-
PDF
- Split View
-
Views
-
Cite
Cite
Jieun Kim, Jung-A Yun, Sangmin Youn, Mi-Ok Park, Endometriosis presenting as a perianal abscess: case report, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae402, https://doi.org/10.1093/jscr/rjae402
Close - Share Icon Share
Abstract
Endometriosis is common benign disorder characterized by the presence of endometrial glands and stroma outside the uterine cavity. Endometriosis of perianal region is a rare condition. We report a case of perianal endometriosis presenting initially as a perianal abscess. Transperineal ultrasound showed a 1.5 cm size irregular mixed echogenicity lesion without involving anal sphincters. Complete surgical excision was performed. The histopathological examination confirmed as endometriosis.
Introduction
Endometriosis is a common benign disorder characterized by the presence of endometrial glands and stroma outside the uterine cavity [1]. It frequently occurs within the pelvic cavity such as ovaries, fallopian tubes, pelvic peritoneum, bowel, and rectovaginal septum. Extra-pelvic endometriosis is a relatively uncommon condition described in various sites such as appendix, abdominal wall, and surgical incisions. Perianal endometriosis is a rare condition usually associated with episiotomy scars [2–4]. Perianal endometriosis is rarely suspected as a differential diagnosis of recurrent painful swelling of perianal region.
Case report
A 37 year old female visited outpatient clinic reporting pain and palpable growing nodule in perianal region. She first noticed nodule in 9 months ago, ineffectively treated with antibiotics. She complained of swelling and pain without purulent discharge aggravated in recent 2 weeks. There was no change in the severity of symptoms in relation to the menstrual cycle. She did not have dysmenorrhea nor difficulty in defecation. She had no past medical history other than full term vaginal delivery with episiotomy 5 years before.
Physical examination showed 1.5 cm size hard tender swelling at perianal area at 11 o’clock position. Episiotomy scar was showed at the lateral side of the swelling. Laboratory tests including complete blood count, inflammatory markers were within normal limits. Viral markers for hepatitis B and serologic studies of an immunocompromised state were all negative. Anoscopic exam showed mild internal hemorrhoids with normal rectal mucosa. Endoanal ultrasound showed normal findings with no evidence of abscess or fistula. Transperineal ultrasound showed a 1.5 cm size irregular mixed echogenicity lesion without involving anal sphincters (Fig. 1). The patient underwent wide excision under local anesthesia. The incision was made with the previous episiotomy scar. 1.5 cm size fibrotic whitish mass with chocolate brown color spots was obtained. Histopathological examination showed several irregular dilated endometrial glands along with stroma in perineal tissue, confirmed as endometriosis (Fig. 2). The postoperative course was uneventful. She had no evidence of recurrence of 6 months follow up.
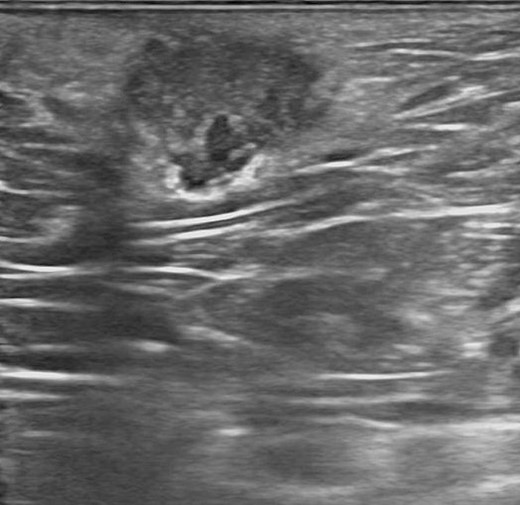
Transperineal ultrasound showed a 1.5 cm size irregular mixed echogenicity lesion.
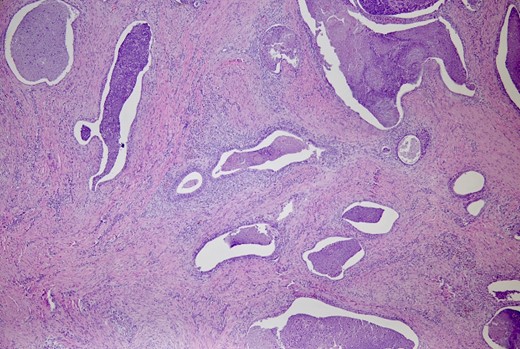
The perineal tissue shows several irregularly dilated endometrial glands along with stroma. (H&E, ×40)
Discussion
Recurrent painful swelling in perianal region is a common medical condition encountered [5]. Clinicians are more likely to suspect common problems such as anal fistula, Crohn’s disease, hidradenitis suppurativa, Bartholin’s abscess, etc. Perianal endometriosis is rarely suspected as a differential diagnosis, which could lead to unnecessary investigations and delay in diagnosis [6]. It is hard to make a suspicion, if there is no visible scar in the perineum, or patient does not have cyclic pain [4, 5]. The most of the case reported in the perianal region, associated with episiotomy site after vaginal delivery [2–4, 7]. However, there was one case of perianal endometriosis reported in a nulliparous patient [3]. In our case, the patient had an episiotomy scar but did not experience cyclic pain. Instead, she complained of persistent, increasing pain, which is a common finding in perianal abscesses.
The pathogenesis of perianal endometriosis is unclear [1]. Diagnosis of endometriosis is difficult due to nonspecific symptoms and lack of clinical relevant biomarkers. Histopathological verification is the only method of confirming endometriosis, which adds to challenge. Endoanal and transperineal ultrasound are important tools for characterizing the lesion and its relationship with the anal sphincters [8].
Complete surgical excision has been shown to be an effective treatment method to prevent recurrence; however, when it involves the anal sphincter, the treatment could become complicated. There are several reports regarding the involvement of anal sphincters in perianal endometriosis [2–4, 7]. However, it is hard to make a generalized consensus due to limited sample size of ~30 cases. Narrow excision with postoperative hormonal therapy had been tried in the literature [3, 7]. Wide excision with primary sphincteroplasty is recommended to decrease the risk of postoperative fecal incontinence [2–4, 7].
Luckily, this case did not involve anal sphincter muscles. Early recognition and complete surgical excision are the best possible strategies in perianal endometriosis. A strong clinical suspicion is needed to consider perianal endometriosis as a differential diagnosis for recurrent perianal painful swellings in female patient.



