-
PDF
- Split View
-
Views
-
Cite
Cite
Marco Gramellini, Folco Solimene, Moritz Menz, Lorenz Hinterleitner, Stefan Breitenstein, Patryk Kambakamba, Cecal volvolus herniation through the Winslow Foramen: a case report and literature review of surgical management, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae325, https://doi.org/10.1093/jscr/rjae325
Close - Share Icon Share
Abstract
Both cecal volvolus and Winslow hernia are rare clinical presentations accounting for 1–1.5 and 0.08% of bowel obstructions. The combination of the two phenomena has been described so far in 13 case reports. Our patient underwent laparotomy with lesser Sac opening, manual hernia reduction, right hemicolectomy and partial Foramen closure with two simple stitches of PDS 4.0. Due to the scarcity of literature guidelines are not available, the intraoperative state of the tissues and the likelihood of a hernia recurrence play a decisive role in surgical management.
Introduction
A cecal volvolus (CV) is a twisting or axial rotation of the cecum and accounts for 1–1.5% of all intestinal obstructions [1]. Even rarer are internal hernias, also accounting for only 1% of Bowel Obstructions. The Foramen of Winslow Hernia (FWH) accounts for 8% of internal Hernias and the cecum is the herniated organ only in one-third of the cases [2]. Both clinical presentations are associated with a mortality rates up to 30 and 49%, respectively if not promptly recognized and treated [3, 4]. The combination of CV and FWH is an extremely rare Phenomenon and has to our knowledge been reported only 13 times in the literature. An excessive viscera mobility with persisting ascending mesocolon, a Winslow Foramen (WF) of more than 3 cm and changes in intra-abdominal pressure are the advocated pathological mechanisms [4]. Data regarding its management are scarce and no guidelines are available. In this case report, we describe our procedure and we compare it with the surgical management in the other reported cases.
Case report
A 68-year-old woman presented in the emergency department of our hospital with epigastric pain irradiated to the back without vomiting or fever. Past clinical history included Hashimoto Thyroiditis and Polycitaemia Vera, with no previous surgical operations. The clinical examination showed a soft abdomen but with bloating, defence reaction and abdominal pain in epigastrium. Blood testing revealed 9.96 G/L leucocytes and 1 mg/l C-reactive protein. We performed a computer tomography (CT) of the abdomen, which identified a retrogastric volvulated cecum (Fig. 1B and C) and the indication to surgery was given.
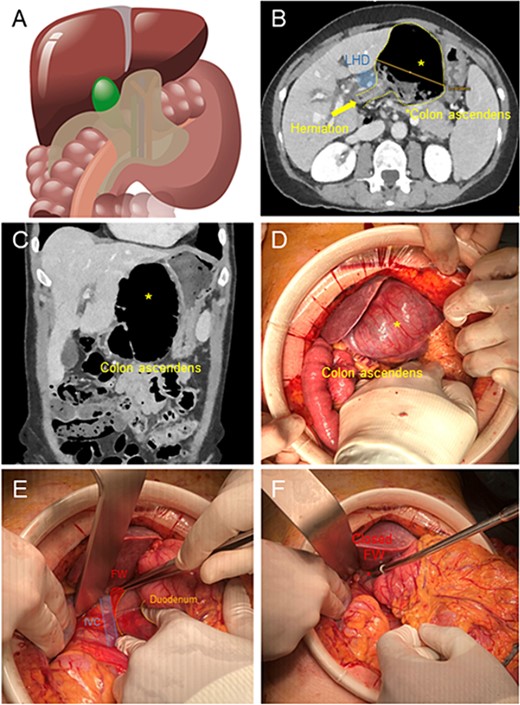
(A) Illustration of cecal herniation through WF as shown in CT scan. (B) Dilated colon ascendens behind the Ligamentum Hepatoduodenale (LHD) in the CT Scan. (C) The coronary view shows the dilated colon. (D) Intraoperative hernia presentation after laparotomy, the dilated colon presents a serosal tear (*) in its surface. (E) After reduction of hernia, exposure of WF, with inferior vena cava below and Duodenum to the right. (F) Closure of WF with interrupted suture with p-Dioxanon (PDS 4-0).
We performed a 12-cm laparotomy, which allowed us to confirm the diagnosis (Fig. 1D). We incised the thin lesser sac, performed a manual derotation of the cecum and cautiously successfully pulled laterally the herniated viscera through the WF (Fig. 1E). The cecum appeared massively dilated with serosal tears. The whole ascending colon appeared lax and hypermobile. Therefore we performed a right hemicolectomy with a stapled side-to-side ileo-colic anastomosis and mesenterial closure. To prevent the recurrence of visceral herniation through the WF, we applied two simple stitches in PDS 4.0 in the inferior portion of the WF aiming to restore its normal diameter (Fig. 1F).
Further postoperative course was uneventful and the patient was discharged on the fifth POD. At 1-year follow-up, the patient hasn’t shown any evidence of hernia recurrence and is feeling well.
Discussion
The combination of FWH and CV is an extremely rare clinical presentation. 12 case reports in English language are reported on Pubmed. Their features as well as that of our case are summarized in Table 1. Out of 13, 12 are female patients, age range: 55–82 years. These findings are coherent with literature as CV is more common in females in this age range [5], although FWH appears to be predominant in males [4]. Typical presentations include abdominal pain with or without vomiting and bloating in the upper abdominal quadrants. CT was the preferred imaging, able to identify the bloated ectopic cecum in the lesser sac and the possible twist of the ileocolic vessels. In the case of Lawson et al. [6] ischemic changes in the liver due to the complete occlusion of the portal vein were also reported, highlighting how a bloated bowel loop herniated through FWH can as well impact the hepato-duodenal Ligament’s structures.
| . | Clinical presentation features . | Surgical management . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| . | Male/female . | Patient age (y) . | Symptoms . | Lab tests . | Laparotomy . | Lesser sac incision . | Hernia reduction . | Bowel resection . | Foramen closure . |
| Morioka et al. 1970 [14] | F | 67 | Abdominal pain | yes | no | yes | no | no | |
| Ray et al 2009 [15] | F | 55 | Abdominal pain Vomiting | unremarkable | yes | no | yes, manual | yes | yes with omental flap |
| Makarawo et al 2014 [12] | F | 75 | Abdominal pain Vomiting | unremarkable | yes | yes | yes, manual | no, cecopexy | yes with omental flap |
| Kamyab et al. 2016 [10] | F | 67 | Upper abdominal pain Nausea Vomiting | yes | no | yes, through Kocher Maneuver | yes | no | |
| Nguyen et al. 2017 [7] | F | 73 | Abdominal pain Nausea Vomiting | slightly elevated WBC | yes | yes | yes, through cecal enterotomy | yes | no |
| Patel et al. 2017 [11] | M | 62 | Upper abdominal pain | WBC 15 G/l CRP 300 mg/l | yes | yes + diverting Ileostomy | |||
| Lawson et al. 2017 [6] | F | 56 | Upper abdominal Pain | unremarkable | yes | no | yes, manual | yes | no |
| Cho et al. 2019 [8] | F | 56 | Abdominal pain Nausea Vomiting | WBC 35,8 x109; CRP 360 mg/l | yes | yes | yes, through cecal enterotomy and lysis of adhesions | yes | no |
| Williams et al. 2021 [13] | F | 63 | Upper abdominal pain | WBC 12,9 K/uL; | yes | no | yes, manual | no, cecopexy | yes with omental flap |
| Chandhrasekar et al. 2022 [9] | F | 82 | Abdominal pain Nausea Vomiting | unremarkable | yes | yes | yes, through Kocher Maneuver and cecal enterotomy | yes | yes with omental flap |
| Carpenter et al. 2022 [2] | F | 70 | Abdominal pain Nausea Vomiting | WBC 16.6/mm3 | yes | yes | no, the resection was performed before reduction | yes | yes, complete closure with Vicryl stitches + omental flap |
| Perabo et al. 2022 [1] | F | 56 | Lower abdominal pain Nausea | yes | no | yes, manual | yes | no | |
| Our case | F | 68 | Upper abdominal pain | WBC 9,96 G/L; CRP 1 mg/ml | yes | yes | yes, manual | yes | yes, partial with PDS 4.0 stitches |
| . | Clinical presentation features . | Surgical management . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| . | Male/female . | Patient age (y) . | Symptoms . | Lab tests . | Laparotomy . | Lesser sac incision . | Hernia reduction . | Bowel resection . | Foramen closure . |
| Morioka et al. 1970 [14] | F | 67 | Abdominal pain | yes | no | yes | no | no | |
| Ray et al 2009 [15] | F | 55 | Abdominal pain Vomiting | unremarkable | yes | no | yes, manual | yes | yes with omental flap |
| Makarawo et al 2014 [12] | F | 75 | Abdominal pain Vomiting | unremarkable | yes | yes | yes, manual | no, cecopexy | yes with omental flap |
| Kamyab et al. 2016 [10] | F | 67 | Upper abdominal pain Nausea Vomiting | yes | no | yes, through Kocher Maneuver | yes | no | |
| Nguyen et al. 2017 [7] | F | 73 | Abdominal pain Nausea Vomiting | slightly elevated WBC | yes | yes | yes, through cecal enterotomy | yes | no |
| Patel et al. 2017 [11] | M | 62 | Upper abdominal pain | WBC 15 G/l CRP 300 mg/l | yes | yes + diverting Ileostomy | |||
| Lawson et al. 2017 [6] | F | 56 | Upper abdominal Pain | unremarkable | yes | no | yes, manual | yes | no |
| Cho et al. 2019 [8] | F | 56 | Abdominal pain Nausea Vomiting | WBC 35,8 x109; CRP 360 mg/l | yes | yes | yes, through cecal enterotomy and lysis of adhesions | yes | no |
| Williams et al. 2021 [13] | F | 63 | Upper abdominal pain | WBC 12,9 K/uL; | yes | no | yes, manual | no, cecopexy | yes with omental flap |
| Chandhrasekar et al. 2022 [9] | F | 82 | Abdominal pain Nausea Vomiting | unremarkable | yes | yes | yes, through Kocher Maneuver and cecal enterotomy | yes | yes with omental flap |
| Carpenter et al. 2022 [2] | F | 70 | Abdominal pain Nausea Vomiting | WBC 16.6/mm3 | yes | yes | no, the resection was performed before reduction | yes | yes, complete closure with Vicryl stitches + omental flap |
| Perabo et al. 2022 [1] | F | 56 | Lower abdominal pain Nausea | yes | no | yes, manual | yes | no | |
| Our case | F | 68 | Upper abdominal pain | WBC 9,96 G/L; CRP 1 mg/ml | yes | yes | yes, manual | yes | yes, partial with PDS 4.0 stitches |
| . | Clinical presentation features . | Surgical management . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| . | Male/female . | Patient age (y) . | Symptoms . | Lab tests . | Laparotomy . | Lesser sac incision . | Hernia reduction . | Bowel resection . | Foramen closure . |
| Morioka et al. 1970 [14] | F | 67 | Abdominal pain | yes | no | yes | no | no | |
| Ray et al 2009 [15] | F | 55 | Abdominal pain Vomiting | unremarkable | yes | no | yes, manual | yes | yes with omental flap |
| Makarawo et al 2014 [12] | F | 75 | Abdominal pain Vomiting | unremarkable | yes | yes | yes, manual | no, cecopexy | yes with omental flap |
| Kamyab et al. 2016 [10] | F | 67 | Upper abdominal pain Nausea Vomiting | yes | no | yes, through Kocher Maneuver | yes | no | |
| Nguyen et al. 2017 [7] | F | 73 | Abdominal pain Nausea Vomiting | slightly elevated WBC | yes | yes | yes, through cecal enterotomy | yes | no |
| Patel et al. 2017 [11] | M | 62 | Upper abdominal pain | WBC 15 G/l CRP 300 mg/l | yes | yes + diverting Ileostomy | |||
| Lawson et al. 2017 [6] | F | 56 | Upper abdominal Pain | unremarkable | yes | no | yes, manual | yes | no |
| Cho et al. 2019 [8] | F | 56 | Abdominal pain Nausea Vomiting | WBC 35,8 x109; CRP 360 mg/l | yes | yes | yes, through cecal enterotomy and lysis of adhesions | yes | no |
| Williams et al. 2021 [13] | F | 63 | Upper abdominal pain | WBC 12,9 K/uL; | yes | no | yes, manual | no, cecopexy | yes with omental flap |
| Chandhrasekar et al. 2022 [9] | F | 82 | Abdominal pain Nausea Vomiting | unremarkable | yes | yes | yes, through Kocher Maneuver and cecal enterotomy | yes | yes with omental flap |
| Carpenter et al. 2022 [2] | F | 70 | Abdominal pain Nausea Vomiting | WBC 16.6/mm3 | yes | yes | no, the resection was performed before reduction | yes | yes, complete closure with Vicryl stitches + omental flap |
| Perabo et al. 2022 [1] | F | 56 | Lower abdominal pain Nausea | yes | no | yes, manual | yes | no | |
| Our case | F | 68 | Upper abdominal pain | WBC 9,96 G/L; CRP 1 mg/ml | yes | yes | yes, manual | yes | yes, partial with PDS 4.0 stitches |
| . | Clinical presentation features . | Surgical management . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| . | Male/female . | Patient age (y) . | Symptoms . | Lab tests . | Laparotomy . | Lesser sac incision . | Hernia reduction . | Bowel resection . | Foramen closure . |
| Morioka et al. 1970 [14] | F | 67 | Abdominal pain | yes | no | yes | no | no | |
| Ray et al 2009 [15] | F | 55 | Abdominal pain Vomiting | unremarkable | yes | no | yes, manual | yes | yes with omental flap |
| Makarawo et al 2014 [12] | F | 75 | Abdominal pain Vomiting | unremarkable | yes | yes | yes, manual | no, cecopexy | yes with omental flap |
| Kamyab et al. 2016 [10] | F | 67 | Upper abdominal pain Nausea Vomiting | yes | no | yes, through Kocher Maneuver | yes | no | |
| Nguyen et al. 2017 [7] | F | 73 | Abdominal pain Nausea Vomiting | slightly elevated WBC | yes | yes | yes, through cecal enterotomy | yes | no |
| Patel et al. 2017 [11] | M | 62 | Upper abdominal pain | WBC 15 G/l CRP 300 mg/l | yes | yes + diverting Ileostomy | |||
| Lawson et al. 2017 [6] | F | 56 | Upper abdominal Pain | unremarkable | yes | no | yes, manual | yes | no |
| Cho et al. 2019 [8] | F | 56 | Abdominal pain Nausea Vomiting | WBC 35,8 x109; CRP 360 mg/l | yes | yes | yes, through cecal enterotomy and lysis of adhesions | yes | no |
| Williams et al. 2021 [13] | F | 63 | Upper abdominal pain | WBC 12,9 K/uL; | yes | no | yes, manual | no, cecopexy | yes with omental flap |
| Chandhrasekar et al. 2022 [9] | F | 82 | Abdominal pain Nausea Vomiting | unremarkable | yes | yes | yes, through Kocher Maneuver and cecal enterotomy | yes | yes with omental flap |
| Carpenter et al. 2022 [2] | F | 70 | Abdominal pain Nausea Vomiting | WBC 16.6/mm3 | yes | yes | no, the resection was performed before reduction | yes | yes, complete closure with Vicryl stitches + omental flap |
| Perabo et al. 2022 [1] | F | 56 | Lower abdominal pain Nausea | yes | no | yes, manual | yes | no | |
| Our case | F | 68 | Upper abdominal pain | WBC 9,96 G/L; CRP 1 mg/ml | yes | yes | yes, manual | yes | yes, partial with PDS 4.0 stitches |
In all cases, a straightforward laparotomy was performed due to the potential ischemic risk of the overly distended bowel suffering from both volvulation and incarceration. In 2019, Moris et al. [4] reported a series of 15 FWH of different organs (ileum, colon, gallbladder) successfully achieving a laparoscopic hernia reduction and, among them, only two cases required a bowel resection. However, we deem the applicability of laparoscopy in case of a volvulated organ through the WF limited, due to a more evident bowel distension hindering repositioning. Furthermore, a failed reposition implies a subsequent laparotomy with possible advanced necrotic state of the bowel due to the time delay.
The reduction of the hernia was achieved in 11 cases out of 12 (in 1 case not mentioned) and, in 6 cases, required the incision of the hepato-gastric ligament to perform a manual derotation of the bowel (such as in our case) or a cecal enterotomy to release the bowel content and reduce the swelling [7–9]. Kocher Manouver was also performed in two cases [9, 10]. In the case of Carpenter et al. [2], the bowel could not be reduced and right hemicolectomy was directly performed.
A right hemicolectomy was performed in 10 cases out of 13 to remove the ischemic pre-perforated cecum. Patel et al. [11] report the only case with a perforated cecum at diagnosis and in this case a diverting ileostomy was performed and at a later date reversed. Makarawo et al. and Williams et al. [12, 13] report two cases of cecal bascule, where the Cecum folds on itself rather than twisting on its vascular axis and resulting in ischemia. The resection could be spared and a cecopexy was performed to reduce the gut mobility and prevent the recurrence of CV.
Foramen closure as a prevention maneuver was performed in 6 cases out of 12 (in one case it is not mentioned) and was except in our case always performed with an omental flap. We preferred a partial closure with simple stitches to restore the standard anatomy. In the review of D. Moris [4] among the 15 operated patients, due to FWH, only 5 underwent a foramen closure but none of them experienced an FWH recurrence in a median follow-up of 3 months. No evidence so far demonstrates foramen closure results in decreased FWH recurrence, nor a preferable closure method (omental flap vs stitches).
Further evidence is required to establish guidelines for surgical management of this uncommon presentation. The status of the cecum and the likelihood of recurrence should guide the surgeon in the intraoperative decision making.
Conflict of interest statement
None declared.
Funding
None declared.



