-
PDF
- Split View
-
Views
-
Cite
Cite
Indranil Chatterjee, Utpal De, Bouveret’s syndrome: a rare presentation of a common surgical enigma, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae379, https://doi.org/10.1093/jscr/rjae379
Close - Share Icon Share
Abstract
Bouveret syndrome, an uncommon complication of cholelithiasis, typically manifests with symptoms of gastric outlet obstruction. Despite its rarity, Bouveret syndrome carries significant morbidity and mortality. This paper presents a case study and explores diagnostic approaches and management options for this challenging condition.
Introduction
Gallstone disease affects 4% of the Indian population, with a surge in prevalence (20%–35%) by age 70 [1]. About 25%–30% of these cases progress to symptomatic gallstone disease [1]. The development of symptoms and complications (6%) is influenced by stone number, size, cystic duct diameter, and disease duration. Advanced age, female sex (65%), and diabetes often exacerbate these conditions [2]. Stones under 2 cm can navigate the cystic duct, causing issues ranging from obstructive jaundice to biliary pancreatitis. Larger impassable stones (>2.5 cm) lead to compressive ischemic necrosis and fistulous communications (0.3%–5%), resulting in conditions like Mirizzi’s syndrome (0.05%–4%) or gallstone ileus (0.03%–0.5%) [1, 2]. Additionally, altered gastrointestinal anatomy, whether congenital, pathological, or post-surgical, contributes to these complications [1–3]. Bouveret’s syndrome is a unique form of gallstone ileus characterized by proximal obstruction rather than distal obstruction [1]. A literature review disclosed 300 reported cases worldwide, with only 11 documented in India [2].
Case report
A 70-year-old male presented to the OPD with a 3-day history of abdominal pain and projectile vomiting. Since the last 2 days, he experienced complete obstipation. The patient was hypertensive, diabetic, and dyslipidemic, undergoing treatment for these conditions.
A clinical examination revealed tachycardia and dehydration. Abdominal examination showed diffuse tenderness in the upper abdomen, with rigidity over the epigastrium and umbilical region. The patient was initiated on nasogastric suction, and intravenous fluids were administered. Hematological investigations demonstrated an elevated total count (16 000/cm), with increased levels of amylase (540 I.U) and lipase (960 I.U). Blood urea was elevated (45 mg/dl) with borderline creatinine levels (1.2 mg/dl). Liver function tests and serum electrolytes were normal. A provisional diagnosis of acute pancreatitis was considered.
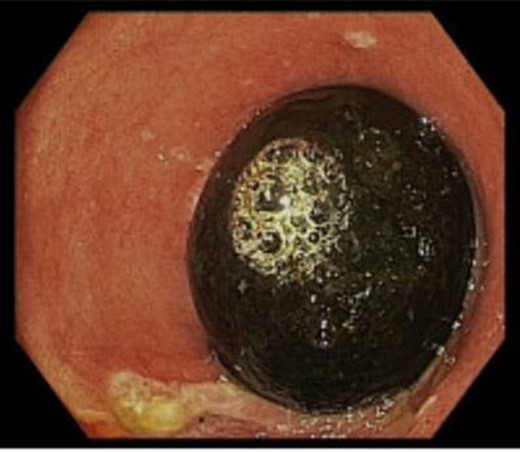
Abdominal sonography revealed a distended gall bladder filled with sludge and a grossly distended stomach. Upper GI endoscopy uncovered residual food, and a peeping gallstone impacted distal to the pyloric ring, indicating BS (Fig. 1). Endoscopic disimpaction was unsuccessful. Computed tomography and MR cholangiography confirmed a large gallstone, causing a cholecystoenteric fistula with significant inflammatory changes and gastric outlet obstruction (Fig. 2).
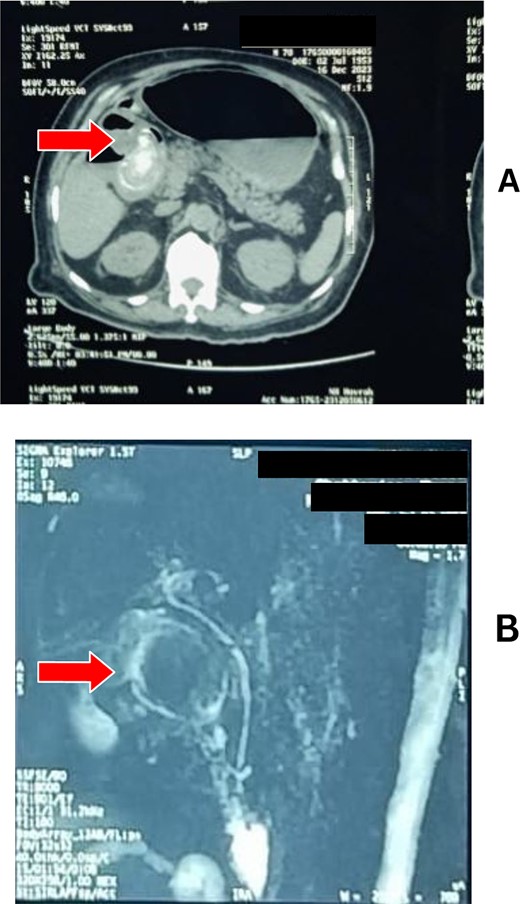
(A) CT scan and (B) MRCP showing a hugely distended stomach with a gallstone obstructing the pylorus.
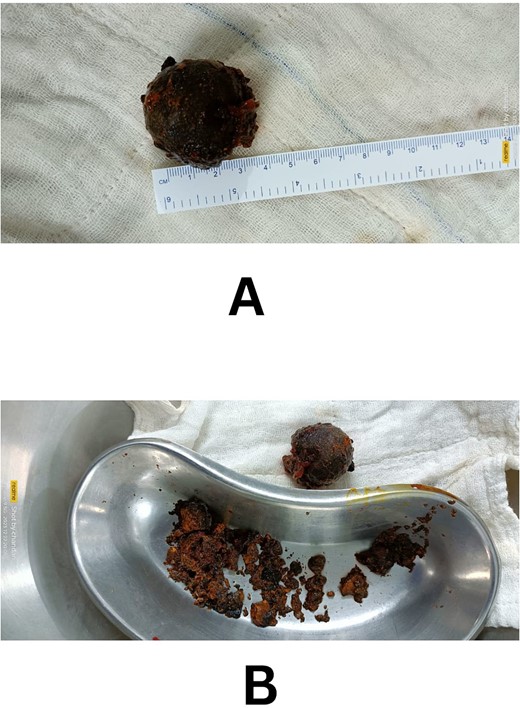
Laparotomy revealed extensive adhesions covering the gall bladder fossa, with the duodenum and colon involved in dense adhesion. The area was edematous and friable. A gastrotomy was performed, and after gentle manipulation, the stone was fragmented and delivered through the pylorus (Fig. 3). No attempt was made to dismantle the fistulous tract. A biopsy from the pylorus was sent. The gastrotomy was closed, and the patient had an uneventful recovery and was discharged on the tenth postoperative day after stitch removal.
At the 2-month follow-up, the patient is stable. The biopsy report indicates gastritis, and the patient was advised to revisit in 6 months for a repeat exploration, management of the fistulous tract, and cholecystectomy.
Discussion
Bouveret syndrome, named after French physician Leon Bouveret (1896), is characterized by gastric outlet obstruction from a gallstone impacted at the gastric outlet or duodenum through a cholecystoenteric fistula (0.3%–5%) [4]. It constitutes 2%–3% of gallstone ileus, which itself represents 1%–4% of all small bowel obstructions, highlighting its rarity [2–4]. The syndrome is prevalent in elderly women with a female-to-male ratio of 1:9, carrying significant morbidity and mortality (12%) [5].
Nonspecific clinical symptoms often result in delayed diagnosis, with patients displaying signs of gastric outlet obstruction. Hematemesis (15%) and melena (6%) further complicate the diagnosis, resembling malignant obstruction [6].
Diagnosis relies on the clinical presentation and the identification of Rigler’s triad (observed in 14.8%–21% of cases) through imaging. This triad comprises a distended stomach, pneumobilia, and a radiopaque shadow suggestive of an enteric gallstone. Subsequently, Rigler’s pentad was introduced, incorporating a ‘tumbling stone’ and the presence of two air-fluid levels in the right upper quadrant (24%) [6]. A CT scan is the preferred investigation due to its high specificity (100%) and accuracy (99%). MRCP is an adjunct providing specific details about the hepatobiliary tree, fistulous tract, and concretions. Upper gastrointestinal series and abdominal ultrasound are alternatives in resource-limited settings [2, 4–6].
Upper GI endoscopy serves both diagnostic and therapeutic purposes, revealing obstruction (69%), stones (31%), and fistulas (13%). Despite enthusiasm for endoscopic stone extraction (10%), high failure rates (42%) are associated with larger stones (>2.5 cm) [7]. Surgical interventions encompass open enterolithotomy or gastrotomy, with or without concomitant cholecystectomy and fistula repair. The decision between a ‘single’ or ‘two’ stage approach remains unsettled. Advocates of one-stage repair stress the importance of preventing potential biliary complications, like cholecystitis, cholangitis, and gallbladder carcinoma. Conversely, proponents of two-stage repair highlight the possibility of spontaneous closure of the fistula in patients with a patent cystic duct and an empty gallbladder [8]. We advocate tailored treatment options for individual patients based on factors, such as age, comorbidities, and the surgical expertise of the operator. While open surgical procedures (91%) have a high success rate, laparoscopic management is feasible for low-risk patients [7, 8].
In conclusion, BS poses a surgical challenge due to nonspecific symptoms, complex diagnostic approaches, and varying therapeutic strategies tailored to individual patient factors.
Acknowledgements
I declare that this manuscript has been composed solely by us and that it has not been submitted, in whole or in part, to any journal.
Author contributions
All authors contributed to the study conception and design, material preparation, data collection, analysis, drafting and final approval.
Conflict of interest statement
None declared.
Data availability
All the data pertaining to the patient is available with the corresponding author and would be made available if necessary.



