-
PDF
- Split View
-
Views
-
Cite
Cite
Junjie Zhou, Hongbin Zhang, Qianming Xiang, Fabiao Dong, Luyun Sun, Heterotopic pancreas in Meckel’s diverticulum causing perforation in an infant: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae375, https://doi.org/10.1093/jscr/rjae375
Close - Share Icon Share
Abstract
Perforation of Meckel’s diverticulum caused by heterotopic pancreas is a rare condition. Despite recent improvements in imaging studies, Meckel”'s diverticulitis and heterotopic pancreas are difficult to diagnose preoperatively and are often diagnosed during autopsy or laparotomy. Symptomatic patients are typically >1 year, and cases of infants displaying symptoms are rarely reported. We report a rare case of heterotopic pancreas in Meckel’s diverticulum causing perforation in an infant. In cases of infants presenting with unexplained acute abdominal pain, there should be a high index of suspicion for congenital gastrointestinal malformations. Prompt action in the form of exploratory laparotomy or laparoscopy is crucial to prevent the escalation of complications and to definitively confirm the diagnosis.
Introduction
Heterotopic pancreas (HP) is defined as pancreatic tissue without anatomical or vascular connection to the pancreas. The true incidence of HP remains uncertain due to its asymptomatic nature in most patients, often discovered incidentally during autopsy [1]. HP can manifest throughout the gastrointestinal tract and other organs. The most commonly reported locations include the stomach (25.5%), duodenum (27.7%), proximal jejunum (15.9%), Meckel’s diverticulum (MD) (5.3%), and ileum (2.8%) [2].
MD stands out as the most prevalent congenital anomaly within the digestive system. It occurs in ~2% to 3% of the general population [3]. The lining of this diverticulum predominantly comprises ectopic gastric mucosa. However, in a minority of instances, ~6% of all MD cases, pancreatic tissue may also be present [4].
In extensive studies, ~85% of patients with HP exhibit no symptoms, with lesions often incidentally identified during procedures conducted for other indications [5]. Pediatric series present varying findings, with some authors indicating symptomatic cases in 8% of instances,while others report symptoms in >60% of patients with HP [5, 6]. However, symptomatic patients are typically older than one year, and cases of infants displaying symptoms are rarely reported [1]. The imaging features of HP and MD lacks specificity. It’s difficult to diagnose preoperatively and are often diagnosed after laparotomy. Here, we report a rare case of heterotopic pancreas in MD causing perforation in an infant with coexisting chronic appendicitis.
Case report
A 7-month-old male infant was admitted to our hospital presenting with persistent crying and fever over the past 2 days. The maximum recorded temperature was 39.5°C. Two days prior, the patient received medical attention at another hospital’s outpatient department, where X-ray and ultrasound examinations were performed, both yielding reports of no abnormalities. Despite receiving anti-inflammatory treatment, the patient’s condition did not improve, prompting further evaluation and treatment in our department.
After admission,the patient underwent a physical examination revealed abdominal distension accompanied by tenderness and localized guarding in the right lower quadrant. Abdominal X-ray revealed partial small intestinal pneumatosis expansion in the left middle upper abdomen and right middle lower abdomen, alongside multiple air-fluid levels, suggestive of a potential ileus (Fig. 1). Laboratory tests showed a white blood cell count of 3.99 × 109/L and a C-reactive protein level of 154.33 mg/L.
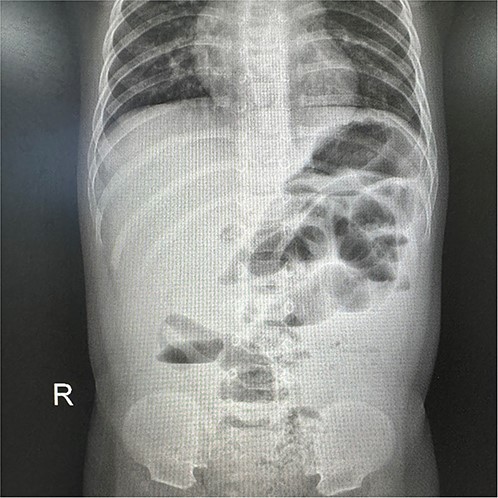
X-ray revealed partial small intestinal pneumatosis expansion alongside multiple air-fluid levels.
Following admission, the patient underwent a regimen of treatments comprising fasting, gastrointestinal decompression, and anti-inflammatory therapy. CT scan of the abdomen revealed suspicion of slight expansion with gas and fluid accumulation in some loops of the small bowel, accompanied by a small amount of intra-abdominal fluid.
After 48 hours of treatment, the patient continued to exhibit recurrent fever, ongoing infection, and localized peritoneal irritation, prompting the initiation of an emergent exploratory laparotomy. Upon initiation of the procedure, a significant volume of turbid pus was observed to discharge from the abdominal cavity. A perforated MD was identified ~30 cm proximal to the ileocecal valve. The base of the diverticulum was stenosed and connected to the cavity by a long pedicle, with a perforation noted at the apex (Fig. 2). Subsequently, diverticulectomy and repair of the bowel wall were performed. Examination of the appendix revealed pus accumulations on the serosal surface, accompanied by mild inflammation, leading to its resection.

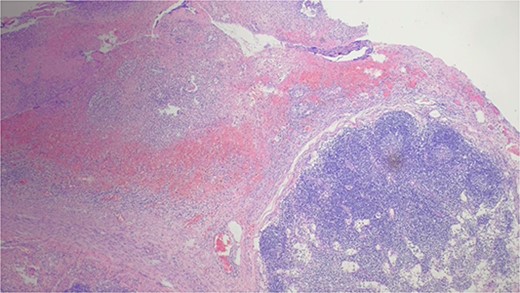
The patient commenced oral intake three days following the operation and was discharged seven days later. The postoperative pathology report indicated chronic diverticulitis with ectopic pancreatic mucosa and chronic appendicitis (Figs 3 and 4).
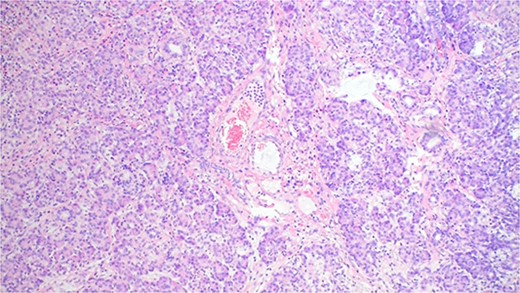
The pathology result of chronic diverticulitis with ectopic pancreatic mucosa.
Discussion
MD typically presents asymptomatically. Nonetheless, it carries an estimated lifetime risk of 4–6% for symptom development, including manifestations such as bleeding, intussusception, inflammation, and perforation. The most common age at presentation is 2 years [7]. A review reported perforation rate of symptomatic MD is ~0.5% [8]. While perforation caused by ectopic pancreas is extremely rare in infants.
The etiology of heterotopic pancreas within MD remains unclear. It is postulated that heterotopic pancreatic tissue arises embryonically through either the rotation of the foregut and subsequent fusion of the dorsal and ventral pancreatic buds, or through pancreatic metaplasia of endodermal tissue. The primary presentations of HP include hemorrhage and intussusception in pediatric patients, with documented cases of malignant transformation [9]. Chemical stimulation and inflammation within pancreas tissue can induce the destruction of mucosa. Pancreatic enzymes, including elastase, may contribute to the corrosion and thinning of vessel walls, ultimately leading to chronic inflammation and eventual perforation.
HP is usually not evident at clinical or imaging examination; rather, it is discernable at microscopic analysis. As observed in our case, HP still need to be confirmed by pathological examination [10]. Their sensitivity and specificity of CT and MIR to diagnose MD are often low. These modalities may reveal findings suggestive of small-bowel obstruction and intussusception. Distinguishing MD from adjacent small intestine loops can be challenging [7, 11]. Previous small sample pilot studies suggested the possibility and advantage of capsule endoscopy in identifying bleeding MD when conventional modalities failed to detect any lesion [12, 13]. A recent study even proposed the possibility of treatment under double balloon enteroscopy, such as argon plasma coagulation, balloon dilatation, polypectomy, but more evidence is needed [14].
Surgical resection for symptomatic MD has garnered consensus. In children with asymptomatic MD, early surgical intervention is advocated based on retrospective multicenter studies, aiming to preempt the development of associated complications in later stages [15]. This case offers valuable insights for clinical physicians, particularly when encountering similar clinical presentations in children under 2 years old. When imaging examinations fail to provide a conclusive diagnosis, it becomes crucial to consider the possibility of perforation in MD.
Conclusion
Heterotopic pancreas within MD leading to perforation in infants represents an exceedingly rare condition, often posing diagnostic challenges prior to surgical intervention. In cases of infants presenting with unexplained acute abdominal pain, there should be a high index of suspicion for congenital gastrointestinal malformations. Prompt action in the form of exploratory laparotomy or laparoscopy is crucial to prevent the escalation of complications and to definitively confirm the diagnosis.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Patient consent
Informed consent was obtained from the patient’s parents.
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Kunming Medical University.
Informed consent
Informed consent was obtained from the patient’s parents.



