-
PDF
- Split View
-
Views
-
Cite
Cite
S Premakrishna, Sreekanthan Gobishangar, Jude Selvakumar Nilojan, Gnanapragasam Vaikunthan, Jothini Thirunavukkarasu, Pneumo-peritoneum, pneumo-retroperitoneum and subcutaneous emphysema following endoscopic retrograde cholangiopancreatography with sphincterotomy—an uncommon complication case report, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae415, https://doi.org/10.1093/jscr/rjae415
Close - Share Icon Share
Abstract
Endoscopic retrograde cholangiopancreatography (ERCP) is invasive for pancreaticobiliary diseases. Perforation is a rare but severe complication among its associated risks. A 45-year-old female with biliary colic and multiple gallbladder calculi was diagnosed with choledocholithiasis based on imaging showing CBD dilation and gallstones. ERCP was planned for stone removal. Sphincterotomy was performed, but stone retrieval attempts failed, leading to severe pneumo-peritoneum and respiratory compromise. Immediate CBD stenting was done, avoiding surgical intervention. The patient recovered uneventfully, later undergoing laparoscopic cholecystectomy with CBD exploration and stone removal. ERCP-related perforations, rare but severe, involve retroperitoneal air collection. Clinical signs include abdominal discomfort, and imaging confirms diagnosis. Management varies by type, with some requiring surgical repair. Conservative management sufficed in this case, with successful patient recovery. ERCP-related complications like pneumo-peritoneum require prompt diagnosis and conservative management if no perforation is evident.
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is a well-established technique for diagnosing and treating pancreatic and extra-hepatic biliary tract diseases [1]. It is an invasive procedure, and ERCP has several complications [2]. The complications of ERCP are pancreatitis (1.3–5.4%), cholangitis(0.87–1%), bleeding (0.76–3%), perforation(0.3–2.1%) ,and issues related to biliary stents and lithiasis treatment [3–6]. The main risk factors for the complications are difficult bile duct cannulation, continuous air insufflation, repeated attempts to cannulate the papilla, duration of the procedure, cirrhosis, sphincter of Oddi dysfunction, and previous gastrointestinal surgery. Perforation and air leakage is an uncommon complication but associated with a high mortality rate [2, 7] It originates from injury of the duodenum and small bowel or extrahepatic bile duct system as a direct consequence of hollow organ wall perforation or ruptured alveoli. Rare complications, such as pneumo-peritonium, pneumo-retroperitoneum, and subcutaneous emphysema, related to this procedure are reported in this case report.
Case presentation
A 45-year-old female presented with a history of intermittent right hypochondrial pain and dyspepsia for 18 months, which worsened over the last one1-month period. Her abdominal examination was unremarkable.
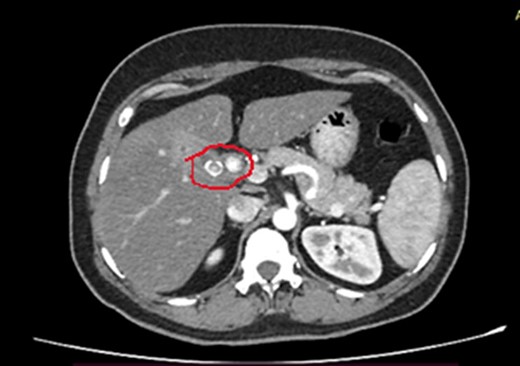
Laboratory investigations showed WBC 13.85 × 106, neutrophils 7.59, Hb 12.8 g/dl, platelet count 287 000 × 106, CRP 6.3, PT/INR 0.85, AST 75, ALT 53, ALP 88, and total bilirubin 12.0 mg/dl. Her ultrasound scan of the abdomen showed multiple common bile duct (CBD) calculi with intrahepatic and CBD dilatation with mild central cholangitis. Contrast-enhanced computed tomography (CECT) of the abdomen showed proximal CBD calculus with mild common hepatic and intra-hepatic duct dilation and gallstone with chronic cholecystitis (Fig. 1).
She has undergone a semi-elective ERCP in a semi-prone position, under sedation with propofol target-controlled infusion. Major papillae identified with side viewing endoscopy. Guidewire was inserted into CBD, and a cholangiogram was done. It showed dilated CBD up to 1.3 cm, mild dilated hepatic ducts, and a large radiolucent area in the distal CBD (around 1.5 cm). Sphincterotomy was done with a sphincterotome, and the ampulla was dilated up to 1.5 cm with a balloon dilator. Then, a balloon retrieval was attempted and failed, probably due to a stone sticking to the CBD wall. Then, a mechanical lithotripter was used to break the stone, but it failed, damaging the instrument. During the procedure, her oxygen saturation dropped to 75–80%, and she developed surgical emphysema in the face, neck, and upper chest region. In addition, she developed abdominal distention as well. Immediately, she underwent CBD stenting with a 12-cm, 10 French Gauge double pigtail biliary stent and changed her position to supine. Then, she was intubated with rapid sequence induction, and a nasogastric tube was inserted and transferred to the surgical intensive care unit. Post-ERCP, non-contrast computed tomography (NCCT) of the abdomen and chest showed extensive pneumo-peritoneum and retroperitoneal gas with subcutaneous emphysema (Figs 2 and 3). There was no evidence of air leakage on NCCT and no clinical features of peritonitis on subsequent days. So she was managed non-surgically with nasogastric tube (NG), nil by mouth, intravenous fluids with intravenous antibiotics. Clear fluid was started after 24 hours slowly via NG.
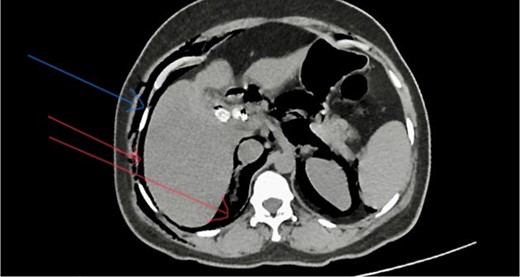
Post-ERCP NCCT abdomen shows pneumo-peritoneum (red arrow), pneumo-retroperitoneum, and subcutaneous emphysema (blue arrow)
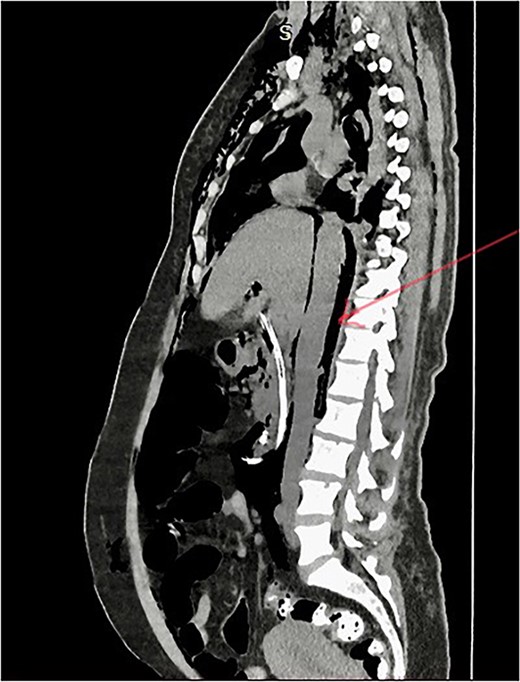
Post-ERCP NCCT abdomen shows pneumo-retroperitoneum (red arrow).
Extension of pneumo-peritoneum and subcutaneous emphysema reduced on following days. She was extubated on the third day. Oral fluid was started on day 3, and she took a regular diet on day 5. The patient’s further clinical course was uncomplicated, and she fully recovered. She was discharged on day 7. Six weeks later, laparoscopic cholecystectomy and CBD exploration with stone removal were performed, and she was discharged on post-operative day two with an uneventful recovery.
Discussion
ERCP-related complications depend on several factors. These factors can be categorized into patient-related, procedure-related, and endoscopist-related risk factors [8]. The severity of the complications determines the management and treatment strategies [1, 9].
Perforation is one of the rare complications, but it is a severe complication, even with life-threatening conditions [7, 10] The significant risk factors for ERCP-related perforation are sphincter of Oddi dysfunction (SOD), Billroth II anatomy, intramural injection of contrast, prolonged duration of the procedure, biliary stricture dilation, the experience of the endoscopist, and other anatomical anomalies [7, 11].
ERCP-related perforations can be classified according to the Howard classification and Stapfer classification [12]. According to Howard’s classification, group 1 perforation is guidewire-associated, group 2 is periampullary perforation, and group 3 is duodenal perforation [6]. Stapfer classification is based on anatomical location and severity [2]. In this classification, there are four types of perforations. Type 1 is lateral or medial duodenal wall perforations produced by a metal guide; type 2 is periampullary perforations due to sphincterotomy; type 3 is bile duct or pancreatic duct perforations related to instrumentations; and type 4 is associated with retro pneumo-peritoneum post-ERCP, which may not represent true perforations [6, 8].
Perforation after ERCP usually occurs in the retroperitoneal portion of the duodenum and results in the retroperitoneal collection of free air [2]. Retroperitoneal perforation is generally related to extensive sphincterotomy beyond the intramural portion of the bile and pancreatic ducts. It is classically manifested by abdominal pain, restlessness, tachycardia, hypoxemia, or subcutaneous emphysema [3, 9]. After a retroperitoneal perforation, free air escapes from the duodenum to the right anterior pararenal space. The air flows to the posterior para-renal compartment, which can quickly spread along the facial planes to subcutaneous tissue, leading to subcutaneous emphysema or diffusing to the mediastinum, causing pneumo-mediastinum. Finally, mediastinal air can access the pleural cavity due to a rupture of the parietal pleura [8]. Pneumo-thorax is usually right-sided or bilateral and accompanied by pneumo-mediastinum, pneumo-retroperitoneum, and subcutaneous emphysema [13]. In this case, the patient developed pneumo-peritoneum, pneumo-retroperitoneum, and surgical emphysema related to ERCP.
Early recognition of clinical features, interpretation of imaging investigations, and early management are essential to reduce the morbidity and mortality associated with perforation [14]. The clinical features of ERCP-related perforations are abdominal discomfort, tenderness, signs of peritonitis, low-grade fever, and tachycardia [12]. Abdominal X-rays and CT scans are used in imaging investigations, and a CT scan is a confirmatory investigation [6].
Management of ERCP-related complications depends on the type of perforation and the patient’s clinical condition. Type 1 perforations are managed with surgical repair [15]. Type 2 perforations are mainly managed conservatively, but some cases with clinical findings of peritoneal signs and sepsis and those with retroperitoneal or peritoneal fluid on CT require surgical repair [15]. Type 3 perforations are usually managed conservatively. Type 4 perforations are also generally managed conservatively, as these are no actual perforations [6, 14] In this case, the patient developed surgical emphysema and abdominal distention suggestive of perforation. She developed respiratory compromise due to pneumo-peritoneum, and her oxygen saturation was dropped during the time of procedure. Therefore, the clinical diagnosis of perforation was made, and the patient was intubated and managed conservatively in the ICU during the post-ERCP period without any need for surgical perforation repair. Post-ERCP, NCCT showed extensive pneumo-peritoneum and retroperitoneal gas with surgical emphysema.
Conclusion
Retroperitoneal air collection related to ERCP is well recognized, even without apparent perforation. A massive pneumo-retroperitoneum and peritoneum due to ERCP without apparent perforation and biliary or gastric juice leakage can be safely managed with conservative management. It needs a series of assessments, and any deterioration can be escalated to laparoscopy or laparotomy.
Conflict of interest statement
None declared.
Funding
No funding was provided.



