mild abdominal pain | Previous cesarean section, dilatation, and curettage | The lower uterine wall | Surgical repair | No complications |
| 10 | Parket al. 2005 [24] | 36 | 10 | *** | Abdominal pain | Without | The upper portion of the left fundus | Surgical repair | N/A |
| 11 | Dabuliset al. 2007 [25] | N/A | 9 | N/A | Abdominal pain, bloating, vomiting, and diarrhea | Three previous cesarean sections | At the site of the prior cesarean section | Hysterectomy | N/A |
| 12 | TANYI et al. 2008 [26] | 32 | 7 | 6/3 | Abdominal pain, vaginal spotting | Right salpingo-oophorectomy Cesarean section curettage, Placenta percreta | 3 cm from the dome of the uterus | Hysterectomy | N/A |
| 13 | Ijaz et al. 2011 [27] | 32 | 8 | 3/1 | Acute abdomen | Manual removal of placenta in a previous pregnancy | The fundus | Surgical repair | No complications |
| 14 | Visariyaet al. 2011 [28] | 26 | 9 | 2/1 | Abdominal pain, giddiness, and shock | Previous cesarean | Lower anterior uterine wall | Surgical repair | No complications |
| 15 | Snigh et al. 2012 [29] | 24 | 10 | Primigravida | Abdominal pain | Bicornuate uterus | Left rudimentary horn | Surgical repair | No complications |
| 16 | Tolaet al. 2014 [30] | 24 | 8 | Multigravida | Vaginal bleeding and generalized abdominal pain | Bicornuate uterus | Left part of the uterus | Left part of the uterus | No complication |
| 17 | Sinha et al. 2014 [31] | 30 | 11 | 6/5 | Syncopal attack, syncopal attack | One cesarian section, history of repair uterine rupture? | Upto the fundus | Surgical repair | No complication |
| 18 | Bandarian et al. 2015 [32] | 30 | 11 | 4/2/ab1 | Shock and acute syncopal attack | D&C, two scars | On the previous scar | Surgical repair | No complication |
| 19 | AKBAŞ et al. 2015 [33] | 36 | 12 | 8/7 | Abdominal pain | Without | At the side of the left uterine vessels extended to the cervix. | Hysterectomy | No complication |
| 20 | Taskin et al. 2015 [34] | 32 | 13 | 2/1 | Pelvic pain | Curettage, one cesarean | Posterior | Surgical repair | No complication |
| 21 | Okada et al. 2015 [35] | 39 | 10 | Primigravida | Abdominal pain and shock | Laparoscopic myomectomy | The fundus | Surgical repair | No complications |
| 22 | Pendy et al. 2015 [36] | 30 | 8 | 3/2 | Acute abdominal pain with hemorrhagic shock | A unicornuate uterus | Rudimentary horn | Surgical repair | No complications |
| 23 | Hefnyet al. 2015 [37] | 24 | 9 | Primigravida | Vomiting and severe epigastric pain | Bicornuate uterus | Superior-lateral region | Surgical repair | No complications |
| 24 | Bechemet al. 2016 [38] | 24 | 11 | 2/1 | Exteriorisation of bowel through the vagina | Manual vacuum aspiration | Fundus | Surgical repair | No complications |
| 25 | Vaezi et al. 2017 [39] | 34 | 12 | 2/1 | Acute abdominal pain | Without | The fundus | Surgical repair | No complications |
| 26 | Miranda et L.2017 [40] | 32 | 13 | 3/2 | Acute abdominal pain | Short pregnancy interval and previous scar | The previous scar | Surgical repair | No complications |
| 27 | Surve et al. 2017 [41] | 25 | 10 | 3/1/ab1 | Shock and acute abdominal pain | One previous scar | The previous scar | Surgical repair | No complications |
| 28 | Mosadet al. 2017 [42] | 19 | 11 | 2/1 + 0 | Sudden abdominal pain, severe vaginal bleeding, syncopal attacks | IUCD | N/A | Surgical repair | No complications |
| 29 | Cho et al. 2017 [43] | 34 | 7 | Primigravida | Abdominal pain | Placenta percreta | Fundus | Surgical repair | No complications |
| 30 | Abbas et al. 2018 [44] | 24 | 10 | 3/2 | Shock and acute abdominal pain | Two previous scars | Posterior wall and fundus | Surgical repair | No complications |
| 31 | Abbas et al. 2018 [44] | 27 | 10 | 3/2 | Severe lower abdominal pain and shock | Two previous scars | Previous scar | Surgical repair | No complications. |
| 32 | Ambrogiet al. 2018 [45] | 36 | 9 | 2/1 | Moderete abdominal pain | One previous scar | The back and the right uterine horn | hysterectomy | No complications |
| 33 | Takashimaet al. 2018 [46] | 43 | 11 | 2/1 | Sudden lower abdominal pain | Abdominal myomectomy and Cesarean section | The uterine fundus and cornea of the Cesarean scar | Hysterectomy | No complications |
| 34 | Amro et al. 2019 [47] | 27 | 12 | 4/2 + 1 | Severe lower abdominal pain | Right salpingectomy for tubal pregnancy? | The fundus | Surgical repair | No complications |
| 35 | Amro et al. 2019 [47] | 34 | 6 | 4/1 + 3 | Severe lower abdominal pain | Left-sided salpingectomy for tubal pregnancy? | The fundus | Surgical repair | No complications |
| 36 | Cecchiniet al. 2020 [48] | 35 | 11 | 5/2 | Abdominal pain, fainting, and shock | Two previous cesarean sections | Lower anterior uterine wall | Surgical repair | No complications |
| 37 | Leeet al. 2020 [49] | 28 | 13 | 2/1 | Pain in the right lower quadrant, nausea, and fever | Placenta percreta | Uterine fundus | Total laparoscopic hysterectomy | No complications |
| 38 | Bruandet al. 2020 [50] | 18 | 12 | 2/0 | Abdominal pain | Abortion by vacuum extraction | Uterine horn in the right side | Surgical repair | No complications |
| 39. | Mutiso et al. 2024 [3] | 39 | 11 | 6/4 + 1 | Severe lower abdominal pain, dizziness | Four previous hysterotomy scars | Anterior uterine rupture | Surgical repair | No complications |
| 40 | Faraj et al. 2022 [1] | 28 | 9 | 2/1 | Abdominal pain and metrorrhagia | Previous cesarean scar | In the anterior uterine wall | Surgical repair | No complications |
In most cases, the rupture was localized in the fundus of the uterus (15/40).
In all cases, surgery was resorted to, whether through repair or radical excision, and in all cases, no complications were observed except for one patient who died due to hemorrhagic shock [22].
Conclusion
Women who are pregnant and primarily in the first trimester with a history of cesarean sections should receive extra care. Uterine ruptures should be taken into mind, particularly when risk factors including a history of cesarean delivery, myomectomy, or uterine scarring are present. In addition, when symptoms like pain in the abdomen appear, uterine rupture should be considered, and it is crucial to confirm that there is no free fluid in the Douglas pouch to protect the patient.



