-
PDF
- Split View
-
Views
-
Cite
Cite
Ioannis Delniotis, Benedikt Leidinger, Fixation of a chondral lateral femoral condyle fracture in a 13-year-old boy following patella dislocation using a new suture technique, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae367, https://doi.org/10.1093/jscr/rjae367
Close - Share Icon Share
Abstract
Osteochondral or, even more rarely, purely chondral fractures of the lateral femoral condyle following patella dislocation in adolescents are relatively infrequent. Various fixation methods are described in the literature, ranging from traditional screws to bioabsorbable constructs or the use of anchors. Each method possesses its own advantages and limitations. Here, we present a case involving a 13-year-old boy with a large purely chondral fracture of the lateral femoral condyle after patella dislocation, initially overlooked. We introduce a cost-effective suture-bridge technique for the fixation of this fracture, which eliminates the need for a second operation and has yielded favorable outcomes. It is important to know that fractures of this type can be easily overlooked, necessitating a high index of suspicion and the utilization of advanced imaging techniques to prevent potential long-term catastrophic outcomes for the knee joint.
Introduction
Patella dislocation is extensively documented in the literature as a prevalent occurrence among adolescents; however, osteochondral fractures of the lateral femoral condyle subsequent to patella dislocation are relatively uncommon [1, 2]. Numerous studies have outlined diverse treatment approaches, including excision, fragment fixation with screws, fixation utilizing bioabsorbable pins, anchors and various suture techniques [2–4].
In this report, we present a case detailing the management of a large, purely chondral fracture of the lateral femoral condyle following patella dislocation in a 13-year-old adolescent. Our approach involved the utilization of an innovative suture technique.
Case report
A healthy 13-year-old boy presented to our facility 2 weeks following knee injury with suspected patella dislocation. The patient reported falling in his home’s bathroom 2 weeks prior and subsequently sought medical attention the following morning at a local hospital due to knee effusion and pain.
At the local hospital, the patient underwent X-ray examination of the affected knee and was subsequently immobilized with an above knee cast. The X-rays yielded normal results (Fig. 1). Instructions were provided to restrict weight-bearing, and a follow-up examination was scheduled in 10 days. However, the family presented to our facility, instead.

(A + B) Antero-posterior and lateral X-ray examination of the injured knee. Radiological examination shows no fracture.
The cast was removed, and the patient underwent thorough examination. A considerable amount of knee effusion was observed, accompanied by pain localized to the lateral femoral condyle. Ultrasound evaluation of the knee joint identified a potential osteochondral fracture in the suprapatellar pouch (Fig. 2A). Subsequently, an MRI examination was promptly conducted, confirming the presence of an (osteo)chondral fragment of the lateral femoral condyle, measuring 2.4 × 1.35 cm2, subsequent to patella dislocation (Fig. 2).
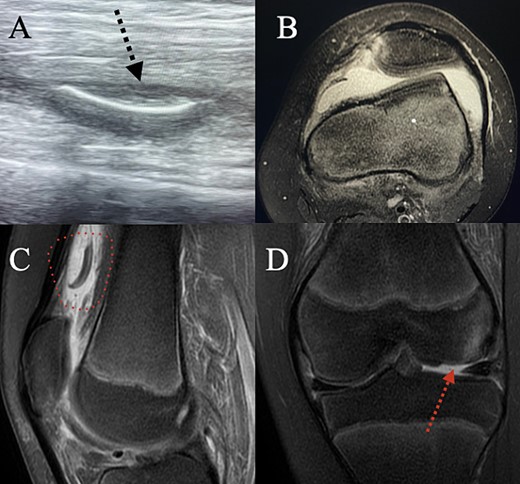
(A) Ultrasound examination of the supra-patellar pouch revealed a possible chondral fragment floating there. (B) Axial MRI showing lateralization of the patella, trochlea dysplasia and a torn MPFL. (C) Sagittal MRI confirming that there is a chondral fragment in the supra-patellar pouch. (D) Coronal MRI showing the chondral fracture in the lateral femoral condyle.
Surgery was scheduled to address the osteochondral fragment. Under general anesthesia and with the application of a tourniquet, a midline incision to the knee joint was performed. The fragment, situated 2,5 cm above the patella, was identified and detached from the surrounding tissues. Comprising solely articular cartilage, the fragment exhibited no attachment to subchondral bone (Fig. 3B). Subsequent to trimming and freshening of both the chondral fragment and the defect due to a partial mismatch in size, the defect bed was prepared for fixation by drilling with a 2-mm Kirschner wire to facilitate healing.
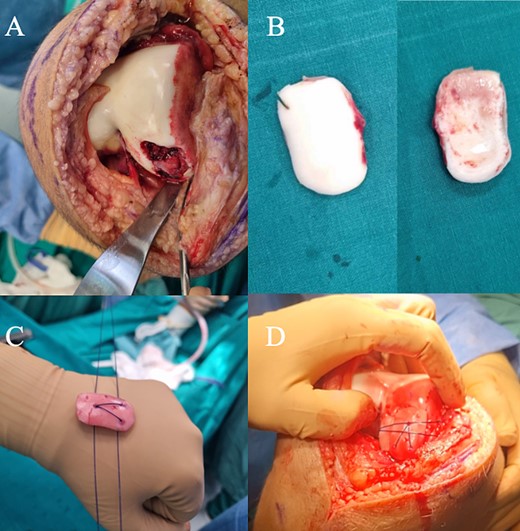
(A) Intra-operative image of the chondral fracture in the lateral femoral condyle. (B) The chondral fragment that was retrieved from the supra-patellar pouch. The fragment exhibited no attachment to subchondral bone. (C) The suture passage on the chondral fragment is created in a triangle fashion. The small holes visible are a result of attempts to suture the edges and to stabilize the fragment with various types of bioabsorbable constructs, all of which failed to stabilize the fragment. (D) Intra-operative view of the suture-bridge technique described in the article, which provides strong compression and stabilization of the fragment.
Two absorbable, no 0, PDS-Ethicon sutures were employed in the procedure. A triangular shape was fashioned in the chondral fragment using the sutures’ needles. One suture was passed from the apex of the triangle to the medial aspect, while the other suture traversed from the same point but directed towards the lateral aspect of the triangle (Fig. 3C).
Three bone tunnels were created utilizing a small drill: one directed towards the medial aspect of the lateral femoral condyle and two towards the lateral aspect. The sutures from the medial side were carefully passed through the (medial) bone tunnel using a suture passer, and then tightly advanced over the fragment toward the lateral side of the femoral condyle, with a slight divergent inclination to ensure optimal compression the fragment.
From the lateral suture, the upper portion was traversed through the upper (lateral) bone tunnel while the lower portion was directed through the lower (lateral) bone tunnel. The upper segment of the ‘medial’ suture was securely fastened to the upper portion of the ‘lateral’ suture, followed by a similar procedure for the lower portions of both the medial and lateral sutures (Fig. 3D).
Postoperatively, no weight-bearing was permitted for 6 weeks, followed by two additional weeks of partial weight-bearing. The knee was immobilized in extension for the initial 2 weeks, after which knee flexion up to 60° was permitted during weeks 2–4, and up to 90° during weeks 4–6. Subsequently, knee flexion was encouraged. The postoperative rehabilitation program was overseen by a physiotherapist to ensure adherence and proper progression. Four months post-surgery, MRI examination revealed complete healing, despite minor subchondral abnormalities (Fig. 4). The patient was able to walk independently without experiencing pain; however, a mild flexion deficit of 25 degrees was present, which will be monitored for improvement.
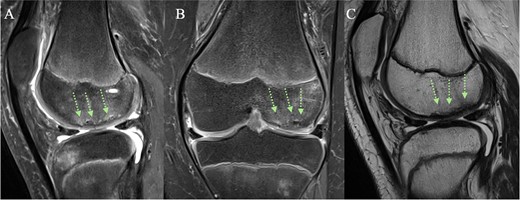
(A + C) Sagittal and (B) coronal MRI views 4 months post-operatively. The arrows indicate healing of the chondral fracture, although some minor subchondral abnormalities are present.
Discussion
Osteochondral or chondral fractures of the lateral femoral condyle subsequent to patella dislocation are relatively infrequent, presenting challenges in both diagnosis and treatment. Particularly in instances of purely chondral fractures, as illustrated in our case report, a high index of suspicion is needed and advanced imaging modalities such as MRI are recommended to facilitate accurate diagnosis. The failure to identify such fractures may lead to potentially catastrophic long-term consequences for the knee joint.
Osteochondral fragment fixation can be achieved using either traditional (headless or not) screws [5] or a diverse array of bioabsorbable implants, including pins, meniscal arrows/darts and anchors [6]. Metal screw fixation offers advantages such as compression and the rotational stability of the fracture, albeit at the expense of necessitating a secondary procedure for screw removal and potentially impending MRI interpretation. Conversely, bioabsorbable devices circumvent these drawbacks but may lack adequate compression [7].
Additionally, reports have indicated potential issues with allergic reactions and rapid absorption [7, 8].
In accordance with our findings, there are a limited numbers of similar reports in the literature. Cavalheiro et al. presented a case report describing the management of an osteochondral fracture of the lateral femoral condyle following patella dislocation, which was treated with transosseous sutures and fibrin glue, resulting in excellent outcomes at a 16-month follow-up [9]. Additionally, Bowers et al. reported on two patients with femoral condyle fragments who were treated using absorbable sutures and bone tunnels, concluding that the suture bridge technique represents a viable alternative to other established methods of fixation [10]. A suture bridge fixation technique is also described by Wu et al. in a case report detailing an osteochondral fracture of the lateral femoral condyle, with the distinction that anchors were utilized. Once again, satisfactory functional outcomes were observed at an 18-month follow-up [11].
Managing patella dislocation with reconstruction of the MPFL (medial patellofemoral ligament) can be performed simultaneously in the same surgical stage. However, in our patient, due to the co-existence of trochlea dysplasia, we preferred to postpone the management of patella dislocation to a second staged operation, as it would involve too many procedures for a single surgery.
Chondral fractures of the lateral femoral condyle subsequent to patella dislocation are infrequent. Here, we present a novel surgical technique yielding favorable outcomes while obviating the necessity for a secondary procedure for implant removal.
Conflict of interest statement
None declared.
Funding
None.



